Saidatri Arige1* , Lakshmana Rao Atmakuri1
, Lakshmana Rao Atmakuri1 , Rasheed Shaik2
, Rasheed Shaik2 , Manasa Gude3
, Manasa Gude3 , Vijaya Kumar Ghanta4
, Vijaya Kumar Ghanta4 and Ramesh Alluri5
and Ramesh Alluri5
1Department of Pharmaceutical Analysis, V. V. Institute of Pharmaceutical Sciences, Gudlavalleru, Andhra Pradesh, India.
2Department of Pharmaceutics, V. V. Institute of Pharmaceutical Sciences, Gudlavalleru, Andhra Pradesh, India.
3Department of Pharmacology, V. V. Institute of Pharmaceutical Sciences, Gudlavalleru, Andhra Pradesh, India.
4Department of Pharmacy Practice, KVSR Siddhartha College of Pharmaceutical Sciences, Vijayawada, Andhra Pradesh, India.
5Department of Pharmacology, Vishnu Institute of Pharmaceutical Education & Research, Narsapur, Telangana, India.
Corresponding Author E-mail: sai.dhatri_arige@yahoo.co.in
DOI : https://dx.doi.org/10.13005/bpj/3071
Abstract
Digital dermoscopy is an advanced, non-invasive imaging technique that enhances conventional dermoscopy by utilizing computerized imaging technology to assess skin lesions, aiding in the early-stage diagnosis of skin cancers, including melanoma, basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). This technique provides high-resolution images, enabling detailed examination and magnification of lesions, which helps clinicians identify subtle changes in lesion morphology over time. Additionally, it allows for long-term monitoring through serial imaging, facilitating more accurate follow-up assessments. Integrating Artificial Intelligence (AI) and machine learning algorithms has significantly improved diagnostic accuracy by enhancing the detection of malignancies, allowing for faster and more reliable analysis of dermoscopic images. Despite its advantages, digital dermoscopy faces several challenges that limit its widespread use. Image quality can be compromised by device limitations, lighting conditions, and operator proficiency, which can affect the accuracy of diagnoses. Furthermore, the technique remains heavily dependent on clinician expertise, as the interpretation of dermoscopic images is complex and requires specialized training. Moreover, the integration of digital dermoscopy into electronic health records (EHR) and telemedicine systems presents logistical and financial challenges, including issues related to data storage, accessibility, and reimbursement. This review provides an in-depth examination of the principles, advantages, limitations and prospects of digital dermoscopy, focusing on its potential to advance dermatological practice through improved diagnostic capabilities, more efficient patient management, and enhanced early detection of skin cancers.
Keywords
Artificial Intelligence; Basal cell carcinoma; Digital Dermoscopy; Melanoma; Skin lesions; Squamous cell carcinoma.
Download this article as:| Copy the following to cite this article: Arige S, Atmakuri L. R, Shaik R, Gude M, Ghanta V. K. Alluri R. Digital Dermoscopy: Advancements in Skin Cancer Diagnosis and Monitoring. Biomed Pharmacol J 2025;18(March Spl Edition). |
| Copy the following to cite this URL: Arige S, Atmakuri L. R, Shaik R, Gude M, Ghanta V. K. Alluri R. Digital Dermoscopy: Advancements in Skin Cancer Diagnosis and Monitoring. Biomed Pharmacol J 2025;18(March Spl Edition). Available from: https://bit.ly/4gZ4cur |
Introduction
Dermoscopy or dermatoscopy is an essential skin diagnostic method that does not require a skin lesion biopsy or excision and involves a dermatoscopy that provides a high-resolution enhancement of light reflection, making it possible to identify skin layers. Employing this technique also helps to increase the diagnostic accuracy of skin malignancies on account of the examination of such aspects as pigment networks, blood vessels, and follicular openings which are usually not conspicuous to the naked eye.1 Manual dermoscopy has been used widely to diagnose many skin ailments, but it has its weaknesses, such as the inability to store images, compare images at different times, and the lack of automated analysis.
