Manuscript accepted on :19-02-2024
Published online on: 19-03-2024
Plagiarism Check: Yes
Reviewed by: Dr. Miss Mais Salim Saadallah and Dr. Ankit Chowdhury
Second Review by: Dr. Fatma Çavuş Yonar
Final Approval by: Dr. Luis Jesús Villarreal-Gómez
Shuaibu Abdullahi Hudu1* , Abdulgafar Olayiwola Jimoh2
, Abdulgafar Olayiwola Jimoh2 , Aiman Alqtaitat1,3
, Aiman Alqtaitat1,3 and Fayig E-lmigdadi1
and Fayig E-lmigdadi1
1Department of Basic Medical and Dental Sciences, Faculty of Dentistry, Zarqa University, Zarqa 13110, Jordan
2Department of Pharmacology and Therapeutics, Faculty of Basic Clinical Sciences, College of Health Sciences, Usmanu Danfodiyo University, Sokoto, 840232 Sokoto State, Nigeria
3Department of Anatomy and Histology, Faculty of Medicine, Mutah University, Karak 61710, Jordan
Corresponding Author E-mail: shudu@zu.edu.jo
DOI : https://dx.doi.org/10.13005/bpj/2829
Abstract
Infectious diseases continue to pose a persistent threat to public health globally. Amidst the array of factors contributing to the complexity of infectious disease outbreaks, the role of seasonal influenza stands out as a significant amplifier. Seasonal influenza, commonly known as the flu, not only inflicts its burden on communities but also plays a crucial role in compounding the spread and impact of other infectious diseases. This review delves into the various ways in which seasonal influenza contributes to the complexity of infectious disease outbreaks. The role of seasonal influenza in compounding the outbreak of infectious diseases is a multifaceted challenge that demands attention from public health authorities worldwide. Addressing this compounding effect requires a holistic approach that encompasses vaccination campaigns, strengthened healthcare infrastructure, and improved diagnostic capabilities. By understanding and mitigating the various ways in which seasonal influenza contributes to the complexity of infectious disease outbreaks, communities can enhance their resilience and responsiveness in the face of evolving public health threats. Recognizing and understanding these dynamics is essential for designing effective public health strategies. By implementing comprehensive vaccination programs, improving diagnostic capabilities, and enhancing overall preparedness, communities can better navigate the complexities of infectious disease outbreaks exacerbated by the presence of seasonal influenza.
Keywords
Compounding; Diseases; Flu; Infection; Outbreak; Seasonal
Download this article as:| Copy the following to cite this article: Hudu S. A, Jimoh A. O, Alqtaitat A, E-lmigdadi F. The Role of Seasonal Influenza in Compounding the Outbreak of Infectious Diseases: A Critical Review. Biomed Pharmacol J 2024;17(1). |
| Copy the following to cite this URL: Hudu S. A, Jimoh A. O, Alqtaitat A, E-lmigdadi F. The Role of Seasonal Influenza in Compounding the Outbreak of Infectious Diseases: A Critical Review. Biomed Pharmacol J 2024;17(1). Available from: https://bit.ly/3Vjbpyg |
Introduction
Infectious diseases pose a significant threat to global public health, and various factors often exacerbate their impact. One such influential factor is the seasonal influenza virus, which not only presents a substantial health challenge but also plays a pivotal role in compounding the outbreak and spread of other infectious diseases1. Seasonal influenza, commonly known as the flu, is a highly contagious respiratory infection caused by influenza viruses which typically manifests with symptoms such as fever, cough, sore throat, and muscle aches2. While the influenza virus is a significant health concern in itself, its role in exacerbating the impact of other infectious diseases cannot be understated as the seasonal nature of influenza creates a recurrent challenge for healthcare systems worldwide 3. The virus tends to peak during specific periods, placing additional strain on healthcare resources and personnel. As these resources are diverted to manage influenza cases, the capacity to effectively respond to other infectious diseases diminishes, creating an environment conducive to the rapid spread of additional pathogens4.Furthermore, the immunomodulatory effects of influenza can compromise individuals’ immune responses, rendering them more susceptible to secondary infections. The influenza virus weakens the immune system by interfering with the body’s ability to mount an effective defence against pathogens5,6. This immune suppression not only prolongs the recovery from influenza itself but also heightens the risk of acquiring and spreading other infectious diseases. For instance, individuals infected with influenza may experience damage to the respiratory epithelium, creating an entry point for opportunistic pathogens7,8. Bacterial co-infections, such as pneumonia, are common complications of influenza and significantly contribute to the severity of illness and mortality rates9.
The interplay between influenza and secondary infections underscores the importance of comprehensive vaccination strategies and prompt medical interventions to mitigate the compounding effects on public health10,11. Moreover, the similarities in symptoms between influenza and various other respiratory infections can pose challenges in timely and accurate diagnosis. Amid an influenza outbreak, distinguishing between influenza and emerging infectious diseases becomes a formidable task for healthcare professionals. This diagnostic challenge delays appropriate treatment and containment measures, allowing the co-occurrence of multiple infectious diseases to escalate within communities. Addressing the compounding role of seasonal influenza in infectious disease outbreaks requires integrated public health strategies. Comprehensive influenza vaccination campaigns, strengthened surveillance systems, and robust healthcare infrastructure are essential components of a proactive approach12. Timely and accurate diagnosis, coupled with effective treatment protocols, can minimize the impact of influenza on individuals and prevent the synergistic effects of other infectious diseases. Therefore, this review provides an insight into the various ways in which seasonal influenza contributes to the complexity of infectious disease outbreaks.
