Manuscript accepted on :04-02-2023
Published online on: 24-08-2023
Plagiarism Check: Yes
Reviewed by: Dr. Thambidorai C R
Second Review by: Dr. Yahya Wahba
Final Approval by: Dr. Ian James Martin
Sonali Pradeep Suryawanshi* , Priti Pravin Dhande
, Priti Pravin Dhande , Pallawi Shashank Khatavkar
, Pallawi Shashank Khatavkar and Linpadmaja Prabhakar Thakur
and Linpadmaja Prabhakar Thakur
Bharati Vidyapeeth (DTU) Medical College, Pune, Maharashtra, India.
Corresponding Author E-mail:docssurya@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2742
Abstract
Background and Objectives: The most commonly prescribed drugs in healthcare systems are proton pump inhibitors (PPIs). Several studies have found that globally PPIs are frequently used without proper justification. Appropriate and updated knowledge about PPI among medical professionals is essential to enhance the rationale of PPI application. The present study with this goal was initiated to evaluate the understanding and behavioral practices toward PPI use among resident doctors in a tertiary care teaching hospital in Pune, western India. Method: A cross sectional survey using structured questionnaire. Results: The questionnaire was completed by 137 resident doctors. 82.5% of them prescribed acid-suppressing drugs for acute gastritis and other drugs in combination with them as the most common indications for the majority of their patients. These prescriptions were based on the consultant's or unit's policy, and resident doctors were not given the liberty to breach this policy. 71.5% of the respondents chose PPIs as their first choice, and 75.1% preferred the oral route. 10.2% of them claimed to have encountered a PPI-related adverse event. Despite the fact that 75.9% of the respondents preferred to prescribe PPIs for short durations, a lack of awareness about the possible risks associated with chronic PPI use was noted. 58.4% of resident doctors preferred using the step-down strategy, but 19.7% of participants were unaware of step up or step down when prescribing PPIs. The concept of drug interactions with the co-administration of PPI was also less understood by study participants. Conclusion: In the present survey study participants had less knowledge on correct indications for PPI usage as they fared PPI over any other acid-reducing medications to majority of their patients. There was also a lack of understanding of PPI adverse drug reactions, drug-drug interactions, and specific PPI administration approaches.
Keywords
GERD; Knowledge; Proton Pump Inhibitors; Practices; Resident doctors; Western India
Download this article as:| Copy the following to cite this article: Suryawanshi S. P, Dhande P. P, Khatavkar P. S, Thakur L. P. Knowledge, Attitude and Practices of Resident Doctors Towards Use of Proton Pump Inhibitors in a Tertiary Care Hospital in Pune, India: A Cross-Sectional Survey. Biomed Pharmacol J 2023;16(3). |
| Copy the following to cite this URL: Suryawanshi S. P, Dhande P. P, Khatavkar P. S, Thakur L. P. Knowledge, Attitude and Practices of Resident Doctors Towards Use of Proton Pump Inhibitors in a Tertiary Care Hospital in Pune, India: A Cross-Sectional Survey. Biomed Pharmacol J 2023;16(3). Available from: https://bit.ly/3R7LRlz |
Introduction
Proton pump inhibitors (PPIs) are one of the most commonly used types of drugs in the world, and there are many articles about how to use them correctly and how not to use inappropriately.1-4 There are reports indicating PPI prescriptions have climbed dramatically worldwide.1,5-8 Global studies have also revealed that the excessive use of PPIs in both intensive and non-intensive care settings places a significant financial burden on health-care systems.1,5,9 However, a systematic assessment of the attitudes and practices of health care providers towards the use of these drugs for improving the rational use of PPIs in developing countries, including India, is lacking.10-12 For a variety of GI diseases related to acid, proton pump inhibitors (PPIs) are among the most commonly prescribed medications in healthcare systems. There are published recommendations and guidelines for using PPIs in various clinical conditions.13-15
Despite the existence of guidelines, many studies have noted the uncontrolled use of these medications. Even in the absence of risk factors, PPIs are frequently administered to patients who are on nonsteroidal anti-inflammatory drugs (NSAIDs).3,9 This method can make it more likely that a drug will have side effects and be a waste of money. PPI medication for a short period is usually well tolerated. Continuous PPI usage, however, has been associated with a greater risk of infections, osteoporosis, and other significant side effects, including fractures, bone marrow toxicity, community-acquired pneumonia, Clostridium difficile diarrhea, etc.16
As there are few studies from developing nations on the extent of prescribing and appropriateness of PPI use, the attitudes and behaviors of healthcare professionals regarding the use of this class of drugs need to be rigorously evaluated.10-12
For the application of PPIs to be more logically justified, resident doctors’ knowledge of PPIs is crucial. In view of this, we conducted a questionnaire-based study to assess resident doctors’ knowledge, attitude, and prescribing practices of gastric acid suppressants, particularly PPIs, at a tertiary care hospital in western India.
