Vijay Ebenezer1, K. Balakrishnan2, R Banu Sargunar3, Senthilnadhan4
1Hod and Professor, Department of Oral and Maxillofacial Surgery , Sree Balaji Dental College and Hospital, Bharath University, Pallikaranai, chennai, 600100 2Professor, Department of Oral and Maxillofacial Surgery , Sree Balaji Dental College and Hospital, Bharath University, Pallikaranai, chennai, 600100 3Senior Lecturer, Department of Oral and Maxillofacial Surgery , Sree Balaji Dental College and Hospital, Bharath University, Pallikaranai, chennai, 600100 4Reader, Department of Oral and Maxillofacial Surgery ,Sree Balaji Dental College and Hospital, Bharath University, Pallikaranai, chennai, 600100
DOI : https://dx.doi.org/10.13005/bpj/715
Abstract
A dental implant (also known as an endosseous implant or fixture) is a surgical component that interfaces with the bone of the jaw or skull to support a dental prosthesis such as a crown, bridge, denture, facial prosthesis or to act as an orthodontic anchor. In addition to being stable in the physiological environment, titanium oxides increase calcium ion interactions, which are important for protein and subsequent osteoblast adhesion [1]. Enhanced bone bonding can be achieved with bioactive materials that form a stable unit with bone through a spontaneous formation of hydroxyapatite (HA) on their surface.
Keywords
Hydroxyapatite; Dental implant; Osseointegration
Download this article as:| Copy the following to cite this article: Ebenezer V, Balakrishnan K, Sargunar R. B, Senthilnadhan. Nano Hdroxyapatite Particulate Graft in Immediate Implant Placement - A Review Of 10 Cases. Biomed Pharmacol J 2015;8(October Spl Edition) |
| Copy the following to cite this URL: Ebenezer V, Balakrishnan K, Sargunar R. B, Senthilnadhan. Nano Hdroxyapatite Particulate Graft in Immediate Implant Placement - A Review Of 10 Cases. Biomed Pharmacol J 2015;8(October Spl Edition). Available from: http://biomedpharmajournal.org/?p=3698> |
Introduction
The basis for modern dental implants is a biologic process called osseointegration where materials, such as titanium, form an intimate bond to bone. Titanium is widely used as material for permanent implants in dental applications. Nanosized hydroxyapatite (HA) is the main component of mineral bone .The biomineralized HA layer acts as a bonding layer to the bone and integration at the atomic/molecular scale can develop. For this reason HA is proposed as a suitable coating material to provide stronger early fixation of uncemented prosthesis. Although hydroxyapatite coatings on implants showed long-term survival [2], there are concerns about their reliability under loads. Hydroxyapatite nano particles possesses exceptional biocompatibility and bioactivity properties with respect to bone cells and tissues, probably due to its similarity with the hard tissues of the body The HA naturally occurring in bone is a multi-substituted calcium phosphate, including traces of CO32- , F-, Mg2+, Sr2+, Si4+, Zn2+, Li+ etc [3, 4]. These ionic substitutions are considered to play an important role for the formation and properties of bone. The basic building block of bone tissue is mineralized collagen fibrils approximately 100 nm in diameter ,These fibrils are made of collagen fibers 300 nm long and 1 – 1.5 nm thick. Within these fibrils are the hydroxyapatite crystals. They usually form as thin flat plates parallel to the long axis of surrounding collagen fibers[5]
Case Report
This case report gives study of implants which was placed immediately following an extraction , with placement of hydroxyapatite nanoparticles (HANANO ). The use of this hydroxyapatite nanoparticles in this immediate implants provides more strength and stability to the implants , thus improvising the bone formation . The mechanism of osseointegration with faster and stronger bone formation, for better stability during the healing process, thus allowing more rapid loading of the implant 6,,7This study was done with 10 patients whose age group varied from 24- 53 yrs , The patient fulfilled the following required criteria before undergoing treatment ,a through detailed history was taken for any systemic disorders and routine blood investigations were done .Patient had fractured teeth in relation to 11 and 21(FIG 1). The patient was informed about the procedure and placement of hydroxyapatite nanoparticles ( synthetic bone particles) in detail and informed consent was taken. Pre operative OPG and IOPA (FIG 2) as taken and bone level sinus was noted .The teeth was extracted with care in preserving the buccal bones (FIG 3) , the implant was placed in the prepared socket(FIG 4) and hydroxyapatite nano particles are placed surrounding the implant (FIG 5) and packed gently and suturing was done. Immediate post operative radiograph of the implant reveals bone like mass surrounding the implant (FIG 6) ,
 |
Figure 1: Pre Operative- Fractured Incisors |
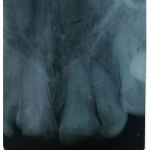 |
Figure 2: Pre Operativ Iopa |
 |
Figure 3: Atraumatic Extraction |
 |
Figure 4: Placement of Implants |
 |
Figure 5: Placement of Hydroxyapatite Nano Particles |
 |
Figure 6: Immediate Post Operative Iopa |
 |
Figure 7: Fifth Month Post Operative Opg |
These hydroxyapatite crystals get resorbed by four weeks thus inducing the osteoblast effect surrounding the implant .These HA particles are three times more stronger than cortical bone hence gives good stability to implants and immediate post operative radiograph taken( FIG 6) ,following fifth month review was done ( FIG 7) and OPG reveals a definitive bone formation around the implant thus providing more stability and less chances of failures of the implant less bone loss as noted comparatively to implants without hydroxyapatite nano particles.