Healthcare system overload
Infectious disease outbreaks pose significant challenges to healthcare systems worldwide with a sudden surge in cases, the need for rapid response, and the strain on resources can lead to healthcare system overload13. One of the primary mechanisms through which seasonal influenza compounds infectious disease outbreaks is by straining healthcare systems.10 The cyclical nature of influenza creates annual spikes in cases, leading to a surge in hospital admissions and outpatient visits14,15. The increased demand for medical resources, personnel, and treatment facilities during flu seasons diverts attention and resources away from addressing other emerging infectious diseases. As healthcare providers grapple with the influx of influenza cases, their ability to effectively respond to concurrent outbreaks diminishes, creating a domino effect that hampers overall public health response capabilities16,17. Infectious disease outbreaks, particularly those with high transmission rates, can deplete essential medical resources18,19. Personal protective equipment (PPE), ventilators, medications, and diagnostic tools become scarce, affecting the quality of care provided to patients20. Healthcare personnel face increased workloads, long hours, and heightened stress, potentially compromising their ability to deliver optimal care. Staff shortages, whether due to illness or burnout, exacerbate the strain on the healthcare workforce. Outbreaks can present logistical challenges in managing patient flow and maintaining infection control measures21. Designated isolation areas, intensive care units, and other critical spaces may become overwhelmed, hindering the ability to segregate infected individuals from the general population22. Limited space and facilities contribute to the difficulties in implementing effective triage, isolation, and treatment strategies23.
During infectious disease outbreaks, the focus on treating infected individuals can lead to delays in providing care for non-infectious conditions such as routine medical procedures, elective surgeries, and treatments for chronic illnesses that may be postponed or cancelled24,25. Patients with conditions unrelated to the outbreak may face challenges accessing timely and appropriate healthcare services, potentially leading to adverse health outcomes26. Effective communication is paramount during infectious disease outbreaks, both within the healthcare system and with the public. Overload can strain communication channels, leading to delays in disseminating critical information to healthcare providers, patients, and the broader community27. Misinformation and a lack of clear communication can contribute to panic, fear, and a breakdown in public trust28. Miscommunication can lead to panic, misinformation, and a loss of public trust, further complicating the healthcare system’s ability to manage the outbreak effectively. Recurring infectious disease outbreaks can erode the overall resilience of healthcare systems and if the systems are consistently stretched to their limits without sufficient recovery periods, they become more vulnerable to subsequent crises29. Long-term strain can result in a diminished capacity to handle future outbreaks, exacerbating the potential for healthcare system overload during infectious disease outbreaks with wide-ranging implications30.
Healthcare personnel face unprecedented challenges during infectious disease outbreaks because their increased workload, prolonged working hours, and exposure to high-stress situations contribute to burnout among healthcare professionals31,32. Staff shortages, whether due to illness among healthcare workers or an overwhelmed workforce, further compound the strain on the healthcare system33. The mental health and well-being of healthcare workers become critical considerations in maintaining a functional healthcare response amid an infectious disease outbreak, routine healthcare services are often disrupted34. Elective surgeries, preventive screenings, and management of chronic illnesses may be postponed or cancelled to redirect resources and personnel toward addressing the outbreak leading to delayed diagnoses, progression of chronic conditions, and long-term health consequences for individuals not directly affected by the infectious disease35,36. The disruption of healthcare systems during infectious disease outbreaks is a multifaceted challenge that requires careful planning, resource allocation, and effective communication. Building resilient healthcare systems that can adapt to surges in demand, ensuring a robust supply chain for medical resources, and prioritizing the well-being of healthcare workers are crucial components of mitigating the disruption caused by infectious disease outbreaks. A comprehensive and coordinated approach is essential to minimize the impact on patient care and protect public health during these challenging times.
Immune compromise and co-infections
In the context of infectious disease outbreaks, the compromised immune status of individuals can significantly impact the course and severity of infections37. Immune compromise may result from various factors, including the primary infectious agent, coexisting health conditions, or treatments received.38 Seasonal influenza can compromise the immune system, making individuals more susceptible to secondary infections because the virus weakens the respiratory epithelium, creating an opportune environment for other pathogens to invade39. Bacterial co-infections, particularly pneumonia, frequently accompany influenza cases, contributing to increased morbidity and mortality rates40. This synergy between influenza and secondary infections underscores the importance of addressing not only the primary infection but also its potential cascading effects on overall health. Seasonal influenza has immunomodulatory effects that can compromise the immune response of individuals as the virus weakens the respiratory epithelium, creating a favourable environment for opportunistic infections41,42. Individuals infected with influenza become more susceptible to secondary bacterial infections, such as pneumonia which increased the susceptibility not only prolongs the recovery from influenza but also escalates the severity of other infectious diseases that may co-occur, leading to a compounding effect on overall public health42,43. Infectious diseases, particularly those affecting the respiratory system, can compromise the integrity of the respiratory epithelium which serves as an entry point for opportunistic pathogens, leading to co-infections44. In the context of outbreaks like influenza or COVID-19, the initial viral infection may damage the respiratory epithelium, facilitating secondary bacterial infections such as pneumonia while co-infections often result in more severe clinical outcomes and increased mortality rates45. Individuals with pre-existing health conditions, such as diabetes, cardiovascular disease, or immunodeficiency disorders, are often more susceptible to infectious diseases and also the presence of chronic illnesses can compromise the immune system’s ability to mount an effective defence against pathogens46. During outbreaks, individuals with underlying health conditions may experience more severe forms of the primary infection and are at an increased risk of acquiring co-infections47.
Similarly, medical interventions used to treat infectious diseases, such as immunosuppressive drugs or certain antiviral therapies, can induce immune suppression48. While these treatments are essential for managing the primary infection, they may inadvertently increase the risk of co-infections. Striking a balance between controlling the outbreak and minimizing treatment-induced immune compromise is a delicate challenge in infectious disease management. Co-infections in the context of immune compromise often result in more severe clinical outcomes that can lead to a synergistic effect, causing a more profound and prolonged illness49,50. This poses challenges for healthcare providers in terms of treatment strategies, as managing co-infections requires a comprehensive and tailored approach to address the unique aspects of each pathogen. Vaccination campaigns targeting both the primary infectious agent and common secondary pathogens can mitigate the risk of co-infections. However, public health strategies should consider the vulnerability of specific populations, such as individuals with chronic illnesses or those undergoing immune-suppressive treatments, to tailor interventions and preventive measures accordingly25. Infectious disease outbreaks create a complex landscape where immune compromise significantly influences the dynamics of co-infections. Recognizing the interplay between the primary infectious agent, compromised immune responses, and secondary pathogens is essential for designing effective control strategies. By addressing immune compromise in the context of outbreaks, public health efforts can better protect vulnerable populations and mitigate the impact of co-infections on overall morbidity and mortality51,52.
