Manuscript accepted on :23-01-2024
Published online on: 04-03-2024
Plagiarism Check: Yes
Reviewed by: Dr. Elisha Paikray
Second Review by: Dr. Manoj Dalai
Final Approval by: Dr. Ayush Dogra
Tri Umiana Soleha1* , Sutyarso2
, Sutyarso2 , Asep Sukohar3
, Asep Sukohar3 , Sumardi2
, Sumardi2 and Sutopo Hadi4
and Sutopo Hadi4
1Doctoral Program, Faculty of Mathematics and Natural Sciences, University of Lampung, Bandar Lampung 35145, Indonesia.
2Department of Biology, Faculty of Mathematics and Natural Sciences, University of Lampung, Bandar Lampung 35145, Indonesia.
3Department of Pharmacology, Faculty of Medicine, University of Lampung, Bandar Lampung 35145, Indonesia.
4Department of Chemistry, Faculty of Mathematics and Natural Sciences, University of Lampung, Bandar Lampung 35145, Indonesia.
Corresoponding Author E-mail:dr.triumiana.unila@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2868
Abstract
Staphylococcus aureus is a type of bacteria that causes an increasing number of infections in hospitals, particularly in diabetic ulcers. Over the last few decades, there has been an alarming increase in the prevalence of pathogen strains of Staphylococcus aureus resistant to antibiotics such as Vancomycin. This study aimed to identify the presence of the vanA gene, which is responsible for the mode of Vancomycin resistance in Staphylococcus aureus Lampung isolate. Ulcer swab was collected from 32 patients with ulcer complications from surgical Installation, Internal Medicine, Home Diabetes Wound Clinic and Diabetes Wound Center in Bandar Lampung. Among the total ulcer swab, 12 samples of S. aureus were identified and subjected to the Minimum Inhibitory Concentration test to identify Vancomycin Resistant Staphylococcus aureus and evaluated the vanA gene by Polymerase Chain Reaction. To detect the presence of the vanA gene, a Polymerase Chain Reaction was performed on Staphylococcus aureus, Vancomycin-Resistant Staphylococcus aureus, and Vancomycin-intermediate Staphylococcus aureus using a specific primer arrangement. There were two samples of Vancomycin- Resistant Staphylococcus aureus and one sample of Vancomycin-intermediate Staphylococcus aureus from the Minimum Inhibitory Concentration test but only one sample tested positive for the vanA gene on Polymerase Chain Reaction. There is Staphylococcus aureus resistance to Vancomycin in Lampung isolate and the vanA gene was detected in some resistant isolates. The arrangement of the vanA gene in the Lampung isolate is different from that of the vanA gene in other places isolates.
Keywords
Resistant; S. aureus; vanA gen; Vancomycin
Download this article as:| Copy the following to cite this article: Soleha T. U, Sutyarso S, Sukohar A, Sumardi S, Hadi S. Identification of vanA gene on Vancomycin-Resistant Staphylococcus aureus from Diabetic Ulcer Isolate at Lampung Province. Biomed Pharmacol J 2024;17(1). |
| Copy the following to cite this URL: Soleha T. U, Sutyarso S, Sukohar A, Sumardi S, Hadi S. Identification of vanA gene on Vancomycin-Resistant Staphylococcus aureus from Diabetic Ulcer Isolate at Lampung Province. Biomed Pharmacol J 2024;17(1). Available from: https://bit.ly/3STC01S |
Introduction
The most common bacteria isolated from diabetic foot infections are Gram-positive cocci and members of the Gram-negative Enterobacteriaceae. Gram-positive bacteria such as Staphylococcus aureus, Enterococcus, and Gram-negative bacteria such as Pseudomonas aeruginosa, Escherichia coli, Klebsiella sp, and Proteus sp, can cause ulcer infection. S aureus is a major human pathogen that was first identified as the causative agent of suppurative abscesses more than 130 years ago1,2 Using antibiotics such as Penicillin and Methicillin in the mid-20th century was initially shown to be effective against Staphylococcus aureus. However, S. aureus quickly developed resistance to these antibiotics. Methicillin-resistant Staphylococcus aureus (MRSA) is becoming increasingly difficult to treat and makes this type of bacteria a major threat all over the world. Meanwhile, in the United States, Vancomycin is the drug of choice for handling MRSA2,3
Vancomycin is currently the antibiotic of choice for treating MRSA infections. The rate of MRSA infection continues to rise globally, and as a result, so does the consumption of Vancomycin. In Japan, the first case of Vancomycin intermediate Staphylococcus aureus (VISA) was reported in 1997. Since then, cases of Vancomycin resistant Staphylococcus aureus (VRSA) began to emerge, particularly in developing countries4. In Indonesia, research on the vanA gene (please add some explanation to relate the vanA gene VRSA) is still very rare, especially in Lampung province.