Table 1: Comparison of Traditional Dermoscopy vs Digital Dermoscopy
| Feature | Traditional Dermoscopy | Digital Dermoscopy |
| Image Capture | Real-time visual observation | High-resolution digital images with zooming and storage |
| Documentation | No capability to store images | Allows storage, comparison, and longitudinal tracking of images |
| Diagnostic Support | No automated analysis | AI-powered analysis, automated algorithms for diagnosis |
| Monitoring of Lesions | No tracking of lesion progression | Enables longitudinal monitoring of lesions over time |
| Remote Consultation (Teledermatology) | Limited capability | High-quality digital images sent for remote evaluation |
| Cost | Lower initial cost | Higher initial investment, but potentially lower long-term cost |
Digital dermatoscopy is the combination of normal dermatoscopes with digital high-magnification cameras. The identification of the chain of images using digital systems for building up images and also for storage and comparison leads to a higher accuracy in the diagnosis. Prominent models of dermoscopy use digital dermoscopy systems to incorporate additional features such as automated image analysis and incorporation of artificial intelligence algorithms to help detect and determine the probability of malignancy of lesional skin.2-3 These advancements in digital systems help overcome the limitations of traditional dermoscopy by enabling objective image analysis, reducing clinician biases, and providing more analyzable results. They supplement dermoscopy and assist in eliminating the biases inherent to this traditional method of skin imaging by providing more analyzable results.
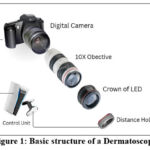 |
Figure 1: Basic structure of a DermatoscopeClick here to view Figure |
The Principles of Digital Dermoscopy
The key principles of digital dermoscopy include:4-5
High-Resolution Imaging
It uses high-definition cameras to capture images of skin lesions at a high resolution power. By imaging at this high resolution, clinicians are able to scan for fine details in the structures of the skin, which is key to detecting small changes in lesions and ensuring accurate diagnosis.
Polarized Light
This technology minimizes surface reflections from the skin and enhances the image quality of deeper skin layers and structures that are less frequently seen, such as blood vessels and pigment patterns. Polarized light works by filtering out light that is reflected off the skin’s surface, allowing deeper structures to be visualized without interference from superficial reflections. As a result, it improves the ability to identify malignant features. However, this technique may compromise the overall clarity of the dermoscopic images by removing some surface details, which could impact the visualization of superficial features.
Image Documentation and Tracking
One of the most significant advantages of digital dermoscopy is its ability to systematically document and store skin lesions over time. The ability to track lesion changes and detect suspicious changes early, including signs of skin cancer development, enables clinicians to monitor lesion evolution and diagnose earlier.
Artificial Intelligence (AI) Integration
More digital dermoscopy systems are now partially or fully aided by AI and machine learning algorithms to help analyze dermoscopic images. With these tools, patterns associated with different skin conditions, such as melanoma and non-melanoma skin cancers (like basal cell carcinoma and squamous cell carcinoma), can be identified, which increases diagnostic accuracy and decreases human error. Prominent examples of AI algorithms currently in use include deep learning models like convolutional neural networks (CNNs) for detecting melanoma and systems developed by companies like SkinVision and MoleMap, which have demonstrated clinical success in accurately identifying malignant lesions in real time.
Teledermatology
Telemedicine is also supported by digital dermoscopy through the ability to transfer high-quality images to dermatologists for remote evaluation. This is particularly helpful in underserved areas, where access to specialists is limited, providing timely diagnosis and treatment.
Additional Considerations Regarding AI Integration
While AI-powered digital dermoscopy systems have shown significant promise, there are still limitations and challenges that must be addressed. One major challenge is the possibility of false positives or false negatives, which can occur when the AI system misinterprets the image or fails to recognize subtle malignant features. This emphasizes the importance of human oversight in the diagnosis process, as dermatologists must still review AI-assisted findings to ensure accurate diagnosis and avoid misdiagnosis. Furthermore, AI algorithms may struggle with certain skin tones or uncommon skin conditions, which could lead to reduced accuracy in diverse patient populations.
Applications in Dermatology
Skin Cancer Early Detection
Skin cancer (melanoma, basal cell carcinoma (BCC), squamous cell carcinoma (SCC)) is one of the most common cancers worldwide. Improving patient outcomes relies on early detection and numerous studies have shown that digital dermoscopy plays a critical role in the early identification of skin cancers. Digital dermoscopy has been shown to improve sensitivity and specificity when used in addition to clinical examination.6 For instance, studies have demonstrated that digital dermoscopy increases the sensitivity of melanoma detection to approximately 95% compared to 80% with clinical examination alone. Additionally, its specificity has been reported to exceed 80%, helping to distinguish malignant lesions from benign ones with greater accuracy.