Diagnostic challenges and delayed intervention
In the context of infectious disease outbreaks, timely and accurate diagnosis is critical for effective control and management. However, the complex nature of outbreaks often introduces diagnostic challenges, leading to delayed intervention as shown in Table 1. The overlap in symptoms between influenza and various other infectious diseases presents a challenge in timely and accurate diagnosis53. During an influenza outbreak, the similarity in clinical presentations hampers the ability to differentiate between influenza and emerging pathogens54. The lack of prompt and precise diagnostic tools may result in delayed interventions and the inadvertent facilitation of the concurrent spread of multiple infectious agents within communities. Timely diagnosis is crucial for effective containment measures, and the failure to promptly identify and isolate cases contributes to the compounding effect of infectious diseases. One of the primary reasons for diagnostic challenges in infectious disease outbreaks is the similarity in clinical presentations among different pathogens55. Many infectious diseases share common symptoms, such as fever, cough, and fatigue, making it difficult to differentiate between them based solely on clinical observation55,56. This lack of specificity hampers healthcare professionals’ ability to quickly and accurately identify the causative agent, delaying appropriate intervention. During the early stages of an outbreak, access to rapid and reliable diagnostic tools may be limited.
Table 1: An outline of the diagnostic challenges and potential delays in intervention during disease outbreaks.
|
Diagnostic Challenge |
Description |
Delayed Intervention Consequences |
References |
|
Asymptomatic Cases |
Difficulty in identifying individuals who are carriers of the disease but show no symptoms. |
Spread of the disease within communities as asymptomatic carriers unknowingly transmit the infection. |
57 |
|
Limited Access to Testing |
Insufficient availability of diagnostic tests, leading to delays in confirming cases. |
Delayed identification of infected individuals, hindering timely isolation, contact tracing, and treatment. |
58 |
|
Symptom Similarity |
Similar symptoms with other common illnesses may lead to misdiagnosis or delayed recognition. |
Delayed initiation of appropriate treatment and increased risk of secondary transmission due to undetected cases. |
59 |
|
Variable Incubation Periods |
Different individuals may exhibit varying incubation periods, making it challenging to predict onset. |
Difficulties in determining the optimal timing for intervention measures such as quarantine and contact tracing. |
60 |
|
Limited Healthcare Infrastructure |
Inadequate resources and healthcare facilities may hinder rapid diagnostic processes. |
Overwhelmed healthcare systems, increased patient load, and reduced capacity to respond effectively to the outbreak. |
61 |
|
Inadequate Surveillance Systems |
Lack of robust monitoring systems may result in delayed detection of unusual patterns. |
Delayed recognition of outbreaks, hinders the ability to implement timely public health measures and control the spread of the disease. |
62 |
|
Globalization and Travel |
Increased international travel may lead to delayed identification of cases in different regions. |
Global spread of the disease, making containment and control efforts more challenging. |
63 |
|
Stigma and Fear |
Social stigma and fear associated with the disease may lead to underreporting and delayed seeking of healthcare. |
Increased risk of community transmission as individuals may avoid testing or treatment due to fear of discrimination or isolation. |
64 |
|
Insufficient Public Awareness |
Lack of awareness about symptoms, preventive measures, and available resources. |
Delayed reporting of symptoms, leads to delays in seeking healthcare and implementation of preventive measures. |
65 |
|
Laboratory Capacity Issues |
Inadequate laboratory facilities and trained personnel for timely and accurate testing. |
Delays in confirming cases hindered contact tracing and challenges in implementing appropriate control measures. |
67 |
Developing and deploying diagnostic tests for a novel pathogen can take time, and in resource-constrained settings, the availability of such tests may be further delayed. The absence of point-of-care diagnostics contributes to delays in confirming cases, isolating individuals, and implementing targeted public health measures. Infectious disease outbreaks often occur in regions with limited healthcare infrastructure and resources. Logistical challenges, including transportation of samples, establishing testing centres, and ensuring a reliable supply chain for diagnostic reagents, can contribute to delays in the testing process68,69. The lack of a robust infrastructure impedes the rapid scaling-up of diagnostic capabilities during an outbreak. Some diagnostic tests may have inherent limitations, including high false-negative rates, especially during the early stages of infection70. False-negative results can lead to an underestimation of the true extent of the outbreak, contributing to delayed intervention71. Therefore, the need for confirmatory testing and retesting individuals with initial negative results further complicates the diagnostic process. The effectiveness of outbreak response relies on robust surveillance and reporting systems72. In regions where surveillance infrastructure is inadequate or reporting mechanisms are inefficient, delays in identifying and reporting cases occur73. This lack of real-time data compromises the ability of public health authorities to implement timely and targeted interventions, allowing the outbreak to escalate. Public awareness and the stigma associated with infectious diseases can also contribute to delayed intervention as such, individuals may be hesitant to seek medical attention due to fear of social isolation or discrimination74,75. This delay in seeking care not only impacts the affected individuals but also allows the infectious agent to spread further within communities before appropriate interventions can be implemented.
In an interconnected world, delayed sharing of information between countries and regions can impede the global response to infectious disease outbreaks76. Political, logistical, or diplomatic challenges may hinder the timely exchange of data, hindering the international community’s ability to coordinate efforts and deploy resources effectively 77,78. Diagnostic challenges and delayed intervention in infectious disease outbreaks are multifaceted issues that require a comprehensive and coordinated response. Addressing these challenges necessitates investment in rapid and accurate diagnostic technologies, strengthening healthcare infrastructure, improving surveillance systems, and promoting global cooperation for timely information sharing. By addressing these factors, public health authorities can enhance their capacity to identify, respond to, and control infectious disease outbreaks in a more effective and timely manner.