The purpose of this study was to analyze the suitability of Minimum Inhibitory Concentration (MIC) values to detect the presence of the novel vanA gene and find a new primer arrangement for the vanA gene from diabetic ulcer isolates in Lampung province. The vanA operon, which encodes the Tn1545 transposon and is part of the conjugative plasmid of Vancomycin-resistant enterococci, was used to generate the complete VRSA strain (MIC 16 mg/ml) (VRE). Vancomycin resistance is mediated by the glycopeptide-specific vanA gene. The presence of vanA causes an exchange within the terminal goal of D-alanyl-D-alanine to D-alanyl-D-lactate or D-alanyl-D-serine, resulting in a negative binding to Vancomycin due to the loss of the important factor for hydrogen bonding.5,6
Materials and Methods
Antibiotic Susceptibility Test
In this study, 32 samples were collected from patients with diabetic foot ulcers in Lampung province. The bacterial samples were placed on liquid nutrient agar media. After 24 hours of incubation, one colony was streaked into Mannitol Salt Agar (MSA) medium and incubated at 37°C for 48 hours to obtain the S. aureus strain7. Then the strain was suspended in 3 ml of physiological NaCl solution and its turbidity was compared to the McFarland standard of 0.5. In a petri dish, 100 µl of pure culture suspension was spread on the surface of Mueller Hinton Agar (MHA). The test medium was left at room temperature for five minutes to allow the bacteria to adapt to the medium. Subsequently, antibiotic disks containing Amoxycillin, Cefotaxime, Cefoxitin, and Vancomycin were placed on the medium. The mixture was then incubated at 37°C for 24 hours. A caliper was used to measure the diameter of the inhibition zone across the colony. Data from the clear zone were compared to those available in Clinical and Laboratory Standard Institute (CLSI) literature8
Minimum Inhibitory Concentration (MIC)
MIC for the strains collected from diabetic ulcers was determined by agar dilution as recommended by the National Committee for Clinical Laboratory Standards. Standard quality control strains were included in each run. Cultures were incubated for 20 to 24 h in ambient air. Drugs were obtained from their respective manufacturers. MIC was determined using the tube dilution method with Mueller Hinton Broth (MHB) at concentrations ranging from 4, 8, 16, 32, and 64 mg/mL. To test for the presence of VRSA, 1 mL of 0.5 MacFarland bacterial colony suspension was added to 1 mL of MHB and Vancomycin at various concentrations. The tube with the highest concentration, where bacterial growth was still visible, was scraped again on Nutrient Agar media and incubated for 24 hours to see if the bacteria, Vancomycin-resistant S. aureus, grew. The MIC concentration for whole vancomycin resistance in S. aureus was 16 mg/ml8,9
Primer Design
The primers were created using the National Center for Biotechnology Information’s BLAST software (NCBI). The primer sequence was created based on the DNA sequence that has been isolated or amplified. Primer comes in two varieties: forward primer and reverse primer. The primer acts as a limiter for the region to be read in the PCR reaction. A good primer design is critical to the success of the PCR reaction.10,11
Polymerase Chain Reaction for vanA Gene
PCR was used to amplify 1-3 µL of DNA in 100 µL of reaction mixture solution consisting of PCR buffer (10 m MTris-HCl pH 9.0), 50 mMol KCl, 1.5 mM MgCl2, 0.1 percent Triton X-100, 0.2 mg/ml bovine serum albumin, 50 M deoxynucleoside triphosphate, 2 primer pairs each, and 2 Taq polymerase enzyme (Qbiogene). The amplification was completed in 3 minutes at 94°C, and 30 amplification cycles consisting of 1 minute at 94°C, 1 minute at 54°C, 1 minute at 72°C, and 7 minutes at 72°C as the final step. This DNA fragment was examined using 0.5xTBE (Tris-Borate-EDTA) electrophoresis on a 1% agarose gel stained with ethidium bromide.12,13
This study has received approval from the Studies Ethics Committee College of Medication Lampung University with ethical clearance number 1616/UN26.18/PP.05.02.00/2021.
