Manuscript accepted on :
Published online on: 19-12-2015
Plagiarism Check: Yes
Neeta Raj Sharma
School of Biotechnology and Biosciences, Lovely Professional University, Phagwara, India.
DOI : https://dx.doi.org/10.13005/bpj/436
Abstract
Study comprised one thousand suspected individuals (884 females and 116 males) reported for the screening of thyroid disorders of different age and sex from Kangra district of Himachal Pradesh. History, sign and symptoms of individuals were recorded and total triiodothyronine (TT3), thyroxine (TT4) and thyroid stimulating hormone (TSH) levels were estimated by using micro well Enzyme Linked Immunosorbant Assay (ELISA) in blood samples. Overall 35.7% were having visible goitre and 16.3% were presented with tremors. Puffiness of face was presenting feature in hypothyroid patients. 43.5% females of 31-50 years age group were maximally affected with thyroid dysfuntions. The association between age group and number of female patients was found significant (X7 2 =15.120, P<0.05) and 5.2% males were found to be suffered from thyroid dysfunctions (X7 2 =14.07, P<0.05) maximally affected at 51-60 years age group.
Keywords
Thyroid Stimulating Hormone (TSH); Hypothyroidism; Hyperthyroidism; Kangra
Download this article as:| Copy the following to cite this article: Sharma N. R. Thyroid Dysfunction in Suspected Population of Kangra Valley in Himachal Pradesh, India. Biomed Pharmacol J 2013;6(2) |
| Copy the following to cite this URL: Sharma N. R. Thyroid Dysfunction in Suspected Population of Kangra Valley in Himachal Pradesh, India. Biomed Pharmacol J 2013;6(2). Available from: http://biomedpharmajournal.org/?p=2788 |
Introduction
Almost one-third of the world’s population lives in areas of iodine deficiency [1]. Iodine deficiency disorders are major public health problem in India. Thyroid tissue is present in all vertebrates. The normal adult thyroid weighs about 20gms.When the dietary intake falls down 10 microgram per day, thyroid synthesis is inadequate and secretion declines [2]. Iodine is micronutrient, which is essential for normal growth and development. Its deficiency leads to a host of physical and neurological abnormalities. These are referred collectively as IDD (Iodine Deficiency Diseases). Epidemiological studies of thyroid dysfunction have limitations, for example the definition of overt hypothyroidism and subclinical hypothyroidism, the selection criteria of the sample used, the influence of age, sex, genetic and environmental factors and the different techniques used for the measurement of thyroid hormones and the relative paucity of incidence data [3]. In India, Sub Himalayan belt extending from Kashmir to Assam is well recognized area of endemic iodine deficiency. Surveys conducted by the National Goiter Survey Team of the Directorate General of health Services during the past three decades have revealed a high prevalence of endemic goiter in different states [4]. According to the profile of thyroid disorders in a referral center in North India, 75% hypothyroid, 6% hyperthyroid and 19% euthyroid goiter cases have been reported [5]. Iodine content of staple food (rice) and drinking water was found to be poor in sub Himalayan zone of India [6]. Goitrogens in the diet, such as thiocyanate in incompletely cooked Cassava or thioglucosides in Brassica vegetables, can explain some of the differences in prevalence of endemic goitre in areas with similar degrees of iodine deficiency [2]. Thyroid disorders are common endocrine diseases in Himachal Pradesh. District Kangra is a known area of endemic iodine deficiency. So far age and sex wise study on thyroid dysfunctions in Kangra district was not available hence present study was undertaken to evaluate the status of thyroid dysfunctions after more than ten years of salt iodination program in state.