Public health strategies and preparedness
Infectious disease outbreaks pose significant threats to public health, requiring comprehensive strategies and preparedness measures for effective prevention, control, and response79. The compounding effect of seasonal influenza on infectious disease outbreaks emphasizes the need for robust public health preparedness as outlined in Figure 1. Comprehensive vaccination programs targeting influenza can significantly reduce the incidence and severity of flu cases, alleviating the burden on healthcare systems 80. Addressing the compounding role of seasonal influenza requires a comprehensive approach to public health strategies and preparedness81. Strengthening surveillance systems and diagnostic capabilities is essential for differentiating between influenza and other infectious diseases promptly. Furthermore, integrated public health planning that considers the seasonal patterns of influenza can enhance overall readiness to respond to emerging infectious diseases82. Timely surveillance and early detection are fundamental to managing infectious disease outbreaks because robust surveillance systems, incorporating real-time data collection and analysis, enable public health authorities to identify and monitor emerging threats swiftly83. This includes monitoring unusual patterns of illness, conducting sentinel surveillance, and utilizing advanced technologies for rapid detection of pathogens84. Early detection facilitates prompt intervention, containment, and the prevention of further transmission. In an interconnected world, global collaboration and establishing international networks and partnerships allow for the exchange of data, resources, and expertise. Organizations such as the World Health Organization (WHO) play a central role in coordinating global responses, facilitating research, and providing guidance to nations facing infectious disease threats. Transparent and effective communication with the public is critical during infectious disease outbreaks. Public health authorities must provide accurate information about the nature of the outbreak, preventive measures, and the current state of affairs. Engaging with communities fosters trust, encourages compliance with public health recommendations, and dispels misinformation. Effective risk communication helps mitigate fear and panic, promoting a collective and informed response 85.
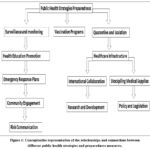 |
Figure 1: Conceptualize representation of the relationships and connections between different public health strategies and preparedness measures. |
Vaccination is a cornerstone of infectious disease prevention and control. Public health strategies should include comprehensive vaccination campaigns, targeting both routine immunizations and specific vaccines for emerging threats. Ensuring high vaccine coverage in populations helps establish herd immunity, reducing the overall transmission of infectious agents and protecting vulnerable individuals86. Building and maintaining the capacity of healthcare systems to handle infectious disease outbreaks is crucial and includes training healthcare professionals, ensuring an adequate supply of medical resources, and establishing surge capacity for increased patient numbers87. Resource allocation should be flexible, allowing for rapid mobilization of personnel, equipment, and facilities to areas experiencing outbreaks. Implementation of quarantine and isolation measures is essential for controlling the spread of infectious diseases which helps in identifying and isolating individuals with confirmed or suspected infections, along with contact tracing, helps break the chain of transmission88. Public health authorities must have clear guidelines for implementing these measures while minimizing the social and economic impact on affected individuals and communities. Investment in research and development for therapeutics and diagnostics is pivotal for enhancing preparedness. The availability of effective treatments and diagnostic tools expedites patient care, facilitates early identification of cases, and informs public health responses89. Collaboration between public and private sectors, as well as academia, will accelerate the development of innovative solutions. Emergency preparedness plans should be in place, outlining clear roles and responsibilities at local, regional, and national levels as well as conducting regular drills and exercises to ensure that the response mechanisms are well-practiced and can be efficiently implemented when needed. Effective public health strategies and preparedness are indispensable for managing infectious disease outbreaks90. Communities and nations can enhance their resilience and ability to respond swiftly to emerging infectious threats by implementing robust surveillance, fostering global collaboration, communicating transparently with the public, and investing in research and development.
Seasonal influenza and covid-19 outbreak
The COVID-19 pandemic has brought unprecedented challenges to global public health, and understanding the compounding effects of seasonal influenza on the COVID-19 outbreak is crucial10. Seasonal influenza, a recurring respiratory infection, adds complexity to the dynamics of the unending pandemic. Studies have shown that seasonal influenza serves as a compounding factor in the COVID-19 outbreak, impacting various aspects of public health response and individual well-being 91. One of the most significant ways seasonal influenzas compound the COVID-19 outbreak is by placing an additional burden on healthcare systems. Both infections share similar symptoms, leading to an increase in hospital admissions and diagnostic challenges. The co-occurrence of influenza and COVID-19 cases strains medical facilities, exacerbating shortages in resources such as hospital beds, ventilators, and medical personnel. This strain compromises the ability of healthcare systems to effectively manage and respond to the surge in respiratory infections92. Seasonal influenza and COVID-19 disproportionately affect similar high-risk groups, including the elderly and individuals with underlying health conditions. The coexistence of these infections places these vulnerable populations at an elevated risk of severe illness and complications. The shared susceptibility among high-risk groups underscores the importance of targeted public health interventions, such as vaccination campaigns, to mitigate the impact of both influenza and COVID-19.
The overlapping symptoms of seasonal influenza and COVID-19 create diagnostic challenges, leading to delays in identifying and isolating cases thereby stretching testing infrastructure and resources when faced with the dual challenge of diagnosing both respiratory infections93. This diagnostic complexity hampers timely interventions, allowing the viruses to spread within communities. Swift and accurate identification of cases is critical for implementing effective containment measures and preventing further transmission of both influenza and COVID-19. The presence of seasonal influenza alongside the COVID-19 outbreak can complicate individual and public perceptions of illness94. Distinguishing between the two infections based solely on symptoms is challenging, leading to increased anxiety and uncertainty. This confusion may contribute to the hesitancy in seeking medical attention, delayed testing, and adherence to public health guidelines. Vaccination campaigns become even more crucial during the co-occurrence of seasonal influenza and the COVID-19 outbreak95. Vaccinating against influenza helps reduce the overall burden on healthcare systems, minimizes the severity of flu cases, and prevents potential co-infections with COVID-1996. Coordinated efforts to promote influenza vaccination alongside COVID-19 vaccination will contribute to enhancing community resilience and reducing the strain on healthcare resources.