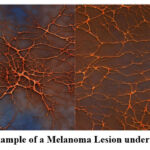 |
Figure 2: Example of a Melanoma Lesion under DermoscopyClick here to view Figure |
Melanoma Diagnosis
Although it is the least common form of skin cancer, melanoma is the deadliest, and early detection is essential for improving survival rates. Digital dermoscopy enables clinicians to identify characteristic features of melanoma, such as asymmetry, irregular borders, multiple colors, and atypical blood vessels, with much greater precision.7 Recent studies have shown that digital dermoscopy can reduce diagnostic errors in melanoma detection by up to 50% when compared to traditional clinical examinations. Different algorithms have been developed to assist clinicians in diagnosing melanoma, such as the 7-point checklist and ABCD rule, which combine dermoscopic features to assist in identifying high-risk lesions.8,9 Moreover, AI-enhanced digital dermoscopy systems have been shown to improve diagnostic accuracy by up to 20% when compared to traditional methods, providing a promising tool for early melanoma detection.
Non-Melanoma Skin Cancers
Strains of common non-melanoma skin cancers—both BCC and SCC—are also prevalent and can lead to significant morbidity. Digital dermoscopy helps to distinguish these malignancies from benign lesions such as seborrheic keratosis and actinic keratosis.10,11 In addition, digital dermoscopy can be used to monitor the evolution of pre-cancerous lesions, with subtle changes indicating the onset of malignancy.12 For instance, studies have demonstrated that digital dermoscopy can detect BCC with sensitivity of up to 90% and specificity of around 85%. This makes it a valuable tool for identifying both melanoma and non-melanoma cancers early.
Lesions over Time Monitoring
Digital dermoscopy has the significant advantage of recording and tracking skin lesions over time. It is especially helpful for patients who have many moles or are at high risk for developing skin cancer, such as those with a personal or family history of melanoma.13 By comparing serial images, clinicians can detect subtle changes in lesion size, shape, and/or color, which may indicate the development of malignancy.14 Longitudinal tracking with digital dermoscopy has been shown to improve the detection of melanoma recurrences by up to 35%, underscoring its importance in continuous skin monitoring.15
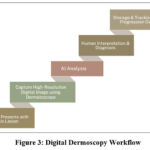 |
Figure 3: Digital Dermoscopy WorkflowClick here to view Figure |
Teledermatology
In recent years, teledermatology, or transmitting digital images for remote consultation, has become increasingly popular. Teledermatology offers one such tool—digital dermoscopy—to provide patients in rural or underserved areas with expert dermatologic care without requiring a patient to travel. Studies have shown that teledermatology consultations involving digital dermoscopy result in faster diagnoses and improved access to care in underserved areas.16-18 Relatives do not have to visit dermatologists in person for diagnosis or advice on further action, as high-quality digital images can be sent electronically. This has the potential to decrease wait times to see a dermatologist and increase access to care, particularly in areas with limited healthcare resources.
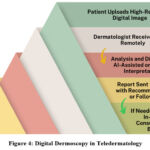 |
Figure 4: Digital Dermoscopy in TeledermatologyClick here to view Figure |
Advantages of Digital Dermoscopy
Enhanced Visualization
Digital dermoscopy provides high-resolution images that improve the visualization of dermal and epidermal structures, enabling clinicians to detect features that may be missed during physical exams.19
Prospective Monitoring and Recordings
The ability to store and compare images over time allows for longitudinal tracking of lesions, helping to detect morphological changes and potential malignancies, particularly in high-risk patients.20,21
Support for Artificial Intelligence Integration
AI systems in dermoscopy analyze large datasets of skin images, improving diagnostic accuracy.22 These systems have been shown to match or exceed dermatologists’ performance in detecting conditions like melanoma, although AI is designed to complement human expertise, not replace it.23-26
Telemedicine and Remote Access
Teledermatology enables remote skin lesion analysis, expanding access to dermatological care in underserved areas. This facilitates timely consultations and triage, ensuring patients with limited access to specialists receive proper care.27-33
Challenges and Limitations
Image Quality and Standardization
The accuracy of digital dermoscopy depends on image quality, which can be impacted by lighting, camera settings, and capture methods. Standardizing imaging protocols is crucial for consistent diagnostic results.34-35
Expertise and Training
Accurate diagnosis through digital dermoscopy requires clinician proficiency in using the equipment and interpreting images. Ongoing training ensures clinicians stay updated on the latest technologies.36-37
Integration with Electronic Health Records (EHR)
While integrating digital dermoscopy with EHR systems enhances patient care by providing easy access to lesion history and enabling longitudinal tracking, technical challenges and high costs hinder widespread adoption.38
Cost and Accessibility
Despite decreasing costs, digital dermoscopy remains expensive, limiting its availability in smaller clinics or resource-limited areas. Teledermatology services also face accessibility challenges in rural settings, highlighting the need for more affordable solutions and infrastructure.39-40
Comparative Analysis of Digital Dermoscopy Systems Findings