Results
S. aureus Antibiotic Susceptibility Test
Amoxicillin (Amx. ), Cefotaxime (Ctx. ), Cefoxitin (Fox. ), and Vancomycin were used in bacterial susceptibility testing of isolates from patients of diabetic ulcers (Va. ). Bacteria grown on Muller Hinton agar media were incubated for 24 hours at 37°C, after which the inhibition zone formed around the antibiotic was measured and classified as Resistance (R), Intermediate (I), or Sensitive (S) based on CLSI criteria, 2014. The results of antibiotic sensitivity tests are shown in Table 1.
Table 1: Susceptibility Profile of S. aureus Lampung Isolate with Antibiotics Penicillin, Cephalosporin and Glycopeptide.
| Sample Code | Antibiotic | |||
| AMX | CTX | Fox | VA | |
| S1 | R | R | R | R |
| S2 | R | R | R | R |
| S3 | R | R | R | R |
| S4 | R | I | S | R |
| S5 | R | R | S | R |
| S6 | R | I | R | S |
| S7 | R | R | R | S |
| S10 | R | R | R | S |
| S14 | R | I | S | S |
| S17 | R | R | S | S |
| S18 | R | S | S | R |
| S19 | R | I | R | I |
Note : AMX (R<21;122-27;S 28), CTX (R 14;115-22;S 23), FOX (R 21;121-22; S 22), VA (R 9;110-11;S 12)
AMX = Amoxicillin, CTX = Cefotaxim, FOX = Cefoxitin, VA = Vancomycin
Based on the data in Table 1, 100% of S. aureus samples were resistant to the antibiotic Amoxicillin; 50% of samples were resistant to Cefotaxime antibiotics, 33% were Cefotaxime intermediates, and 8.3% were sensitive to Cefotaxime. 50% of samples were resistant to the antibiotic Cefoxitin, while 41,6% were not. 50% of samples were resistant to the antibiotic Vancomycin, 8.3% were intermediate, and 41.7% were sensitive. It was discovered that 6 out of 12 test samples that met the inclusion criteria were resistant to Vancomycin or exhibited Vancomycin-resistant S. aureus (VRSA), while 7 out of 12 patients exhibited MRSA or Methicillin-resistant S. aureus (MRSA) or were multidrug resistant. As a result, there is little difference in the prevalence of MRSA and VRSA.
MIC of Vancomicyn-resistant Staphylococcus aureus (VRSA)
Six S. aureus isolates (Table 2) that were resistant to the antibiotic Vancomycin were tested for the presence of VRSA, and it was discovered that two samples have MIC = 32 g/mL that were VRSA, one sample has MIC = 8 g/mL that was Vancomycin Intermediate Staphylococcus aureus (VISA), and the other three samples were still susceptible to Vancomycin antibiotics.