Expert opinion on mitigating the effect of seasonal influenza on disease outbreak
Seasonal influenza poses a significant public health challenge, contributing to the burden of infectious diseases worldwide. A comprehensive approach is essential to mitigate its impact on public health and prevent the escalation of larger outbreaks. One of the most effective ways to mitigate the impact of seasonal influenza is through widespread vaccination campaigns. Annual vaccination, especially targeting vulnerable populations, serves as a crucial preventive measure. Governments and healthcare organizations must invest in public awareness campaigns to educate individuals about the benefits of vaccination. By increasing vaccine coverage, the overall burden of influenza cases can be reduced, preventing the virus from spreading rapidly within communities. Implementing robust public health measures is vital for controlling the spread of influenza and minimizing its impact on infectious disease outbreaks. Surveillance and monitoring systems should be strengthened to detect influenza outbreaks early. Isolation and quarantine measures can help contain the virus, while social distancing strategies can reduce person-to-person transmission. Promoting hygiene practices, such as regular handwashing and respiratory etiquette, is essential to prevent the spread of influenza in various settings.
Enhancing the preparedness of healthcare systems is critical to handle the seasonal influx of influenza cases effectively. This involves increasing healthcare facility capacity, ensuring a sufficient supply of antiviral medications, and improving communication channels between healthcare providers and public health agencies. Timely and accurate information dissemination is crucial for managing resources efficiently and providing appropriate care to individuals affected by influenza. Educating the public about influenza prevention is a cornerstone in the fight against its spread. Public awareness campaigns should convey the importance of vaccination, personal hygiene practices, and early symptom recognition. Workplace education programs can play a role in preventing the spread of influenza in professional settings. By fostering a culture of awareness, individuals are better equipped to protect themselves and their communities. In the interconnected world of today, international collaboration is indispensable for mitigating the effects of seasonal influenza. Countries should work together to share information on influenza trends, coordinate response efforts, and collectively address challenges associated with the virus. Collaborative research initiatives can lead to the development of more effective vaccines and treatments, benefiting global public health.
Investment in research and development is paramount for staying ahead of the influenza virus. Ongoing surveillance of influenza strains, coupled with research into novel vaccines and antiviral medications, ensures a proactive rather than reactive approach to the evolving nature of the virus. Governments, academic institutions, and pharmaceutical companies should collaborate to drive innovation in influenza prevention and treatment. Engaging communities in the mitigation of seasonal influenza is essential for building resilience. Communities should be active participants in the development and implementation of preventive measures. By fostering a sense of collective responsibility, individuals are more likely to adhere to recommended practices and contribute to the overall success of influenza prevention strategies. Mitigating the impact of seasonal influenza on the outbreak of infectious diseases requires a multifaceted and collaborative approach. By prioritizing vaccination campaigns, implementing public health measures, enhancing healthcare system preparedness, promoting education and awareness, fostering international collaboration, investing in research and development, and engaging communities, we can collectively work towards a world where the effects of seasonal influenza are minimized, protecting global public health.
Conclusion
The role of seasonal influenza in compounding the outbreak of infectious diseases cannot be overstated. As a highly contagious respiratory virus, influenza not only poses a significant health risk on its own but also amplifies the severity and spread of other infectious diseases, creating a compounding effect on public health systems. The seasonal nature of influenza leads to predictable surges in cases during colder months, placing additional strain on healthcare infrastructure already grappling with other infectious outbreaks.Effective management of seasonal influenza requires a multifaceted approach encompassing vaccination campaigns, public awareness initiatives, and robust surveillance systems to track and respond to outbreaks swiftly.By addressing the role of seasonal influenza in compounding infectious disease outbreaks, policymakers, healthcare professionals, and communities can better prepare and respond to future health crises, ultimately safeguarding population health and well-being.
Acknowledgement
The researchers appreciate Zarqa University for supporting this research publication
Conflicts of Interest
The authors declare no conflict of interest
Author’s contribution
SAH: conceived the idea and wrote the first draft; AA and FE: Source the literature relevant to the review article; AOJ: critically reviewed the manuscript. All authors read and approved the submission of the manuscript.
Funding source
No funding
References
- Baker RE, Mahmud AS, Miller IF, et al. Infectious disease in an era of global change. Nature Reviews Microbiology. 2022;20(4):193-205.
- Lawson A, López-Candales A. COVID-19 and seasonal influenza. Postgraduate Medicine. 2022:148-151.
- Piret J, Boivin G. Viral Interference between Respiratory Viruses. Emerging Infectious Diseases. 2022;28(2):273-281.
- Hagiwara Y, Harada K, Nealon J, Okumura Y, Kimura T, Chaves S. Seasonal influenza, its complications and related healthcare resource utilization among people 60 years and older: A descriptive retrospective study in Japan. Plos one. 2022;17(10):e0272795-e0272795.
- Javanian M, Barary M, Ghebrehewet S, Koppolu V, Vasigala VKR, Ebrahimpour S. A brief review of influenza virus infection. Journal of Medical Virology. 2021;93(8):4638-4646.
- Jansen JM, Gerlach T, Elbahesh H, Rimmelzwaan GF, Saletti G. Influenza virus-specific CD4+ and CD8+ T cell-mediated immunity induced by infection and vaccination. Journal of Clinical Virology. 2019;119:44-52.
- Flerlage T, Boyd DF, Meliopoulos V, Thomas PG, Schultz-Cherry S. Influenza virus and SARS-CoV-2: pathogenesis and host responses in the respiratory tract. Nature Reviews Microbiology. 2021;19(7):425-441.
- Mifsud E, Kuba M, Barr I. Innate Immune Responses to Influenza Virus Infections in the Upper Respiratory Tract. Viruses. 2021;13(10):2090-2090.
- LeMessurier K, Tiwary M, Morin N, Samarasinghe A. Respiratory Barrier as a Safeguard and Regulator of Defense Against Influenza A Virus and Streptococcus pneumoniae. Frontiers in Immunology. 2020;11:3-3.