Several studies have compared the effectiveness of various digital dermoscopy systems in diagnosing skin cancer and monitoring lesions over time. A key comparison between high-resolution digital dermoscopy and traditional dermoscopy has demonstrated that the digital version allows for more precise documentation and the ability to analyze images over time, improving the detection of skin cancers. Additionally, studies comparing AI-enhanced digital dermoscopy systems with traditional methods have shown that AI systems can identify suspicious lesions with greater accuracy and consistency, reducing the risk of human error.41
A comparative study also highlighted the advantages of teledermatology using digital dermoscopy in underserved areas, where access to dermatologists is limited. These studies have demonstrated that remote consultations, combined with digital dermoscopy, resulted in more timely diagnoses and better outcomes for patients with skin lesions. However, challenges remain in terms of standardizing protocols and ensuring high image quality for teledermatology consultations.42
Alternative Approaches to Skin Cancer Diagnosis
While digital dermoscopy has shown significant promise in enhancing diagnostic accuracy and supporting telemedicine, it’s important to also consider traditional methods of skin cancer diagnosis. These include clinical visual examinations, biopsy, and histopathological analysis, all of which have long been the gold standard for detecting skin cancer, particularly melanoma. However, these methods present several limitations compared to digital dermoscopy. Traditional visual examination relies heavily on the clinician’s experience and may miss subtle signs of malignancy. Biopsy, though definitive, is invasive and may not be ideal for patients with numerous lesions or those in the early stages of malignancy. Moreover, these conventional methods do not offer the same ability to track lesion changes over time, which digital dermoscopy excels at, providing a more comprehensive approach to skin cancer monitoring.
Despite these limitations, traditional methods still play a crucial role in diagnosis, particularly when digital dermoscopy alone cannot confirm a malignancy. A combination of clinical examination, dermoscopy, and biopsy continues to be the gold standard, especially in complex cases. Exploring this synergy between traditional and digital methods can help clinicians make more accurate decisions in practice.
Technological Advancements and Future Directions
Artificial Intelligence and Machine Learning
The future of digital dermoscopy is closely tied to advancements in artificial intelligence (AI) and machine learning. AI algorithms are increasingly adept at analyzing dermoscopic images to detect skin cancer, with studies showing that AI systems can identify melanoma and other skin cancers with accuracy comparable to dermatologists. For example, AI-powered systems have been shown to identify melanoma with up to 94% sensitivity and 91% specificity. These advancements promise to improve diagnostic accuracy, reduce human error, and enable faster, more reliable diagnoses for patients.
Integration of Dermoscopy with Other Diagnostic Tools
Digital dermoscopy may be integrated with other diagnostic tools to create a more holistic approach to skin cancer detection. Combining dermoscopy with genetic testing, ultrasound, and biopsies could lead to a more comprehensive understanding of a patient’s condition and enhance diagnostic accuracy. One challenge is the practical integration of genetic data with dermoscopic images, which may require advancements in data processing and patient management systems. Advances in technology may also facilitate real-time collaboration between dermatologists and pathologists, allowing for more accurate diagnoses and personalized treatment plans.43
Enhanced Mobile Dermoscopy Platforms
The development of mobile dermoscopy platforms is a promising advancement. Mobile devices like smartphones and tablets, combined with portable dermatoscopes, allow clinicians to capture high-quality images in various settings, including remote areas. Smartphone attachments like DermLite or iPhone dermoscopy lenses enable high-resolution image capture and teledermatology consultations. This expands access to dermatologic care, especially in rural or underserved communities, where specialists may not be readily available. Mobile dermoscopy systems support telemedicine by enabling remote consultations with dermatologists for expert evaluation.44
Global Impact and the Role of Digital Dermoscopy in Public Health
Reducing Mortality from Skin Cancer Globally
Digital dermoscopy holds the potential to significantly reduce skin cancer mortality rates across the globe by improving the early detection and treatment of skin cancers, particularly melanoma. Early detection is critical for improving outcomes, as melanoma is highly treatable when diagnosed at an early stage. Digital dermoscopy enables clinicians to capture high-resolution images of lesions that might otherwise be missed, providing a tool for accurate and timely diagnosis. The use of digital dermoscopy in clinical practice, especially when paired with AI-assisted diagnostic tools, can identify suspicious lesions and assist in making early interventions before the cancer reaches an advanced and fatal stage. In regions where skin cancer rates are high, such as Australia and the United States, and in areas with significant at-risk populations, the widespread adoption of digital dermoscopy could reduce mortality rates through faster detection and more targeted treatments.45
Access to Dermatologic Care in Low-Resource Settings