Table 2: Minimum Inhibitory Concentration (MIC) of Vancomycin Resistant Staphylococcus aureus (VRSA) Lampung Isolate.
|
Sampel |
4 mg/mL |
8 mg/mL |
16 mg/mL |
32 mg/mL |
64 mg/mL |
Kind (MIC) |
Disk Diffusion (VA) |
|
|
S1 |
– |
– |
– |
– |
– |
VSSA |
VRSA |
|
|
S2 |
+ |
+ |
+ |
+ |
– |
VRSA |
VRSA |
|
|
S3 |
+ |
+ |
– |
– |
– |
VISA |
VRSA |
|
|
S4 |
+ |
+ |
+ |
+ |
– |
VRSA |
VRSA |
|
|
S5 |
– |
– |
– |
– |
– |
VSSA |
VRSA |
|
|
S18 |
– |
– |
– |
– |
– |
VSSA |
VRSA |
|
Note : (+) still growing (cut off point 16mg/mL)
(-) not growing 32 mg/mL
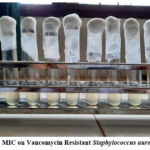 |
Figure 1: MIC on Vancomycin Resistant Staphylococcus aureus (VRSA) |
Primer Design for vanA Gene of Vancomycin Resistant Staphylococcus aureus (VRSA)
The complete VRSA strain (MIC≥16 µg/ml) was obtained from the vanA operon encoding transposon Tn1545 which is part of the conjugative plasmid of Vancomycin resistant enterococci (VRE). The primers were created with the help of the National Center for Biotechnology Information’s BLAST software (NCBI). The following candidates received the most votes:
(5′ 3′)
vanA_Foward : AGGAGACAGGAGCATGAATAG
vanA_Reverse : CAATACCGCACAACCGAC
In addition, a preliminary analysis was performed through the website https://sg.idtdna.com/calc/analyzer to obtain primary data in accordance with predetermined criteria. The results of primer analysis obtained are percentage of nucleotides in primer candidates (%GC Forward = 47.62%, %GC Reverse = 55.56%).
In another study in Tehran, a vanA gene primer pair was found with the arrangement shown in Figure 2.4
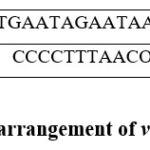 |
Figure 2: Primer arrangement of vanA gene (5’ to 3’). |
The primer pair is slightly different from the primers designed in this study, in terms of the percentage of guanine-cytosine and the size of the PCR product. Primer sequences were created from the isolated or amplified DNA sequence. Primer is classified into two types: forward primer and reverse primer. A primer serves as a separator for the region of the sequence to be read in a sequencing reaction. A good primer design is critical to the success of the PCR reaction. 6,14 Specific primers were developed in this study to detect Staphylococcus aureus strains from diabetic ulcer isolates in Indonesia.
Polymerase Chain Reaction
Using independently designed primers, PCR can detect Vancomycin-resistant Staphylococcus aureus (VRSA) and compare it to Vancomycin-sensitive Staphylococcus aureus (VSSA). VSSA is sample one, VRSA is sample number two and four, and VISA is sample number three. The results obtained are shown in the image in Figure 3.
Only sample No. 2 has the vanA gene because it is VRSA, whereas sample No. 1 does not have the vanA gene. After all, it is S. aureus, which is still susceptible to Vancomycin. Meanwhile, no vanA gene was detected by PCR examination in samples No. 3 (VISA) and No. 4 (VRSA) based on the MIC value. This is due to several factors, including the determination of VRSA based on the MIC value, which is the phenotype of resistant bacteria, whereas the genotype can be carried by genes other than vanA, such as vanS, vanR, and vanH. Another possibility is that the primer length used in sample No. 3 does not match the vanA gene.15,16
To clarify, the PCR process was repeated on sample No. 2, and the results of DNA amplification were obtained with an amplicon length of 673 bp, as shown in Figure 3.
