Manuscript accepted on :16-Mar-2019
Published online on: 23-03-2019
Plagiarism Check: Yes
Reviewed by: Md. Sahab Uddin
Second Review by: Prof Dr. M Zak Khalil
Mahadewa Tjokorda G. B.
Department of Neurosurgery, Fakulty of Medicine, Universitas Udayana / Sanglah Hospital- Bali-Indonesia.
Corresponding Author E-mail: tjokmahadewa@unud.ac.id
DOI : https://dx.doi.org/10.13005/bpj/1663
Abstract
To investigate clinical improvements and histologic studies of patients with symptomatic lumbar hypertrophic of flavum ligament (HFL) associated with neurogenic claudication. There were 32 subjects (18 males and 14 females) included in the study with the mean age of 46 years old (range 32 to 64). Patients functionality is measured by Neurogenic Claudication Outcome Score (NCOS). All patients were treated previously in a rehabilitation unit for four weeks and indicated for surgery due to neurogenic claudication (excluding those without neurological deficit). Imaging modalities were taken preoperatively (plain spine x-ray, computed tomography (CT) scan, magnetic resonance imaging (MRI) and postoperatively (plain x-ray at day 3 and two months later, CT scan after eight weeks). Histological studies were also taken, as well as the NCOS for evaluating the claudication. A student’s t-test analysis was carried out on the NCOS pre- and postoperative to evaluate the improvement significance. The improvement of the NCOS score in male was 23.1±2.23 and female was 24.85±2.68 (p=0.023). Histologically, the flavum ligament was hardening, stiffening, and calcifying resulting in a decrease in the ratio of elastin to fibrous tissue, leading to the hypertrophic process. In the short term, surgical results improved in all patients with no surgical complication. Surgical decompression can yield a better outcome in the short term for treating symptomatic lumbar HFL associated with neurogenic claudication. This early pathological process in the flavum ligament results in an overall tissue thickening leading to narrowing of the lumbar canal.
Keywords
Hypertrophy of Flavum Ligament; Neurogenic Claudication; Surgical Decompression
Download this article as:| Copy the following to cite this article: Mahadewa T. G. B. Symptomatic Lumbar Hypertrophy of Flavum Ligament Associated with Neurogenic Claudication. Biomed Pharmacol J 2019;12(1). |
| Copy the following to cite this URL: Mahadewa T. G. B. Symptomatic Lumbar Hypertrophy of Flavum Ligament Associated with Neurogenic Claudication. Biomed Pharmacol J 2019;12(1). Available from: https://bit.ly/2upUTyE |
Introduction
Stenosis due to degenerative processes in the lumbar canal may cause neurogenic claudication, lower back pain, and in severe stenosis cases, can affect the neurologic function. Laminectomy is the standard surgical management for patients with neurogenic claudication in lumbar canal stenosis. Canal stenosis is the resultant of facet hypertrophy, spur formation, thickening of flavum ligament, disc degeneration and herniation, and spondylolisthesis, all of which affect the canal diameter and the intervertebral foraminal. Symptoms include neurogenic claudication, back pain, neurological deficits including paresthesia, and autonomic disturbance. The narrowing of the canal, in part, results from hypertrophic of flavum ligament (HFL) and the mechanism of hypertrophy remains unclear.1,2
Previous reports indicated the importance of HFL in patients with spinal stenosis. Several studies have radiologically examined flavum ligament thickness and its association with age and lumbar levels in the early stages of degenerative cascade; examining the relationship of the inflammatory process with the occurrence of ligamentum flavum thickening and so on.1,3,4
Although the thickening of the flavum ligament from the radiological results is less significant, the patient’s neurological complaints and deficits are not so. Furthermore, there remains a lack of histological reports regarding fibrocartilagenous tissue underlying calcification or ossification of the flavum ligament in the early stage.
The current study emphasizes the clinical improvements and histologic studies in patients with symptomatic lumbar HFL associated with neurogenic claudication. This was an observational study on surgically treated patients based on medical records in Sanglah-General Hospital, Bali, Indonesia.