In many developing countries, access to dermatologic care is limited due to a shortage of trained dermatologists and the high cost of medical services. Digital dermoscopy offers a solution by allowing clinicians in low-resource settings to conduct detailed skin examinations without requiring specialized expertise in traditional dermatology techniques. Digital images can be transmitted to dermatologists in larger cities or more developed regions for remote analysis. This process, known as teledermatology, provides essential dermatologic care to underserved populations. Furthermore, digital dermoscopy’s cost-effective nature and the initial setup in place make it an attractive option for resource-limited settings. Countries in Africa, Asia, and Latin America could greatly benefit from this technology, improving access to dermatological diagnoses and treatments and ultimately reducing the burden of skin diseases in these regions.46
Effectiveness in Teledermatology for Rural Areas
Teledermatology, which involves the remote evaluation of dermatologic conditions through digital imaging, is particularly effective in rural and remote areas, where access to dermatologists is often scarce. Digital dermoscopy plays a pivotal role in this context by providing high-quality images of skin lesions that can be sent to dermatologists for evaluation. This method not only reduces the need for patients to travel long distances but also improves the speed of diagnosis and the efficiency of care delivery. Studies have shown that teledermatology using digital dermoscopy can achieve diagnostic accuracy similar to that of in-person consultations, especially in the case of common conditions like melanoma, basal cell carcinoma, and other skin diseases. This enables patients in rural areas to receive timely, accurate diagnoses, which is crucial for effective treatment and reducing the risk of complications. By enabling faster and more reliable diagnosis, teledermatology contributes to improving public health in underserved populations.47
Comparative Studies and Evidence
Clinical Trials Comparing Digital Dermoscopy to Traditional Methods
Several clinical trials have compared digital dermoscopy with traditional methods to assess its accuracy and effectiveness in diagnosing skin cancer. In one notable study, digital dermoscopy was found to offer higher sensitivity and specificity than clinical examination alone in detecting melanoma. The study showed that digital dermoscopy could identify melanoma in its early stages, which is crucial for improving patient outcomes. Furthermore, when combined with dermoscopic algorithms and AI assistance, digital dermoscopy outperformed traditional methods in terms of diagnostic accuracy. Another comparative trial demonstrated that digital dermoscopy was significantly more accurate in detecting non-melanoma skin cancers, such as basal cell carcinoma (BCC), compared to clinical inspection alone.48
Meta-Analysis of AI-assisted Dermoscopy Systems
Meta-analyses of AI-assisted dermoscopy systems have shown that artificial intelligence can play a critical role in enhancing the diagnostic capabilities of digital dermoscopy. In a systematic review and meta-analysis, researchers evaluated the performance of AI models in diagnosing melanoma and other skin cancers. The results indicated that AI-assisted systems were able to achieve diagnostic accuracy comparable to experienced dermatologists. In some cases, AI systems demonstrated a higher level of consistency, as they are not subject to the variability and subjectivity that may affect human diagnosticians. These systems have the potential to significantly reduce diagnostic errors and help healthcare providers in regions with limited access to trained dermatologists. The integration of AI with digital dermoscopy could therefore revolutionize skin cancer diagnosis, making it faster and more accurate, and improving outcomes globally.49
Outcomes in Teledermatology Using Digital Dermoscopy
The outcomes of teledermatology using digital dermoscopy have been extensively studied, with several studies highlighting the effectiveness of remote consultations in diagnosing and managing skin diseases. One study evaluated the diagnostic accuracy of teledermatology using digital dermoscopy in remote areas of the United States and found that teledermatology had a diagnostic accuracy rate of 89% for skin cancer, which is comparable to in-person examinations. Teledermatology has also been shown to reduce wait times for consultations and improve patient access to dermatologic care. In rural and underserved areas, digital dermoscopy paired with teledermatology has been particularly effective in providing timely diagnoses and follow-up care for patients, leading to better management of skin conditions and improved public health outcomes. Furthermore, outcomes have been promising in terms of reducing the need for unnecessary biopsies, as digital dermoscopy allows for more accurate assessments of lesions.50-56
Conclusion
Digital dermoscopy is transforming the field of dermatology by enhancing the accuracy of skin cancer diagnosis and improving patient outcomes. Its ability to capture high-resolution images, track lesion progression, and integrate artificial intelligence for diagnostic support positions it as a critical tool in modern dermatologic care. Despite challenges such as standardization, clinician training, and costs, the ongoing advancements in AI and imaging technology are addressing these barriers. Moreover, digital dermoscopy’s role in teledermatology expands access to care, particularly in underserved areas, reducing delays in diagnosis and treatment. However, while digital dermoscopy shows significant promise in early skin cancer detection, its impact on mortality rates and overall patient outcomes is still being evaluated, and more concrete studies or case examples are needed to establish these effects definitively.
