Manuscript accepted on :
Published online on: 05-01-2016
Plagiarism Check: Yes
Vijayashri Sakthi1, S. Kishore Kumar2, W. S. Manjula3
1Senior lecturer, Tagore Dental college and Hospital, Chennai, India 2Department of Orthodontics, Sree Balaji Dental College and Hospital, Bharath University, Pallikaranai, Chennai-600100 3Sree Balaji Dental College and Hospital, Bharath University, Pallikaranai, Chennai-600100
DOI : https://dx.doi.org/10.13005/bpj/761
Abstract
In recent years, a trend toward implementing treatment plans that achieve immediate facial change has arisen. In “Surgery First” treatment plans, the presurgical orthodontic treatment phase is eliminated or greatly reduced, the jaws are surgically repositioned into the desired locations, and orthodontic tooth movement follows. This clinical case typically exemplifies the effect of Anterior segmental maxillary osteotomy and Mandibular anterior subapical osteotomy on improving the skeletal, dental, soft tissue and over all aesthetics of the patient.
Keywords
Anterior Maxillary Segmental Osteotomy; Surgery first; Gummy Smile
Download this article as:| Copy the following to cite this article: Sakthi V, Kumar S. K, Manjula W. S. Anticipated Benefit of “Surgery First” Approach- A Clinical Case Report. Biomed Pharmacol J 2015;8(October Spl Edition) |
| Copy the following to cite this URL: Sakthi V, Kumar S. K, Manjula W. S. Anticipated Benefit of “Surgery First” Approach- A Clinical Case Report. Biomed Pharmacol J 2015;8(October Spl Edition). Available from: http://biomedpharmajournal.org/?p=3426> |
Introduction
The general protocol in traditional orthognathic treatment has consisted of a variable length of preoperative orthodontic preparation, surgerical procedure and a relatively constant period of postoperative orthodontics.1 Recently, the performance of surgery without orthodontic
preparation (ie, “surgery first”), followed by regular postoperative dental alignment, was proposed by Nagasaka et al.2
Anterior maxillary excess presents with excessive gummy smile with increased over jet and deep overbite. The usual indications for ASMO are excessive vertical or sagittal development of the maxillary alveolar process in patients where the relationships between the posterior teeth are acceptable.
The outcome may be less than ideal if only dentoalveolar compensation is achieved. Surgical alteration of the occlusal plane can make a profound difference in terms of facial esthetics. McCollum and colleagues3 were the first to describe surgical manipulation of occlusal plane for class II div 1 or div 2 malocclusions. This article illustrates treatment with surgery first approach in Class II malocclusion with vertical maxillary excess.
Diagnosis and Etiology
A 29 year old female presented with the chief complaint of dissatisfaction with her facial appearance due to forwardly placed upper front teeth and gummy smile. She reported emotional disability because of her facial profile and requested corrective surgery as soon as possible.
On extraoral examination (fig. 1) patient presented with leptoprosopic facial form, convex profile, mild recessive chin, severe gummy smile and incompetent lips. Soft tissue attributed with Protrusive upper and lower lips and an increased interlabial gap with complete incisor exposure at rest along with 7mm of gingival show on smile. Intraoral examination revealed proclined upper incisor and severely proclined lower incisor with increased overjet and end on relationship of bilateral molars and right canine and class I canine relationship of the left canines alone.
 |
Figure 1: Pretreatment Extraoral and Intraoral records |
Table 1: Cephalometric Data
| NORM | PRE TREATMENT | POST TREATMENT | |
| Skeletal
SNA SNB |
82˚ 80˚ |
85˚ 76˚ |
81˚ 76˚ |
| ANB
N perp to point A N perp to point Pog SN to GoGn
Dental U1 to NA L1 to NB IMPA L1- A Pog Overjet Overbite Soft tissue S line to upper lip S line to lower lip NLA
|
2˚
0±2mm 0 to -4mm 32˚
4mm, 22˚ 4mm, 25˚ 90˚ 1±2mm 3.4 2.8
|
9˚
3 -12 34˚
7mm, 23˚ 15mm, 44˚ 113˚ 7mm 5mm 5mm
5mm 10mm 108˚ |
4˚
-4mm -16mm 34˚
6mm, 19˚ 10mm, 33˚ 103˚ 7mm 1mm 3mm
2mm 4mm 112˚ |
Discolouration was observed in relation to asymptomatic 21, non vital with no periapical pathology. Cephalometric evaluation (Table I) revealed Class II skeletal pattern with prognathic maxilla and retrognathic mandible with anterior maxillary excess and severely proclined lower incisors and increased lower anterior facial height.
Treatment Objectives
The treatment objectives included the improvement of the protrusive profile; elimination of maxillary and mandibular dental protrusion; reduce gummy appearance of the maxilla and correction of dental relationship.
Treatment Plan
Because the patient was extremely self-conscious about her appearance, she accepted a “surgery-first” approach that would achieve a normal occlusion, enhance her facial esthetics and potentially reduce orthodontic treatment time. Nonvital asymptomatic 21 were endodonticaly treated prior to surgery. Using virtual prediction (Fig. 2) and model set up, treatment was planned for extraction of upper and lower first premolars and segmental osteotomy procedures to retract the maxillary and mandibular dentoalveolar segments.Both the arches were operated on the same day under General anesthesia, maxillary and mandibular first premolars were extracted at the time of surgery. Since the relationship between the posterior occlusion were acceptable for orthodontic correction at a later stage, and the arches were aligned without the presence of crowding: Surgery without braces was planned for at the start of treatment.
 |
Figure 2: Surgical plan Dolphin Prediction compared |
The treatment plan included anterior maxillary osteotomy with 5mm impaction and 4mm setback along with extraction of upper first bicuspids to reduce the incisal show was carried out. Mandibular anterior subapical osteotomy with lower first bicuspid extraction were done to achieve ideal inclination of lower incisors and to level the occlusal plane along with approximation of the extraction spaces were carried out in the mandible (Fig. 3).