Material and Methods
A cross-sectional, observational study among resident doctors from clinical branches in a tertiary care teaching hospital in Pune, Western India, was conducted. The study was approved by the Institutional Ethics Committee (BVDUMC/IEC/E4), and written informed consent was obtained from all the participating resident doctors. An extensive search of the literature on the internet turned up little information about the prevalence of awareness of the proper usage of PPIs among resident doctors, particularly in developing countries in a tertiary care hospital. The sample size calculations were thus based on the assumption that 50% of the residents had correct knowledge regarding the rational use of PPIs. with a 95% confidence limit and a 5% tolerance for error applied in the Rao software online formula17,18 to estimate a reasonable sample size, which amounted to 137 participants. Hence, of the total 212 resident doctors in our study setup, we surveyed 137 resident doctors of clinical departments who were involved in prescribing PPI [Medicine, Surgery, Gynecology, Orthopedics, Anesthesiology].
The study questionnaire was created after referring to similar kinds of research studies carried out in other clinical settings.10,19,20 The questionnaire’s first section included demographic data such as name, age, and gender, followed by the knowledge-assessing section, which included queries aimed at gathering data such as correct choice, recommended method of delivery, and required duration of gastric acid-reducing medications. In the following section, resident doctors’ viewpoints were included, along with how well they comprehended the course of treatment and were aware of the risks of PPI use. Inquiries regarding common indications and dangers, as well as potential risks associated with long-term PPI usage, had a choice of many responses to opt for.
Before the major survey, the questionnaire was given to relevant professionals in the fields of pharmacology and medicine for scrutiny. The designed questionnaire was pretested among ten resident doctors in a comparable setting (pilot study). The questionnaire was adjusted in light of expert recommendations and results from a pilot study. The necessary modifications had been incorporated in the final questionnaire and utilized among study participants.
Statistical Analysis: Data were entered into Microsoft Excel (MS Office 2008), and statistical analyses were conducted using SPSS version 28.0 (IBM SPSS, Chicago). The results are presented as frequencies and percentages.
Results
137 resident doctors from chosen clinical branches completed the questionnaire, and the majority of them were male resident doctors (64%), with an average age between 20 and 30 years.
The resident doctors’ drug prescriptions were based on the consultant’s or unit’s policy, which is common in tertiary care practices, and they were not given any flexibility in doing so.
100% of the respondent doctors confirmed that they had given their patients antiulcer medications.
82.5% reported prescribing acid-suppressing medications (PPI and H2 blockers) for the majority of their patients, 3.6% of whom almost always administered them. About 71% of respondents reported PPIs were often the first acid-suppressing medication they had chosen, and 75.1% of them preferred the oral route for their administration. The majority of the study participants (75.9%) prescribed PPI once daily for a duration of less than 1 week, which is the recommended duration. Also, the majority of the resident doctors (92%) knew that oral PPI intake should be in the morning before breakfast.
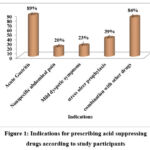 |
Figure 1: Indications for prescribing acid suppressing |
The commonest indication for which resident doctors prescribed acid suppressive drugs were acute gastritis (89%) in combination with other drugs (84%), followed by prophylaxis against stress ulcers. (39%) [Figure 1]
Only 14 resident doctors (10.2%) reported experiencing a PPI-related adverse event and specifically mentioning nausea, vomiting, and diarrhea as the adverse events. When asked about any possible adverse effects with PPI, a total of 94 responses were received from the 88 participants (64.2%) who opted to respond to this question. According to the responses on the awareness of the risks inherent with long-term usage of PPIs, just 16% of the participants were aware of a higher risk of community-acquired pneumonia, 48% knew about Clostridium difficile infection, and 30% knew about hip fractures or osteoporosis as a long-term risk with PPI. [Figure 2]
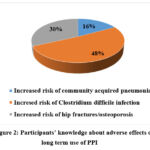 |
Figure 2: Participants’ knowledge about adverse effects on long term use of PPI |
Table 1: Participants’ knowledge about drug interactions with PPI
|
Drugs |
No. of responses |
Percentage |
|
Aspirin |
12 |
8.8 |
|
Warfarin |
33 |
24.1 |
|
Digoxin |
15 |
10.9 |
|
Iron |
48 |
35 |
|
Any other |
0 |
0 |
83 (60.6%) residents stated that drug interactions can happen with the co-administration of PPI with other medications. When persistently administered with PPIs, they found that medications like iron (35%) and warfarin (24%), besides a few others, can cause clinically significant interactions. Unfortunately, none of the participants was aware that all drugs mentioned in Table 1 could have possible drug–drug interactions when co-administered with PPIs.