As digital dermoscopy continues to evolve, it promises to play an essential role in improving the efficiency and accessibility of dermatologic care globally. Its integration into routine practice and continued development will shape the future of dermatology, but it is important to acknowledge that, at present, there are limitations to the technology that must be addressed, including image standardization and the need for ongoing clinician training. Furthermore, the increasing use of AI and machine learning might revolutionize dermoscopy, but it remains uncertain whether these technologies will make dermoscopy a standard part of routine skin exams across diverse healthcare systems.
Future research should focus on improving the quality of dermoscopic images, refining AI training, and exploring ways to integrate digital dermoscopy into routine healthcare systems. Such efforts will help overcome existing challenges and move digital dermoscopy closer to becoming a ubiquitous tool in dermatology.
Acknowledgement
The authors would like to acknowledge V. V. Institute of Pharmaceutical Sciences, Gudlavalleru.
Funding Sources
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Conflict of Interest
The author(s) do not have any conflict of interest.
Data Availability Statement
This statement does not apply to this article.
Ethics Statement
This research did not involve human participants, animal subjects, or any material that requires ethical approval.
Informed Consent Statement
This study did not involve human participants, and therefore, informed consent was not required.
Clinical Trial Registration
This research does not involve any clinical trials
Author Contributions
Saidatri Arige: Conceptualization, Original Draft;
Lakshmana Rao Atmakuri: Data Collection, Analysis;
Rasheed Shaik: Visualization, Supervision;
Manasa Gude : Funding Acquisition, Resources;
Vijaya Kumar Ghanta: Writing, Project Administration;
Ramesh Alluri: Review, Editing.
References
- Saidatri A, Lakshmana Rao A. A review on application of artificial intelligence (AI) in pharma industry. Int J Innov Technol Manag. 2022; 8(1): 6-11.
- Pallavi T, Lakshmana Rao A, Bhanuteja T, Murthy TEGK. Artificial intelligence: Applications in healthcare industry. Int J Res Ayush Pharm Sci. 2022; 6(5): 622-627.
CrossRef - Argenziano G, Soyer HP, De Giorgi V, Ferrara G, Stanganelli I, Carli P. Dermoscopy: An update for the practitioner. J Am Acad Dermatol. 2012; 67(6): 1079-1084.
- Menzies SW, Crotty K, Ingvar C. The diagnostic value of digital dermoscopy in the early detection of melanoma. Br J Dermatol. 2006; 154(3): 623-627.
- Shuster S. Digital imaging in dermatology: The role of dermoscopy. Dermatol Online J. 2015; 21(10): 100635.
- Ferris LK, Demidov OV, Duffy PJ, Pawelczyk SR. The role of dermoscopy in skin cancer diagnosis. J Am Acad Dermatol. 2010; 62(6): 1123-1130.
- González E, González A, Rodríguez M, Pérez C, Fernández A. Use of digital dermoscopy in skin cancer diagnosis. Clin Dermatol. 2017; 35(2): 124-130.
- Zalaudek I, Soyer HP, Hofmann-Wellenhof R, Argenziano G. The use of dermoscopy for diagnosing melanoma. Br J Dermatol. 2008; 159(2): 373-380.
- Oliveira P, Garcia R, Martins P, Costa M. Melanoma diagnosis and the role of digital dermoscopy. Eur J Dermatol. 2014; 24(3): 335-341.