- Dhanasekaran V, Sullivan S, Edwards K, et al. Human seasonal influenza under COVID-19 and the potential consequences of influenza lineage elimination. Nature Communications. 2022;13(1):1721-1721.
- Chen T, Attewell N, Malik A, Ludden D, Jin MR, Chiang M. The Problems and Possibilities of Global Asias Pedagogy. Verge: Studies in Global Asias. 2023;9(1):1-42.
- Hudu SA, Harmal NS, Malina O, Sekawi Z. Influenza vaccination among Malaysian healthcare workers: a survey of coverage and attitudes. The Medical Journal of Malaysia. 2016;71(5):231-237.
- Baker R, Mahmud A, Miller I, et al. Infectious disease in an era of global change. Nature Reviews Microbiology. 2021;20(4):193-205.
- Simonsen L, Viboud C, Taylor RJ, Miller MA. The epidemiology of influenza and its control. (eds) Influenza Vaccines for the Future. Birkhäuser Advances in Infectious Diseases. Springer, Basel. https://doi.org/10.1007/978-3-0346-0279-2_2.
- Matias G, Taylor R, Haguinet F, Schuck-Paim C, Lustig R, Shinde V. Estimates of hospitalization attributable to influenza and RSV in the US during 1997–2009, by age and risk status. BMC Public Health. 2017;17(1):1-14.
- Weeks V. Understanding sessional general practitioners. Education for Primary Care. 2007;18(sup1):279-282.
- Umpleby H, Houghton R. Infection prevention and surgery in the pandemic era. Surgery . 2021;39(11):722-729.
- Baker RE, Mahmud AS, Miller IF, et al. Infectious disease in an era of global change. Nature Reviews Microbiology. 2022;20(4):193-205.
- Maity B, Banerjee S, Senapati A, Chattopadhyay J. Quantifying optimal resource allocation strategies for controlling epidemics. Journal of the Royal Society Interface. 2023;20(202):20230036-20230036.
- Sigala IF, Sirenko M, Comes T, Kovács G. Mitigating personal protective equipment (PPE) supply chain disruptions in pandemics-a system dynamics approach. International Journal of Operations and Production Management. 2022;42(13):128-154.
- Nash R, Nouvellet P, Cori A. Real-time estimation of the epidemic reproduction number: Scoping review of the applications and challenges. PLOS Digital Health. 2022;1(6):e0000052-e0000052.
- Mohammadi M, Nikzad A. Sustainable and reliable closed-loop supply chain network design during pandemic outbreaks and disruptions. Operations Management Research. 2023;16(2):969-991.
- Chung S, Marlow S, Tobias N, et al. Lessons from countries implementing find, test, trace, isolation and support policies in the rapid response of the COVID-19 pandemic: a systematic review. BMJ Open. 2021;11(7):e047832-e047832.
- Alshrari A.S., Hudu, S.A., Imran M., et al. Rabbani, S.I. Innovations and development of COVID-19 vaccines: A patent review. Journal of Infection and Public Health. 2022 15(1), 123-131. doi: 10.1016/j.jiph.2021.10.021.
- Zhao X, Li M, Haihambo N, et al. Changes in Temporal Properties of Notifiable Infectious Disease Epidemics in China During the COVID-19 Pandemic: Population-Based Surveillance Study. JMIR Public Health and Surveillance. 2022;8(6):e35343-e35343.
- Engelmann L. Coinfection, Comorbidity, and Syndemics: On the Edges of Epidemic Historiography. Isis. 2023;114(S1):S71-S84.doi/epdf/10.1086/726981
- Yoo W, Choi D-H. Predictors of expressing and receiving information on social networking sites during MERS-CoV outbreak in South Korea. Journal of Risk Research. 2020;23(7-8):912-927.
- Kim Y. Outbreak news production as a site of tension: Journalists’ news-making of global infectious disease. Journalism. 2022;23(1):171-188.
- Augustynowicz A, Opolski J, Waszkiewicz M. Resilient Health and the Healthcare System. A Few Introductory Remarks in Times of the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2022;19(6):1-8.
- Grimm P, Oliver S, Merten S, Han W, Wyss K. Enhancing the understanding of resilience in health systems of low-and middle-income countries: a qualitative evidence synthesis. International Journal of Health Policy and Management. 2022;11(7):899-911.
- Mehedi N. Experiences of the Frontline Healthcare Professionals Amid the COVID-19 Health Hazard: A Phenomenological Investigation. Inquiry: a Journal of Medical Care Organization, Provision and Financing. 2022;59:469580221111925-469580221111925.
- Pala A, Chuang J, Chien A, et al. Depression, anxiety, and burnout among hospital workers during the COVID-19 pandemic: A cross-sectional study. Plos one. 2022;17(12):e0276861-e0276861.
- Sprung CL, Devereaux AV, Ghazipura M, et al. Critical Care Staffing in Pandemics and Disasters: A Consensus Report From a Subcommittee of the Task Force for Mass Critical Care–Systems Strategies to Sustain the Health Care Workforce. Chest. 2023;164(1):124-136.
- Proserpio P, Zambrelli E, Lanza A, et al. Sleep disorders and mental health in hospital workers during the COVID-19 pandemic: a cross-sectional multicenter study in Northern Italy. Neurological Sciences. 2022:43(4):2241-2251.
- Mehta A, Awuah W, Ng J, et al. Elective surgeries during and after the COVID-19 pandemic: Case burden and physician shortage concerns. Annals of Medicine and Surgery. 2022;81:104395-104395.
- Frio G, Russo L, de Albuquerque C, et al. The disruption of elective procedures due to COVID-19 in Brazil in 2020. Scientific Reports. 2022;12(1):10942-10942.
- Palmer CS. Innate metabolic responses against viral infections. Nature Metabolism. 2022;4(10):1245-1259.
- Suardi C, Cazzaniga E, Graci S, Dongo D, Palestini P. Link between Viral Infections, Immune System, Inflammation and Diet. International Journal of Environmental Research and Public Health. 2021;18(5):2455-2455.