Material and Methods
There were 32 patients with lumbar stenosis who underwent laminectomy decompression stabilization fusion by the single author between January 2015 and May 2017. All patients were treated in a rehabilitation unit for four weeks and indicated for surgery due to neurogenic claudication that can not be manage by physical therapy or medication. The preoperative radiographic examination included plain spine x-ray, computed tomography (CT) scan and magnetic resonance (MRI) imaging. Patients with lumbar stenosis without neurological deficit were excluded, which were treated by conservative management.
All patients had paraparesis range from 2 to 4 in scale out of 5 for the manual muscle tests (MMT) and underwent posterior decompression, used the lumbar brace for a minimum of 2 months and continued to physical therapy for the next two months. Plain x-rays were obtained on day three post-surgery and after two months of follow up. A follow up CT scan was performed at eight weeks postoperatively and at least two months of follow-up was carried out in all patients (range 10-24 months). The neurologic status was recorded after two months of follow-up. The NCOS was utilized for the evaluation of claudication. This study had received a recommendation from the Ethics Committee on human research, Faculty of Medicine, Udayana University (No: 2436/UN.14.2/KEP/2017). Written consent was obtained from each subject after they understood the purpose and agreed to participate the study.
Statistical Analysis
In this study, data were evaluated using a student’s t-test analysis on the NCOS pre- and postoperative to evaluate the improvement significance. All analyses were performed with SPSS version 21. P-value of 0.05 was considered as statistically significant.
Results
The present study is comprised of 18 men and 14 women ranging from 32 to 64 years old (mean age is 46). Spinal MRI shows canal compromise due to HFL (Fig. 1A-B). Patients had neurological paraparesis as examined by NCOS. The mean preoperative NCOS for males was 40.7±1.8, 95% CI (39.76-41.45) and for females was 39.7±2.51, 95% CI (38.50-40.90). The mean postoperative NCOS for males 63.8±2.51, 95% CI (62.53-65.0) and for females was 64.57±1.22, 95% CI (63.87-65.27). The improvement of NCOS in males was 23.1±2.23, 95% CI (21.95-24.26) and females was 24.85±2.68, 95% CI (23.61-26.09). Pre-operative HFL thickness in males was 14,9±1.41, 95% CI (13,49-16,3) and females was 13.7±1.29, 95% CI (12.41-15,0) which were measured at the most stenotic level of the MRI images (Table 1). In the short term, surgical results improved in all patients. No infection leakage of cerebrospinal fluid nor implant failure was observed in this study. Postoperative lumbar x-rays were performed to show the area of laminectomy and instrumentation (Fig. 2).
 |
Figure 1: A-B. Spine MRI shows canal compromise due to HFL.
|
(A) Sagittal T2-weighted MRI shows hypertrophy of flavum ligament (HFL) from L1-S1 levels with additional disc bulging on L3-S1 causing narrow lumbar canal (B) Coronal MR-Myelogram shows significant lumbar canal stenosis at L3-S1 levels.
Table 1: Characteristic of Subjects.
| Characteristic | Cases (n=32) | 95% CIP |
| Sex | 0.22 | |
| Male, n(%) | 18 (56.25) – | |
| Female, n(%) | 14 (43.75) – | |
| Age, mean (range) | 46 (32-64) – 0.057 | |
| NCOS score pre-operative | ||
| Male, mean (SD) | 40.7(1.8) 39.76-41.45 | |
| Female, mean (SD) | 39.7(2.51) 38.50-40.90 0.079 |
|
| NCOS score post-operative | ||
| Male, mean (SD) | 63.8 (2.51) 62.53-65.00 |
|
| Female, mean (SD) | 64.57(1.2) 63.87-65.27 0.003 |
|
| Improvement of NCOS | ||
| Male, mean (SD) | 23.1 (2.23) 21.95-24.26 |
|
| Female, mean (SD) | 24.85(2.68) 23.61-26.09 0.023 |
|
| Pre-operative HFL thickness | ||
| Male, mean (SD) | 14,9 (1.41) 13,49-16,3 0.07 |
|
| Female, mean (SD) | 13.7 (1.29) 12.41-15,0 |
|
SD=standard deviation; NCOS=neurogenic claudicatio outcome score; CI = confidence interval; P= p value.
 |
Figure 2: Postoperative Lumbar x-ray showing area of laminectomy and instrumentation.
|
Postoperative plain Lumbar x-ray shows acceptable pedicle screws placement on L3-S1 levels with visible shadow of empty area after laminectomy from L3-S1 levels.