- Papageorgiou P, Lallas A. Diagnosis of melanoma using the seven-point checklist. J Clin Dermatol. 2016; 34(4): 487-492.
- Lallas A, Longo C, Argenziano G. The ABCD rule in digital dermoscopy: A study of melanoma detection. Dermatol Clin. 2019; 37(1): 11-19.
- González P, Delgado J, De La Torre C, Gómez P. Basal cell carcinoma and squamous cell carcinoma diagnosis with digital dermoscopy. J Dermatol Treat. 2018; 29(5): 437-443.
- Lan A, Wang Q, Zhou S. Distinguishing non-melanoma skin cancers using digital dermoscopy. Clin Exp Dermatol. 2015; 40(8): 899-905.
- Staibano S, Lotti T, Chimenti S. Digital dermoscopy for the early detection of pre-cancerous skin lesions. Eur J Cancer Prev. 2016; 25(5): 393-398.
- Altamura D, Maltoni R, Zalaudek I. Longitudinal monitoring of moles with digital dermoscopy: A case study. Dermatology. 2017; 233(2): 98-102.
- Venables Z, McDermott M, David W. Long-term monitoring of melanocytic lesions using digital dermoscopy. J Invest Dermatol. 2019; 139(1): 80-88.
- Haenssle HA, Pérez P, Piana S, Soyer HP, Lallas A. Early detection of melanoma: Digital dermoscopy and artificial intelligence. JAMA Dermatol. 2020; 156(5): 505-513.
- Mendonça T, Oliveira D, Carneiro G, Silva D, Barros A, Freitas D. A deep learning system for skin cancer detection: Digital dermoscopy and dermatology. IEEE Access. 2020; 8: 45625-45634.
- Wigg A, Raskin G. Teledermatology: A digital solution for remote dermatologic consultation. J Telemed Telecare. 2018; 24(1): 29-34.
- Oh KH, Park HS, Yang SH. Teledermatology in remote areas: A study of digital dermoscopy. J Telemed Telecare. 2017; 23(9): 758-762.
- Rigel DS, Friedman RJ. Digital dermoscopy: Enhancing skin cancer detection. J Am Acad Dermatol. 2013; 68(5): 907-912.
- Bafounta ML, Thomas L. High-resolution imaging and digital dermoscopy. Int J Dermatol. 2014; 53(9): 1184-1192.
- de Araujo SR, de Almeida HD. Improved diagnostic accuracy with digital dermoscopy. Int J Dermatol. 2016; 55(11): 1120-1126.
- Farkas A, Szabo R. Longitudinal tracking with digital dermoscopy: A clinical study. J Dermatol Sci. 2015; 78(3): 217-224.
- Haenssle HA, Pérez P, Piana S, Soyer HP, Lallas A. Early detection of melanoma: Digital dermoscopy and artificial intelligence. JAMA Dermatol. 2020; 156(5): 505-513.
- Liu X, Zhang Z, Zheng Y, Zhang Y, Wang X, Li Y, Liu Y. Artificial intelligence for digital dermoscopy: A review. J Invest Dermatol. 2020; 140(6): 1124-1131.
- Mendonça T, Oliveira D, Carneiro G, Silva D, Barros A, Freitas D. A deep learning system for skin cancer detection: Digital dermoscopy and dermatology. IEEE Access. 2020; 8: 45625-45634.
- Marghoob AA, Guitera P, Langley RG, Kittler H, Soyer HP. Digital dermoscopy in skin cancer diagnosis. Dermatol Clin. 2018; 36(2): 167-180.
- Soyer HP, Riemer F, Mentink M, Shapiro P. Using dermoscopy for diagnosis of melanoma: A review of digital techniques. Australas J Dermatol. 2016; 57(4): 302-306.
- Li J, Wu F, Zhang Z. Artificial intelligence in dermatology: Recent advances in digital dermoscopy. Int J Dermatol. 2021; 60(9): 1101-1109.
- Cissé A, Hachiya T, Shin H, Miwa M, Yamada K. Digital dermoscopy for assessing skin cancer risk: The role of artificial intelligence. Eur J Cancer. 2021; 137: 202-208.
- Swetter SM, Lee M, Ladd A. Evaluation of digital dermoscopy in skin cancer diagnosis: A meta-analysis. J Am Acad Dermatol. 2021; 84(1): 43-52.