 |
Figure 3: Sample 1. VSSA 2. VRSA 3. VISA 4. VRSA |
Discussion
The S. aureus is the causative agent of the high incidence of infection and is responsible for 80% of suppurative diseases with a natural habitat on the surface of the skin so that its presence can be suppressed with antibiotics so that increased morbidity rates lead to reduced mortality and human survival can be maintained longer. Diabetic ulcer is a chronic ulceration that occurs on the feet of patients with diabetes mellitus. Diabetic ulcers are mostly caused by S. aureus and Pseudomonas spp.17,18
Treatment of S. aureus bacterial infection in diabetic ulcers is difficult due to the ability of the bacteria to develop resistance to various antibiotics. For several decades, there has been an increase in the prevalence of pathogens and resistant strains to antibiotics. Methicillin was created in response to increased penicillin resistance. With the isolation of the first strain of Methicillin-resistant Staphylococcus aureus (MRSA) in 1961, infection by S. aureus can be well controlled using methicillin.19,20
Vancomycin is the last antibiotic resistance test in this study. The cultured isolates from diabetic ulcer patients in Lampung province revealed that six of the twelve isolates identified by the S. aureus bacteria are resistant to Vancomycin antibiotics, one is in the intermediate group and the remaining five samples are still in the sensitive group. Based on these findings, we can see that the sensitivity of vancomycin antibiotics has decreased, even though it is still a positive control of each antibiotic sensitivity test and the most effective control for the presence of MRSA.21,22
The number of VRSA obtained from the results of the Vancomycin antibiotic susceptibility test using the disc diffusion method differs from the number of VRSA obtained from the results of the Vancomycin antibiotic susceptibility test using the dilution method, where the number of VRSA in the disc diffusion method is 6 samples and the MIC method is 3 samples. This is because the Vancomycin antibiotic is more evenly dispersed into the bacterial suspension in the MIC test, and Vancomycin is more likely to inhibit the growth of S. aureus.9,23 Because the disc diffusion technique for antibiotic susceptibility testing is not a quantitative method, the data obtained from the antibiotic susceptibility test based on the MIC value as recommended by Clinical and Laboratory Standard Institute (CLSI).7
When the vanA gene primer from VRE was used, no PCR products were produced from the 4 samples. This is because the low percentage of Guanine Cytosine (GC) reduces the efficiency of the PCR process due to the weaker bonding of the primers so that they are easily released and the primers do not recognize the sample. Good Cytosine Guanine binding in the primer is 40% – 55%10. Next, a new primer using the BLAST primer design method from NCBI. 24,25was designed. Primers are usually designed to isolate specific fragments of genomic DNA by PCR. The primer sequence is made based on the DNA sequence to be isolated or amplified. Good primer design is essential for the success of a PCR reaction. In this research, only the vanA gene can be detected in one isolate, this happens because only 69% of VRSA can detect the the vanA gene. 26The primers produced in this study are specific for the vanA gene derived from diabetic ulcers in Lampung province. For VRSA detection, the discovery of the vanA gene cannot yet be used as a standard examination, so further research is needed.
The discovery of the vanA gene in diabetic ulcer isolates indicates that the process of Staphylococcus aureus bacteria resistance to Vancomycin antibiotics in Indonesia, particularly in the province of Lampung, is confirmed and this should be monitored. Because the findings of the vanA gene and specific new primers are very important to detect the presence of VRSA in various regions so that it can prevent further bacterial resistance, similar studies need to be carried out with a larger number of samples.27,28 Not only do VRSA from different regions have different genetic features, but even from 1 patient, several VRSA strains can be obtained. 29,30It is necessary to consider more rational use of antibiotics in the cases of severe infections such as diabetic ulcers to avoid the occurrence of antibiotic resistance.
Conclusion
VRSA that was found in Lampung isolate has a MIC value of 32 mg/mL and based on the PCR electrophoresis images it turned out that a new band with a size of 673 bp was found in VRSA sample No.2 which indicated the presence of the vanA gene carrying resistance to the antibiotic Vanomycin Lampung isolate. This band appears in the PCR electrophoresis image using the new primer arrangement as follows vanA_Foward : AGGAGACAGGAGCATGAATAG
vanA_Reverse : CAATACCGCACAACCGAC. There is S. aureus resistance to Vancomycin in Lampung isolate and the vanA gene was detected in some resistant isolates. The emergence of VRSA must be taken care of because it is an indicator of widespread bacterial resistance.
Acknowledgement
None
Conflict of Interest
The authors declare no conflict of interest to other parties.