- Han AX, de Jong SP, Russell CA. Co-evolution of immunity and seasonal influenza viruses. Nature Reviews Microbiology. 2023:1-13.
- Mirzaei R, Goodarzi P, Asadi M, et al. Bacterial co‐infections with SARS‐CoV‐2. IUBMB life. 2020;72(10):2097-2111.
- Dunning J, Thwaites RS, Openshaw PJ. Seasonal and pandemic influenza: 100 years of progress, still much to learn. Mucosal immunology. 2020;13(4):566-573.
- Metzger DW, Sun K. Immune dysfunction and bacterial coinfections following influenza. The Journal of Immunology. 2013;191(5):2047-2052.
- Morris D, Cleary D, Clarke S. Secondary Bacterial Infections Associated with Influenza Pandemics. Frontiers in Microbiology. 2017;8:1041-1041.
- Page L, Staples K, Spalluto C, Watson A, Wilkinson T. Influence of Hypoxia on the Epithelial-Pathogen Interactions in the Lung: Implications for Respiratory Disease. Frontiers in Immunology. 2021;12:653969-653969.
- Stölting H, Baillon L, Frise R, et al. Distinct airway epithelial immune responses after infection with SARS-CoV-2 compared to H1N1. Mucosal immunology. 2022;15(5):952-963.
- Morrison C, Edwards C, Shaffer K, et al. SARS-CoV-2 infection of airway cells causes intense viral and cell shedding, two spreading mechanisms affected by IL-13. Proceedings of the National Academy of Sciences of the United States of America. 2022;119(16):e2119680119-e2119680119.
- Cilloniz C, Luna C, Hurtado J, Marcos M, Torres A. Respiratory viruses: their importance and lessons learned from COVID-19. European Respiratory Review. 2022;31(166):220051-220051.
- Verma G, Dhawan M, Saied A, Kaur G, Kumar R, Emran T. Immunomodulatory approaches in managing lung inflammation in COVID-19: A double-edge sword. Immunity, Inflammation and Disease. 2023;11(9):e1020-e1020.
- Devi P, Yadav A, Yadav S, et al. Role of co-infections in modulating disease severities and clinical phenotypes. Genomic Surveillance and Pandemic Preparedness. 2023:151-186.
- Devi P, Khan A, Chattopadhyay P, et al. Co-infections as Modulators of Disease Outcome: Minor Players or Major Players? Frontiers in Microbiology. 2021;12:664386-664386.
- Reaser JK, Hunt BE, Ruiz-Aravena M, et al. Fostering landscape immunity to protect human health: A science-based rationale for shifting conservation policy paradigms. Conservation Letters. 2022;15(3):e12869.
- Grifoni A, Alonzi T, Alter G, et al. Impact of aging on immunity in the context of COVID-19, HIV, and tuberculosis. Frontiers in Immunology. 2023;14:1146704-1146704.
- Sieber P, Flury D, Güsewell S, et al. Characteristics of patients with Coronavirus Disease 2019 (COVID-19) and seasonal influenza at time of hospital admission: a single center comparative study. BMC Infectious Diseases. 2021;21(1):1-9.
- Jiang C, Yao X, Zhao Y, et al. Comparative review of respiratory diseases caused by coronaviruses and influenza A viruses during epidemic season. Microbes and infection. 2020;22(6-7):236-244.
- El-Radhi AS. Fever in common infectious diseases. Clinical Manual of Fever in Children. 2018:85-140.
- Jaworski CA, Donohue B, Kluetz J. Infectious disease. Clinics in sports medicine. 2011;30(3):575-590.
- Huff HV, Singh A. Asymptomatic transmission during the coronavirus disease 2019 pandemic and implications for public health strategies. Clinical Infectious Diseases. 2020;71(10):2752-6.
- El-Sadr WM, Platt J, Bernitz M, Reyes M. Contact tracing: barriers and facilitators. American Journal of Public Health. 2022;112(7):1025-33.
- Prashanth LK, Taly AB, Sinha S, Arunodaya GR, Swamy HS. Wilson’s disease: diagnostic errors and clinical implications. Journal of Neurology, Neurosurgery, and Psychiatry. 2004;75(6):907-9.
- Klinkenberg D, Fraser C, Heesterbeek H. The effectiveness of contact tracing in emerging epidemics. PloS one. 2006;1(1):e12.
- Watson SK, Rudge JW, Coker R. Health systems’“surge capacity”: state of the art and priorities for future research. The Milbank Quarterly. 2013;91(1):78-122.
- Kappler S, Wiesner L, Davis S. Pandemic Preparedness and Response. Ciottone’s Disaster Medicine 2024 Jan 1 (pp. 36-42). Elsevier.
- Hudu SA, Alshrari AS. Preparedness in Containment of Coronavirus Disease-19 in the African Continent. Bioscience Biotechnology Research Communications. 2020;13(3):1623-9.
- Baldassarre A, Giorgi G, Alessio F, Lulli LG, Arcangeli G, Mucci N. Stigma and discrimination (SAD) at the time of the SARS-CoV-2 pandemic. International journal of environmental research and public health. 2020;17(17):6341.
- Adinkrah EK, Cobb S, Bazargan M. Delayed Medical Care of Underserved Middle-Aged and Older African Americans with Chronic Disease during COVID-19 Pandemic. Healthcare. 2023;11(4):595-595.
- Pozo-Martin F, Beltran Sanchez MA, Müller SA, Diaconu V, Weil K, El Bcheraoui C. Comparative effectiveness of contact tracing interventions in the context of the COVID-19 pandemic: a systematic review. European Journal of Epidemiology. 2023;38(3):243-66.
- Connolly C, Keil R, Ali SH. Extended urbanisation and the spatialities of infectious disease: Demographic change, infrastructure and governance. Urban studies. 2021;58(2):245-263.