Discussion
This study shows that immediate implants with hydroxyapatite nano particles which is used to bridge the small gap between the implant a submerged surgical technique provides a clinically and radiographically good result of stability and bone formation . The quality of implant surface influences wound healing at implantation site and subsequently affects osseointegration[6]. Hydroxyapatite nano particles increases the surface area of the implant , thus increasing the implant bone surface contact area and thereby implant stability. Synthetic hydroxyapatite is commercially available. Muller-Mai et al tested nanoapatite and nanoapatite/organic implants in vivo. From their results, it was seen that both materials were suitable for bone replacement and for drug release such as antibiotics, growth factors or other substances. In addition, the organic component can be used to control physical properties in the bone implantation [7]The production is usually based on aqueous precipitation or conversion from other calcium rich material. While these methods are common for supplying the material in a bulk form, coating hydroxyapatite onto other material is 20 also common[8]. The aim of this study was to observe the bone formation and stability of implants with the hydroxyapatite nano particles which proved to have better results than immediate implants without any bone grafts . Since hydroxyapatite is found in bone tissue and teeth, not only is it non-toxic but it would not be targeted by the immune system as foreign body. Therefore the local tissue inflammation and eventual scarring caused by an immunological response would not be an issue if hydroxyapatite were used.
Conclusion
Review of these cases were with one year done and IOPA and OPG revealed good density of bone formation Thus in this study we conclude that use of hydroxyapatite nanoparticles in the placement of the immediate implants provides good result in stability , less complication and perform comparatively well than without bone graft .
Reference
- Ellingsen J. A study on the mechanism of protein adsorption to TiO2. Biomaterials 1991;12:593-596
- Kido H, Saha S. Effect of HA coating on the long-term survival of dental implant: a review of the literature. J Long Term Eff Med Implants 1996;6(2):119-133.
- Dorozhkin SV, Epple M. Biological and medical significance of calcium phosphates. Angew Chem Int Ed Engl 2002;41(17):3130-3146.
- Vallet-Regí M. Ceramics for medical applications. J Chem Soc, Dalton Trans 2001:97-108
- Fratzl, Peter; Weinkamer, Richard (2007) Nature’s Heirarchichal Materials, Progress in Materials Science, in press, corrected proof, doi:10.1016/j.pmatsci.2007.06.001.
- Wennerberg A, Albrektsson T. Effects of titanium surface topography on bone integration: a systematic review. Clin Oral Implants Res 2009;20:172-184
- Beutner R, Michael J, Schwenzer B, Scharnweber D. Biological nano-functionalization of titanium-based biomaterial surfaces: a flexible toolbox. J R Soc Interface 2010;7:S93-S105.
- Albrektsson T, Lekholm U. Osseo-integration: Current state of art. Dent Clin north Am 1989;(4):537-54
- Muller-Mai CM, Stupp SI, Voigt C, Gross KA. Nanoapatite and organoapatite implants in bone: Histology and ultrastructure of the interface. J Biomed Mater Res 1995; 29: 9-18
- Ratner, Hoffman, Schoen, and Lemons (2004), Biomaterials Science, Second Edition: An Introduction to Materials in Medicine (Boston: American Press, 2004)