Funding Source
None
References
- Kerner W, Brückel J. Definition, classification and diagnosis of diabetes mellitus. Experimental and Clinical Endocrinology and Diabetes. 2014;122(7):384-386. doi:10.1055/s-0034-1366278
CrossRef - Banu A, Noorul Hassan MM, Rajkumar J, Srinivasa S. Spectrum of bacteria associated with diabetic foot ulcer and biofilm formation: A prospective study. Australasian Medical Journal. 2015;8(9):280-285. doi:10.4066/AMJ.2015.2422
CrossRef - Mcguinness WA, Malachowa N, Deleo FR. Vancomycin Resistance in Staphylococcus Aureus. Vol 90.; 2017.
- Dezfulian A, Aslani MM, Oskoui M, et al. Identification and Characterization of a High Vancomycin-Resistant Staphylococcus aureus Harboring VanA Gene Cluster Isolated from Diabetic Foot Ulcer. 2012;15(2):803-806.
- Jawetzs, Meilnick, Eidelberg. Jawetz Microbiology. 25th ed. (Brooks G CKBJMS, ed.).; 2014.
- Périchon B, Courvalin P. VanA-type vancomycin-resistant Staphylococcus aureus. Antimicrob Agents Chemother. 2009;53(11):4580-4587. doi:10.1128/AAC.00346-09
CrossRef - Kateete DP, Kimani CN, Katabazi FA, et al. Identification of Staphylococcus aureus: DNase and Mannitol salt agar improve the efficiency of the tube coagulase test. Ann Clin Microbiol Antimicrob. 2010;9. doi:10.1186/1476-0711-9-23
CrossRef - Cong Y, Yang S, Rao X. Vancomycin resistant Staphylococcus aureus infections: A review of case updating and clinical features. J Adv Res. 2020;21:169-176. doi:10.1016/j.jare.2019.10.005
CrossRef - Jiang L, Wang F, Han F, Prinyawiwatkul W, No HK, Ge B. Evaluation of diffusion and dilution methods to determine the antimicrobial activity of water-soluble chitosan derivatives. J Appl Microbiol. 2013;114(4):956-963. doi:10.1111/jam.12111
CrossRef - Borah P. Primer Designing for PCR.; 2011. www.sciencevision.in
CrossRef - Li D, Zhang J, Li J. Primer design for quantitative real-time PCR for the emerging Coronavirus SARS-CoV-2. Theranostics. 2020;10(16):7150-7162. doi:10.7150/thno.47649
CrossRef - Shariati A, Dadashi M, Moghadam MT, van Belkum A, Yaslianifard S, Darban-Sarokhalil D. Global prevalence and distribution of vancomycin resistant, vancomycin intermediate and heterogeneously vancomycin intermediate Staphylococcus aureus clinical isolates: a systematic review and meta-analysis. Sci Rep. 2020;10(1). doi:10.1038/s41598-020-69058-z
CrossRef - Bamigboye BT, Olowe OA, Taiwo SS. Phenotypic and molecular identification of vancomycin resistance in clinical Staphylococcus aureus isolates in Osogbo, Nigeria. Eur J Microbiol Immunol (Bp). 2018;8(1):25-30. doi:10.1556/1886.2018.00003
CrossRef - Fredriksson NJ, Hermansson M, Wilén BM. The Choice of PCR Primers Has Great Impact on Assessments of Bacterial Community Diversity and Dynamics in a Wastewater Treatment Plant. PLoS One. 2013;8(10). doi:10.1371/journal.pone.0076431
CrossRef - Elsayed N, Ashour M, Ezzat A, Amine K. Original article Vancomycin resistance among Staphylococcus aureus isolates in a rural setting , Egypt. 2018;8(September):134-139.
CrossRef - Samadin KH, Aziz S, Farmakologi B, Kedokteran F, Sriwijaya U. Pola Kepekaan Bakteri Staphylococcus aureus terhadap Antibiotik Vancomycin di RSUP Dr . Mohammad Hoesin Palembang. 2014;(4):266-270.