Histopathologic preparations of the patient’s flavum ligament included mineral deposits and cartilage growth suggesting an early pathological process in the flavum ligament that results in overall tissue thickening leading to lumbar canal stenosis. Hematoxylin-Eosin staining showed visible pieces of tissue containing solid connective tissue as well as areas comprising cartilage matrix and mineralized focus (x 400) (Fig. 3).
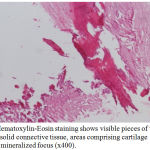 |
Figure 3: Hematoxylin-Eosin staining shows visible pieces of tissue containing solid connective tissue, areas comprising cartilage matrix and mineralized focus (x400).
|
Histopathologic preparations of the patient’s flavum ligament using Hematoxylin-Eosin staining shows mineral deposits and cartilage growth process in the flavum ligament that results in solid tissue
Verhoeff-van Gieson and Trichrome stains found more dominant fibrous tissue compared to elastin connective tissue in flavum ligament. This finds indicated that the elastic bands of the flavum ligament are undergoing hardening, stiffening, and calcification resulting to a decrease in the ratio of elastin tissue to fibrous tissue (Figs. 4A & B).
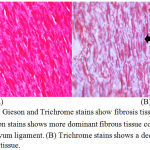 |
Figure 4: Verhoeff-van Gieson and Trichrome stains show fibrosis tissue and elastic fibers.
|
(A) Verhoeff-van Gieson stains shows more dominant fibrous tissue compared to elastin connective tissue in flavum ligament. (B) Trichrome stains shows a decrease in the ratio of elastin tissue to fibrous tissue. This finds indicated that the elastic bands of the flavum ligament are undergoing hardening, stiffening, and calcification.
Discussion
The flavum ligament serves as an elastic band that assists the spinal column in continuing the neutral position after flexion and extension movements.5 In elderly individuals, the flavum ligament is lost and replaced by fibrocartilaginous cells, leading to the formation of fibrous tissue with increased affinity for calcium deposition or known as calcification of flavum ligament (CFL). Lately, the known pathological term in the flavum ligament is ossification of the flavum ligament (OFL), characterized by structural changes of an ectopic bone formation through endochondral hardening.6
Thickening of the flavum ligament without ossification, known as hypertrophy of flavum ligament (HFL), by which the lamellar bone, through endochondral hardening of fibrocartilaginous vascularization tissue, begins at the intersection of dense ligament-osseous.7 A decreased in the flavum ligament’s elastin-to-collagen ratio, together with HFL, are associated with lumbar canal stenosis. Previous reports indicated that HFL is associated with the inflammatory process seen from cyclooxygenase-2 expression (COX-2) in the immunohistochemical examination of flavum ligament specimens. The accumulation of fibrosis tissue in the flavum ligament affects its thickness. Apparently, the higher the inflammation, the thicker the fibrotic tissue formation.1 However, the underlying molecular mechanisms of fibrosis and hypertrophy remain unclear.8 Here we sought to clarify the difference between CFL and OFL. Histologically, CFL consists of degenerated flavum ligament with temporary calcification grains, meanwhile, OFL is formed from ectopic cartilage hardening.9 CFL often affects women in their cervical region, whereas OFL is more dominant in men within the chest and lumbar regions.10 Radiographically, CFL is reported to involve only one interlaminar segment that can be easily identified using a sagittal CT scan.5 However, it is still debatable whether this HFL is an initial process of CFL or OFL.
In patients with milder symptoms, pharmacological treatment is still the mainstay of therapy. In cases where MRI images of lumbar stenosis due to thickening of the flavum ligament are inconclusive, however, paraparesis has occurred due to neurogenic claudication, decompression laminectomy surgery is the preferred treatment strategy. This rationalization is based on the histopathological process of the flavum ligament losing its elasticity and thickening over time and therefore, we should not wait for a more severe neurological deficit.