Materials and Methods
The study was conducted in department of Biochemistry, Dr. RPGMC, Kangra at Tanda. Total one thousand cases of suspected individuals of both the sex of varying age group ranging from one year to eighty years from Kangra district of Himachal Pradesh were undertaken for study. Suspected cases divided initially into two categories on the basis of sex and eight catagories on the basis of age groups. Study included pertinent history and relevant laboratory investigations. The results were correlated with the nature and duration of symptoms. Laboratory investigations included total T3, T4 and TSH in blood by using micro well Enzyme Linked Immunosorbant Assay (ELISA, Bio-Rad). Kits were procured from Pathozyme, Omega Diagnostics Limited, Scotland UK. Precaution was taken at the step of washing, which was carried out by ELISA plate washer (Bio-Rad, Microtech) to maintain uniformity of the results. Cross sectional study was designed and statistical analysis was done by using chi square test.
Results and Discussion
Out of total one thousand suspected cases, the number of suspected females (884) was comparatively more than the suspected males (116). Thyroid disorders are common endocrine diseases in the state. District Kangra in Himachal Pradesh is a known area of endemic iodine deficiency. A goiter prevalence of 55% was reported from the district in 1956. The prevalence of goiter was 12.1% in 1999. Despite years of salt iodization under the universal iodization program, the total goiter rate (TGR) was found to be 19.8% in 2004 [7]. No biochemical deficiency of iodine was found in the population studied despite that 36% families were consuming salt with the iodine content less than 15 ppm. The higher prevalence has been attributed to a chronic iodine deficiency state [7]. Figure 1 shows the distribution of suspected cases for thyroid dysfunction with reference to various age groups. The result reveals maximally affected age group is from 31 to 50 years, which was followed by 21-30, 51-60, 11-20, 0-10, 61-70 and 71-80 years. Percentage of females suffering from hypothyroidism was maximum (7.3%; TSH 15.21uIU/l) in the age group ranging from 41-50 followed by the age group of 31-40 years (7%), 21-30 years (4.4%), 51-60 (2.2%), 11-20 (1.7%), 0-10 and 71-80 years (0.5%) (Table1). It has been reported that thyrotoxicosis is predominantly a disorder in women. The presence of opthalomopathy is not uncommon with Grave’s disease. Toxic multinodular goiter is more common than toxic adenoma. Some unique features attributed to thyrotoxicosis in elderly are the presence of thyrocardiac disease in the form of atrial fibrillation and heart failure in our set-up. These patients have invariably neglected their symptoms. A poor pregnancy outcome and infertility due to thyroid disorders is common among reproductive women [8]. In case of male individuals, maximally affected age group observed was 51-60 years (1.1%). However the least affected age group noted was of 0-10 years. The highest TSH value obtained in the age group of 21-30 years was 17.05uIU/l followed by14.99 uIU/l in 51-60 years (Table1). In the community, the most Common aetiology is chronic autoimmune thyroiditis.1,9 In the original Whickham survey, 8 % of women (10 % of Women over 55 years of age) and 3 % of men had subclinical Hypothyroidism.8 In the Colorado, USA, study, 9.4 % of the subjects had a high serum TSH concentration, Of whom 9.0 % had subclinical hypothyroidism.4 Among those with a high serum TSH concentration, 74 % had a value between 5.1 mu/L and 10 mu/L and 26 % had a value greater than 10 mU/L. The percentage of subjects with a high serum TSH concentration was higher for women than men in each decade of age, and ranged from 4 to 21% in women and 3 to 16% in men [9].