- Bakker H, Bindewald V, Dunke F, Nickel S. Logistics for diagnostic testing: An adaptive decision-support framework. European Journal of Operational Research. 2023;311(3) 1120-1133 https://doi.org/10.1016/j.ejor.2023.05.028.
- Gavina K, Franco L, Khan H, Lavik J, Relich R. Molecular point-of-care devices for the diagnosis of infectious diseases in resource-limited settings-A review of the current landscape, technical challenges, and clinical impact. Journal of Clinical Virology. 2023;169:105613-105613.
- Kucirka LM, Lauer SA, Laeyendecker O, Boon D, Lessler J. Variation in false-negative rate of reverse transcriptase polymerase chain reaction–based SARS-CoV-2 tests by time since exposure. Annals of internal medicine. 2020;173(4):262-267.
- Haldane V, De Foo C, Abdalla SM, et al. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nature Medicine. 2021;27(6):964-980.
- Abbey E, Khalifa B, Oduwole M, et al. The Global Health Security Index is not predictive of coronavirus pandemic responses among Organization for Economic Cooperation and Development countries. Plos one. 2020;15(10):e0239398-e0239398.
- Li W, Yang Y, Ng CH, et al. Global imperative to combat stigma associated with the coronavirus disease 2019 pandemic. Psychological medicine. 2021;51(11):1957-1958.
- Sattler S, Maskileyson D, Racine E, Davidov E, Escande A. Stigmatization in the context of the COVID-19 pandemic: a survey experiment using attribution theory and the familiarity hypothesis. BMC Public Health. 2023;23(1):521-521.
- Stenseth N, Schlatte R, Liu X, et al. How to avoid a local epidemic becoming a global pandemic. Proceedings of the National Academy of Sciences of the United States of America. 2023;120(10):e2220080120-e2220080120.
- Coppola DP, Milliken B. Incident Command (IC) Role in Coordination (Logistics and Politics). International Perspective. The Path of Flames: CRC Press; 2024:69-86.
- Agyarko R, Al Slail F, Garrett DO, et al. The imperative for global cooperation to prevent and control pandemics. Modernizing Global Health Security to Prevent, Detect, and Respond: Elsevier; 2024:53-69.
- Bloom D, Cadarette D. Infectious Disease Threats in the Twenty-First Century: Strengthening the Global Response. Frontiers in Immunology. 2019;10:549-549.
- Zhang Z, Shi L, Liu N, et al. Coverage and impact of influenza vaccination among children in Minhang District, China, 2013-2020. Frontiers in Public Health. 2023;11:1193839-1193839.
- Lazarus JV, Mark HE, Villota-Rivas M, et al. The global NAFLD policy review and preparedness index: are countries ready to address this silent public health challenge? Journal of Hepatology. 2022;76(4):771-780.
- Aruru M, Truong H-A, Clark S. Pharmacy Emergency Preparedness and Response (PEPR): a proposed framework for expanding pharmacy professionals’ roles and contributions to emergency preparedness and response during the COVID-19 pandemic and beyond. Research in Social and Administrative Pharmacy. 2021;17(1):1967-1977.
- Maddah N, Verma A, Almashmoum M, Ainsworth J. Effectiveness of Public Health Digital Surveillance Systems for Infectious Disease Prevention and Control at Mass Gatherings: Systematic Review. Journal of Medical Internet Research. 2023;25:e44649-e44649.
- Jia P, Liu S, Yang S. Innovations in Public Health Surveillance for Emerging Infections. Annual Review of Public Health. 2023;44:55-74.
- Berg SH, O’Hara JK, Shortt MT, et al. Health authorities’ health risk communication with the public during pandemics: a rapid scoping review. BMC Public Health. 2021;21(1):1-23.
- Stevens DL, Bryant AE. Endemic, epidemic and pandemic infections: the roles of natural and acquired herd immunity. Current Opinion in Infectious Diseases. 2023;36(3):171-176.
- Meyer D, Bishai D, Ravi S, et al. A checklist to improve health system resilience to infectious disease outbreaks and natural hazards. BMJ Global Health. 2020;5(8):e002429-e002429.
- Girum T, Lentiro K, Geremew M, Migora B, Shewamare S. Global strategies and effectiveness for COVID-19 prevention through contact tracing, screening, quarantine, and isolation: a systematic review. Tropical medicine and health. 2020;48:1-15.
- Venter M, Richter K. Towards effective diagnostic assays for COVID-19: a review. Journal of Clinical Pathology. 2020;73(7):370-377.
- Oza S, Chen F, Selser V, et al. Community-Based Outbreak Investigation And Response: Enhancing Preparedness, Public Health Capacity, And Equity: Commentary examines Community-Based Outbreak Investigation And Response, a local public health strategy developed during the COVID-19 pandemic. Health Affairs. 2023;42(3):349-356.
- Ehrlich H, Boneva D, Elkbuli A. The intersection of viral illnesses: A seasonal influenza epidemic amidst the COVID-19 pandemic. Vol 60: Elsevier; 2020:41-43.
- Jones N. How COVID-19 is changing the cold and flu season. Nature. 2020;588(7838):388-390.
- Batta I, Kaur T, Agrawal D. Distinguishing Swine Flu (H1N1) from COVID-19: Clinical, Virological, and Immunological Perspectives. Archives of Microbiology & Immunology. 2023;7(4):271-280.
- Harris G, Rak K, Kahn J, et al. US Hospital Capacity Managers’ Experiences and Concerns Regarding Preparedness for Seasonal Influenza and Influenza-like Illness. JAMA Network Open. 2021;4(3):e212382-e212382.
- Dombrádi V, Joó T, Palla G, Pollner P, Belicza É. Comparison of hesitancy between COVID-19 and seasonal influenza vaccinations within the general Hungarian population: a cross-sectional study. BMC Public Health. 2021;21(1):2317-2317.
- Lan C, Chen Y, Chang Y, Chuang P. Impact of COVID-19 Outbreak on Influenza and Pneumococcal Vaccination Uptake: A Multi-Center Retrospective Study. Vaccines. 2023;11(5):986-986.