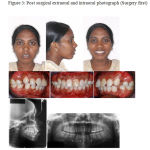 |
Figure 3: Post surgical extraoral and intraoral photograph (Surgery first) |
Treatment Progress
The patient was planned for orthognathic surgery well before any orthodontic procedures were initiated. 4 weeks after surgery .022″ Roth prescription brackets were bonded in both the arches. Leveling and aligning was performed by using Nickel titanium continuous arch wire both in the maxilla and mandible. Leveling and aligning was carried out until 0.019”X 0.025” stainless steel archwire could be fully engaged in the bracket slot. Retraction hooks were soldered distal to the lateral incisors, closed Niti coil spring which was engaged from the first molar tube to the soldered hook on the archwire delivering a force of 250gms for en-masse retraction using sliding mechanics was carried out in both the arches (Fig 4). Mild anchor loss of the lower molars was expected and was sufficient to bring the molars to classI relationship.
 |
Figure 4: Retraction mechanics |
Leveling and aligning was complete by 1.5 months followed by retraction to close the residual post surgical extraction spaces took 2 months period.
Treatment Results:
At the end of treatment, the protrusive facial profile was improved with reduction of gummy appearance. The proclination was eliminated, and Class I molar and canine relationships with normal overjet and overbite were established. (Fig. 5)
However, it was noted that the stabilization plates in relation to the lower anterior segment was in close approximation to the lower anterior root apices. Although there was no interference during retraction the plates were decided to be removed 8 months post surgery under local anesthesia.
On the panoramic and periapical radiographs taken at the end of treatment, well-aligned and parallel roots of the teeth were noted. The final lateral cephalometric measurements and
the superimpositions of the initial and final lateral cephalometric radiographs revealed that the lower facial height was normal, the Molar and canine relationship were in class I, the upper and lower incisors were retracted and the upper and the interlabial gap was reduced after orthodontic treatment.
A balanced occlusion and facial esthetics were achieved after 10 months of total treatment time. Permanent retention was planned in both the arches with bonded lingual retainers.
 |
Figure 5: Post treatment Intraoral and extraoral records |
Discussion
Orthodontic treatment of Class II malocclusion with increased overjet and anterior maxillary excess could have been accomplished with conventional 0rthodontic treatment or surgical approach with dental decompensation. However, the need for accelerating the treatment progress to meet the patient’s expectations during the initial phases of therapy surgery first approach without orthodontic intervention eliminated the unsightly presurgical decompensation profile and allowed the chief complaint of the patient to be addressed at the beginning of the treatment. Immediate resolution of the soft tissue and skeletal imbalance is an added advantage in surgery first approach. 2, 4
The pre-surgical orthodontic phase in conventional three-step orthognathic surgery cases is the most time consuming step. Bypassing this step results in an overall shortened treatment time to 1 to 1.5 years or less.3 Pre surgical planning along with surgical phase required 2 months. Post surgical inflammation was reduced in 3 weeks period. Thus Orthodontic treatment was initiated immediately by the 4 th week post surgery to take advantage of the regional acceleratory phenomenon of the osteotomy site to close the remaining extarcion spaces. This could be biologically co-related with the transient RAP phenomenon as mentioned by Frost5 which remains active for first 4 months.
A dramatic improvement in facial esthetics and occlusal function was realized with the completion of treatment.(Fig. 5) The lip competency, gingival exposure on smile and facial contour was significantly improved. The patient was very satisfied with the results of treatment. The excessive vertical dysplasia was dramatically reduced, and most of the cephalometric values were brought into the normal range.(Table 1) The anterior maxillary excess was significantly reduced, an ideal over jet and overbite and the chin deficiency was well addressed.
Conclusion
Performing orthognathic surgery before orthodontic treatment has multiple advantages namely shortened treatment time, increased patient acceptance, and utilization of the regional acceleratory phenomenon. If the cases are selected carefully, the orthodontist and the surgeon are experienced enough to predict the final occlusion beforehand, and the level of cooperation between the clinicians is high, the results are very promising. the patient’s well-being and chief complaint should always be the first priority.
High orthodontic efficiency responds to the correction of the skeletal bases as a starting point and accelerated tooth movement increased the postoperative metabolic turnover. This case illustrates the importance of proper diagnosis and treatment planning. A team approach with the orthodontist and surgeon having input before the initiation of treatment resulted in achieving stable, functional, and esthetic results. The patient has reported a better self-esteem and a greater degree of pleasure related to her appearance.
References
- Proffit WR, White RP, Sarver DM: Contemporary Treatment of Dentofacial Deformity. St Louis, MO, Mosby, 2003, 250
- Nagasaka H, Sugawara J, Kawamura H, et al: “Surgery first” skeletal class III correction using the skeletal anchorage system. J Clin Orthod 2009; 43:97.
- McCollum, A.G.; Reyneke, J.P.; and Wolford, L.M.: An alternative for the correction of the Class II low mandibular plane angle, Oral Surg. Oral Med. Oral Pathol . 1989; 67:231-241.
- Baek, S.H.; Ahn, H.W.; Kwon, Y.H. & Choi, J.Y. (2010). Surgery First Approach in Skeletal Class III Malocclusion Treated with 2-Jaw Surgery: Evaluation of Surgical Movement and Postoperative Orthodontic Treatment. Journal of Craniofacial Surgery, Vol.21, No.3, (March, 2010), pp. 332-338
- Frost HM. Biology of fracture healing – An overview for clinicians Part I and II. Clini Orthop Relat Res 1989;248:283.