Females (5.9%) of 31 to 40 years were observed with raised TT3 values however the maximum mean TT3 value noted was 6.8 ng/ml in the age group of 1 to 10 years followed by 5.0 ng/ml in 41-50 years (Figure 2). 6.1% females with elevated TT4 values were observed from 31-50 years whereas mean TT4 value was found highest (28.2 ng/ml) in age group of 71-80 years which was followed by 41-50 years (19.39 ng/ml), 51-60 years (18.74 ng/ml). In the age group 1 to 10 years and 61-70 years no raised mean TT4 was observed (Figure 3). In one of the study, the prevalence of hyperthyroidism in women was found between 0.5 and 2 %, and was ten times more common in women than in men in iodine-replete communities. In the Whickham survey, the prevalence of undiagnosed hyperthyroidism was 4.7 per 1000 women [10]. In present study, males (0.6%) with high TT3 values by the age group of 31 to 40 and 51 to 60 years were observed which was followed by 0.3% in the age group of 1 to 10, 21 to 30 & 41 to 50 years (Figure2). The maximum mean TT3 value was obtained in the age group of 21 to 30 years (6.13ng/ml), followed by 41 to 50 years (4.2ng/ml). Slight variation was obtained in the mean TT3 values of the individuals of age group 31 to 40 years (3.78ng/ml) and 51 to 60 years (3.7ng/ml), 1 to 10 years (3.46ng/ml), 61 to 70 years (3.2ng/ml). In the age group of 1 to 10 years the mean TT3 value was 3.46ng/ml, which was followed by 3.2ng/ml and 3.0ng/ml in the age group of 61 to 70 and 71 to 80 years. Males (0.8%) of 31 to 40 years with elevated level of TT4 were observed followed by 0.1% of 61 to 80 years age group. However, maximum mean TT4 values were recorded in the age group of 1 to 10 years (34.6ng/ml), which was followed by 61 to 70 years (33.7ng/ml). Individuals of age group of 21 to 30 years and 51 to 60 years showed slight variation in TT4 values i.e. 18.5 and 18.1ng/ml and with lease value (12ng/ml) at 11 to 20 years (Figure3). In the large population study in Tayside, Scotland, 620 incident cases of hyperthyroidism were identified with an incidence rate of 0.77/1000 per year (95 % CI 0.70 to 0.84) in women and 0.14/1000 per year (95 % CI 0.12 to 0.18) in men [11]. The incidence increased with age, and women were affected two to eight times more than men across the age range. Recent further analysis suggested that the incidence of thyrotoxicosis was increasing in women but not in men between 1997 and 2001 [12]. As per study available, from screening large US population samples [13], differences in the frequency of thyroid dysfunction and serum thyroid antibody concentrations in different ethnic groups was reported whereas studies from Europe have revealed the influence of dietary iodine intake on the epidemiology of thyroid dysfunction [13]. Studies of incidence of autoimmune thyroid disease have only been conducted in a small number of developed countries [14]. There is an urgent need for long-term studies of the effects of identification and treatment of both subclinical hypothyroidism and subclinical hyperthyroidism, to determine if there is indeed benefit from screening for thyroid dysfunction in adults [15].
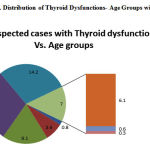 |
Figure 1: Distribution of Thyroid Dysfunctions- Age Groups wise
|
Table 1. Levels of Thyroid Stimulating Hormone (TSH)- Sex and Age group wise
| Age Group
(Years) |
% of Patients
(Females) |
TSH (uIU/l)
(Mean) |
% CV | % of Patients
(Males) |
TSH (uIU/l)
(Mean) |
% CV |
| 0-10 | 0.5 | 12.84 | 65.8 | 0.1 | 6 | 2.4 |
| 11-20 | 1.7 | 12.73 | 47.9 | 0.2 | 10.9 | 32.4 |
| 21-30 | 4.4 | 11.38 | 51.3 | 0.4 | 17.05 | 58.2 |
| 31-40 | 7.0 | 12.93 | 3.1 | 0.4 | 13.65 | 47.0 |
| 41-50 | 7.3 | 15.21 | 99.4 | 0.5 | 13.12 | 90.0 |
| 51-60 | 2.2 | 12.46 | 47.8 | 1.1 | 14.99 | 45.0 |
| 61-70 | 0.5 | 15.42 | 52.3 | nil | – | – |
| 71-80 | nil | nil | nil | nil | – | – |
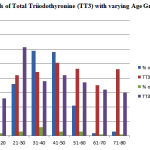 |
Figure 2: Levels of Total Triiodothyronine (TT3) with varying Age Groups and Sex
|
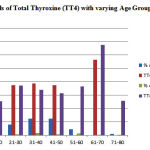 |
Figure 3: Levels of Total Thyroxine (TT4) with varying Age Groups and Sex
|
Conclusion
Present study concludes that females are more affected with thyroid dysfunctions as compared to males hence regular screening of at least thyroid stimulating hormone in serum is recommended as routine test in iodine depleted areas since thyroid dysfunctions relate with other metabolic diseases also.