- Hasan R, Acharjee M, Noor R. Prevalence of vancomycin resistant Staphylococcus aureus ( VRSA ) in methicillin resistant S . aureus ( MRSA ) strains isolated from burn wound infections. Tzu Chi Med J. 2016;28(2):49-53. doi:10.1016/j.tcmj.2016.03.002
CrossRef - Banu A, Noorul Hassan MM, Rajkumar J, Srinivasa S. Spectrum of bacteria associated with diabetic foot ulcer and biofilm formation: A prospective study. Australasian Medical Journal. 2015;8(9):280-285. doi:10.4066/AMJ.2015.2422
CrossRef - Sotto A, Richard JL, Messad N, et al. Distinguishing colonization from infection with Staphylococcus aureus in diabetic foot ulcers with miniaturized oligonucleotide arrays: A French multicenter study. Diabetes Care. 2012;35(3):617-623. doi:10.2337/dc11-1352
CrossRef - Tefera S, Awoke T, Mekonnen D. Methicillin and vancomycin resistant staphylococcus aureus and associated factors from surgical ward inpatients at debre markos referral hospital, northwest Ethiopia. Infect Drug Resist. 2021;14:3053-3062. doi:10.2147/IDR.S324042
CrossRef - Walters MS EPAVTTLDHGTD. Vancomycin – Resistant Staphylococcus aureus – Delaware. MMWR Morb Mortal Wkly. 2015;64(37):1056-1066.
CrossRef - Unni S, Siddiqui TJ, Bidaisee S. Reduced Susceptibility and Resistance to Vancomycin of Staphylococcus aureus: A Review of Global Incidence Patterns and Related Genetic Mechanisms. Cureus. Published online October 20, 2021. doi:10.7759/cureus.18925
CrossRef - Katzung BG. Basic & Clinical Pharmacology. http://www.usdoj.gov/ dea/pubs/scheduling.html
- Yousefi M, Fallah F, Arshadi M, Pourmand MR, Hashemi A, Pourmand G. Identification of tigecycline- and vancomycin-resistant Staphylococcus aureus strains among patients with urinary tract infection in Iran. New Microbes New Infect. 2017;19:8-12. doi:10.1016/j.nmni.2017.05.009
CrossRef - Tiwari HK, Sen MR. Emergence of vancomycin resistant Staphylococcus aureus (VRSA) from a tertiary care hospital from northern part of India. BMC Infect Dis. 2006;6. doi:10.1186/1471-2334-6-156
CrossRef - Mcguinness WA, Malachowa N, Deleo FR. Vancomycin Resistance in Staphylococcus aureus. 2017;90:269-281.
CrossRef - Olufunmiso O, Tolulope I, Roger C. Multidrug and vancomycin resistance among clinical isolates of Staphylococcus aureus from different teaching hospitals in Nigeria. 2017;17(3).
CrossRef - Liu M, Yang Z hui, Li G hui. A Novel Method for the Determination of Vancomycin in Serum by High-Performance Liquid Chromatography-Tandem Mass Spectrometry and Its Application in Patients with Diabetic Foot Infections. 2018;(Figure 1):1-12. doi:10.3390/ molecules23112939
CrossRef - Selim S, Faried OA, Almuhayawi MS, et al. Incidence of Vancomycin-Resistant Staphylococcus aureus Strains among Patients with Urinary Tract Infections. Antibiotics. 2022;11(3). doi:10.3390/ antibiotics 11030408
CrossRef - Wu Q, Sabokroo N, Wang Y, Hashemian M, Karamollahi S, Kouhsari E. Systematic review and meta-analysis of the epidemiology of vancomycin-resistance Staphylococcus aureus isolates. Antimicrob Resist Infect Control. 2021;10(1). doi:10.1186/s13756-021-00967-y
CrossRef - Samsuar S., Simanjuntak W., Qudus H.I., Yandri Y., Herasari D., Hadi S. In Vitro Antimicrobial Activity Study of Some Organotin(IV) Chlorobenzoates against Staphylococcus aureus and Escherichia coli. Journal of Advanced Pharmacy and Education Research. 2021; 11 (2): 17-22.
CrossRef