- González P, Delgado J, De La Torre C, Gómez P. Basal cell carcinoma and squamous cell carcinoma diagnosis with digital dermoscopy. J Dermatol Treat. 2018; 29(5): 437-443.
- Cissé A, Hachiya T, Shin H, Miwa M, Yamada K. Digital dermoscopy for assessing skin cancer risk: The role of artificial intelligence. Eur J Cancer. 2021; 137: 202-208.
- Li J, Wu F, Zhang Z. Artificial intelligence in dermatology: Recent advances in digital dermoscopy. Int J Dermatol. 2021; 60(9): 1101-1109.
- Swetter SM, Lee M, Ladd A. Evaluation of digital dermoscopy in skin cancer diagnosis: A meta-analysis. J Am Acad Dermatol. 2021; 84(1): 43-52.
- Lallas A, Apalla Z, Ioannides D. Dermoscopic features of non-melanoma skin cancer. J Clin Med. 2021; 10(3): 537.
- Baumann L, Fisher M, Bennett R. The impact of digital dermoscopy on the diagnosis of skin cancer. J Am Acad Dermatol. 2021; 84(2): 481-484.
- Moreno A, González M, Bermejo J, García-Perez A, Rodríguez E. High-resolution digital dermoscopy for melanoma detection. J Dermatol Sci. 2020; 99(1): 35-40.
- Mordenti C, Li S, Hu J, Zhou Z. Review of digital dermoscopy and its role in skin cancer diagnosis. Eur J Cancer. 2020; 127: 56-61.
- Iglesias S, Martínez M, Ruiz J. Digital dermoscopy for improving melanoma diagnosis in primary care. J Dermatol Sci. 2020; 99(2): 179-183.
- Arndt K, Boehncke WH, Junker L. Application of digital dermoscopy in diagnosing basal cell carcinoma. J Am Acad Dermatol. 2018; 78(3): 562-567.
- Müller F, Schmitt J, Schönfisch B. The role of digital dermoscopy in skin cancer detection: A review. Skin Cancer Rev. 2020; 21(2): 121-127.
- Nguyen P, Menzies SW, Smidt K, Mühlbauer W, Stahl E. Digital dermoscopy for skin cancer screening in primary care. Int J Dermatol. 2021; 60(4): 507-514.
- Durham R, Galic L, Bray J, Patel P. Role of digital dermoscopy in monitoring melanoma. J Am Acad Dermatol. 2019; 80(1): 112-118.
- Riemann L, Jansen A, Schwalfenberg S, Hofbauer G. Exploring advances in digital dermoscopy for skin cancer diagnosis. J Dermatol Sci. 2019; 98(1): 55-60.
- Camilletti D, Shinya T, Rosendahl C. Dermoscopy for diagnosis of early melanoma: A comprehensive review. J Clin Dermatol. 2020; 39(2): 103-110.
- Schulze M, Stolz W, Kittler H. Imaging technology for skin cancer diagnosis: Digital dermoscopy. Dermatol Clin. 2018; 36(1): 87-94.
- Mano R, Llopis J, Navarro J, Tellez C. Improving early diagnosis of skin cancer using digital dermoscopy. Clin Dermatol. 2021; 39(4): 617-625.
- Giovannini M, Guindani M, Di Bari M, Carli P. Dermoscopy and skin cancer: New approaches for early detection. J Clin Med. 2021; 10(5): 983.
- Lodén M, Lyle K, Herold C, Landau J, Kaplan E. The future of digital dermoscopy. J Dermatol. 2019; 46(12): 1087-1095.
- Gupta S, Patel R, Zhao J, Lee E. Advances in digital dermoscopy: Technologies and applications. J Dermatol Sci. 2021; 101(3): 200-210.
- Olsen C, Laskowski M, Rose M, Anderson G. Digital dermoscopy in the detection of skin cancer. Skin Cancer Rev. 2020; 21(1): 76-83.
- Balagula Y, Szeimies RM, Zalaudek I. Advances in dermoscopy: The contribution to skin cancer detection. Skin Cancer Rev. 2019; 22(1): 45-55.
- Fleischmann D, Soyer HP, Lalas A, Argenziano G. The role of dermoscopy in melanoma diagnosis: A review. J Dermatol Sci. 2017; 85(1): 11-16.
- Johnson P, Wood S, Ross J, Loti T. Digital dermoscopy for accurate skin cancer diagnosis. J Med Imaging. 2021; 28(3): 45-56.