Acknwledgement
Author acknowledges the support provided by Department of Biochemistry, R.P. Govt. Medical College Tanda at Kangra, India
References
- Zimmermann, M.B., Jooste, P.L., Pandav, C.S., ‘’Iodine-deficiency disorders’’. Lancet 372:1251-1262, (2008)
- Chatterjea, M.N. and Shinde, R., Medical Biochemistry, 2nd edn. Jaypee Brothers, New Delhi, P 734, (1995)
- Mansoor Ahmad, S. Mahboob Alam, Salman Habib, Mehjabeen, Noor Jahan., ‘’Effects of thyroid dysfunction on systolic / diastolic blood pressure, pulse rate, Serum creatinine and liver enzymes’’ Int. Res. J. Pharm., 4(8):117:119, (2013)
- World Health Organization Monograph Series, Endemic Goitre., Geneva., No. 44., (1960)
- Virmani, A., Menon, P. S., Karmarkar, M. G., Gopinath, P.G., Padhy, A. K. ,“ Profile of thyroid disorder in a referral center in north India. Ind. Pediater. 26 (3), 265-9, (1989)
- Sharma, S. K., Chelleng, P. K., Gogoi, S., Mahanta, J., “ Iodine status of food and drinking water of a sub Himalayan zone of India., Int. J. Food Sci. Nutr. 50 (2), 95-8, (1999)
- Umesh Kapil, Sharma T. D., Preeti Singh., “Iodine Status and Goiter Prevalence After 40 Years of Salt Iodisation in the Kangra District, India”, Indian Journal of Pediatrics, Vol. 74 February, (2007)
- Raina, S., “Endocrinology in the hills of Himachal Pradesh, India”, Indian J Endocrinol Metab. Mar-Apr; 16(2): 316–317. (2012)
- Hollowell, JG, Staehling NW, Flanders WD, et al., “Serum TSH, T4, and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab; 87:489-99, (2002)
- Tunbridge, WMG, Evered DC, Hall R, Appleton D, Brewis M, Clark F, Evans JG, Young E, Bird T, Smith PA., “The spectrum of thyroid disease in the community: the Whickham survey”., Clin Endocrinol; 7: 481-493. (1977)
- Flynn, RV, MacDonald, TM, Morris, AD, Jung, RT, Leese, GP., “ The Thyroid epidemiology, Audit and Research Study; thyroid dysfunction in the general population. J Clin Endocrinol Metab; 89:3879-3884., (2004)
- Leese, GP, Flynn, RV, Jung, RT, MacDonald, TM, Murphy, MJ, Morris, AD., “Increasing prevalence and incidence of thyroid disease in Tayside, Scotland: The Thyroid Epidemiology, Audit and Research Study (TEARS)”, Clin Endocrinol, 68:311-316, 2008
- Mark, P. J. Vanderpump, “The epidemiology of thyroid disease” British Medical Bulletin., vol. 99., Issue 1., 39-51., (2011)
- Parle, J.V., Franklyn, J.A., Cross, K. W., et al., “Prevalence and follow–up of abnormal thyrotrophin (TSH) concentrations in the elderly in the United Kingdom”., Clin Endocrinol, (Oxf); 34:77-83, (1991)
- Surks, M. I., Ortiz, E., Daniels, G.H., et al., “ Subclinical thyroid disease: scientific review and guidelines for diagnosis and management”, JAMA, 291:228-238, (2004)
(Visited 598 times, 1 visits today)