Folding the ligamentum flavum when standing will give compression to the spinal canal so that it worsens the stenosis that occurs, the complaint may improve when the patient bends down so that the ligamentum flavum is stretched again. In this study, we found that the mean thickness of the HFL were 14.9±1.41 mm in males and females was 13.7±1.29 mm which already causing claudication, meanwhile in normal population the flavum ligament thickness is 3.38 – 3.84 mm (L3-S1). If either the claudication symptoms yield minimal response of pharmacological therapy or neurological symptoms develop, the chosen treatment becomes laminectomy decompression.7,11
The weaknesses of the study are; this study did not examine the relationship or correlation but only tested the difference in mean neurological scores before and after decompression of all patients with HYL claudication. This study used all data of patients who failed conservatively, then performed surgery and recorded their neurological clinical progress. So it did not use the control group to find out the different effects of the treatment given. Patients collected were all with intermittent claudication without ischialgia complaints due to disc hernia.
Conclusion
In this report we have shown that surgical treatment has improved the short-term outcomes of symptomatic lumbar HFL associated with neurogenic claudication due to flavum ligament thickening process. The message is although the level of stenosis on MRI images is less severe, author emphasize that whatever the etiology of the stenosis if neurological deficits occur, must be treated surgically if conservatives fail.
Acknowledgments
Authors would like to take this opportunity to thank all of the patients who warmly co operated in this research program.
Conflict of Interest
There is no conflict of interest.
References
- Sairyo K., Biyani A., Goel V. K., Leaman D. W., Booth Jr R., Thomas J., et al. Lumbar ligamentum flavum hypertrophy is due to accumulation of inflammation-related scar tissue. Spine. 2007;32(11):E340–E347.
CrossRef - Coric D., Branch Jr C. L. Posterior lumbar interbody fusion in the treatment of symptomatic spinal stenosis. Neurosurgical focus. 1993;3(2):E10.
- Munns J. J., Lee J. Y., Orías A. A. E., Takatori R., Andersson G. B., An H. S., et al. Ligamentum flavum hypertrophy in asymptomatic and chronic low back pain subjects. PLoS One. 2015;10(5):e0128321.
- Löhr M., Hampl J. A., Lee J. Y., Ernestus R. I., Deckert M., Stenzel W. Hypertrophy of the lumbar ligamentum flavum is associated with inflammation-related TGF-β expression. Acta neurochirurgica. 2015;153(1):134–141.
CrossRef - Xu R., Sciubba D. M., Gokaslan Z. L., Bydon A. Ossification of the ligamentum flavum in a Caucasian man: Case report. Journal of Neurosurgery: Spin. 2008;9(5):427–437.
CrossRef - Pascal-Moussellard H., Cabre P., Smadja D., Catonné Y. Symptomatic ossification of the ligamentum flavum: a clinical series from the French Antilles. Spine. 2005;30(14):E400–E405.
CrossRef - Li F., Chen Q., Xu K. Surgical treatment of 40 patients with thoracic ossification of the ligamentum flavum. Journal of Neurosurgery: Spine. 2006;4(3):191–197.
CrossRef - Park J. B., Lee J. K., Park S. J., Riew K. D. Hypertrophy of ligamentum flavum in lumbar spinal stenosis associated with increased proteinase inhibitor concentration. JBJS. 2005;87(12):2750–2757.
CrossRef - Christiano L. D., Assina R., Goldstein I. M. Ossification of the ligamentum flavum: a unique report of a Hispanic woman. Neurosurgical focus. 2011;30(3):E15.
CrossRef - Khan M. H., Smith P. N., Donaldson W. F. Acute quadriparesis caused by calcification of the entire cervical ligamentum flavum in a white female—report of an unusual case and a brief review of the literature: case report. Spine. 2005;30(22):E687–E691.
CrossRef - Mahadewa T. B. G., Raka-Sudewi A. A., Wiryana M. Blood hsCRP And PGE2 Content With Clinical Outcome Using Modified Fenestratio-Restorative Spinoplasty Better Than Laminectomy-Fusion In Lumbar Stenosis. 2012.