In response to an open-ended inquiry about recommendations for therapeutic approaches while using acid suppressing agents, 19.7% of participants were unable to name any such approach. When prescribing PPI to their patients, 58.4% of resident doctors preferred using the step-down strategy, while 21.9% of participants preferred the step-up approach. Only 5.1% of the respondents who answered correctly stated that they should wait seven to eight weeks before switching from one strategy to another. Only 13.13% of the resident doctors in the study suggested that GERD patients should change their lifestyle.
 |
Figure 3: Study Participants’ Practice- approach while prescribing the PPI. |
Discussion
PPI is overused and often used without proper justification, according to several studies worldwide.3,5,9,21,22 Appropriate and updated knowledge about PPI among medical professionals is essential to enhance the rationale of PPI application. There are not many studies evaluating prescription drug usage and the appropriateness of using PPI in developing countries, including India.1,10 In view of this, the present study was initiated to evaluate the understanding and behavioral practices toward PPI use among the resident doctors in the study setting.
The extent of use of drugs for reducing gastric acid was high in the present study and among the majority of the study participants. PPIs were the acid-suppressing medication of choice for 71.5% of respondents. Our study findings are similar to those of earlier studies 1,10,22 conducted in India and other developed countries where the majority of patients were prescribed acid-suppressing medications and PPI was the top choice among these medications. Though the majority of resident doctors preferred oral PPIs, some of them opted for intravenous PPI for acid suppression in their hospitalized patients. The authors have mentioned that parenteral PPIs are frequently prescribed by doctors instead of oral PPIs to achieve higher therapeutic efficacy.10,12 Oral PPI appears to be as effective as parenteral PPI, and only a small percentage of patients with upper GI bleeding require parenteral PPI administration.23
Prescription of acid suppressive agents in acute gastritis is appropriate and has been found in other studies such as this one, but treatment in these cases should ideally begin with H2 blockers and be stepped up to PPI after 6-8 weeks if necessary. Step-up therapy (treat for eight weeks with H2 blockers; if symptoms do not improve, switch to PPI) or step-down therapy are the preferred empiric approaches (treat initially with PPI; then titrate to the lowest efficient drug type and dosage). 19.7% of the study respondents were unable to name any such approaches while prescribing PPI to their patients. Our research revealed that a significant percentage of doctors chose PPIs over H2 blockers, and as a result, it was impossible to avoid a rise in treatment costs. The selection of appropriate approaches for PPI prescriptions was not implemented in the current system with valid indications. Proven techniques, including step-down, step-up, and on-demand therapy with PPIs, should be applied in our tertiary teaching hospital in order to optimize the cost-effectiveness of PPI-based treatment.24 Because the prescription of drugs, including PPIs, by resident doctors is primarily determined by the consultant’s policy, educational interventions to all clinicians, including resident doctors, for appropriateness and encouragement for step-down approaches following regular review of ongoing indications for PPI use, as well as de-prescribing PPI policy without valid indication, could be beneficial.
A PPI is the first-line treatment for patients with erosive esophagitis noticed during an endoscopy. PPIs, as “prophylactic” gastro-protective medications, were mentioned by study participants as being prescribed to patients on NSAIDs, similar to other studies.3,9,10 But it is illogical to recommend PPI to every patient who takes NSAIDs.25 Patients suffering from chronic conditions who need NSAIDs should be given coxib, misoprostol, or a PPI if GI risk factors are present. However, without a thorough assessment of their GI risk factors, such patients are frequently offered gastro-protective medications on an empirical basis.10 From a scientific perspective, even consistently administering PPI to the majority of in-patients without evident reasons is inappropriate. National and international guidelines specifying the rational indications for prescribing PPI are available and should be referred to by clinicians during their practice.13-15
Even though the majority of our respondents opted to only administer PPIs for short durations (75.9%), we noted a lack of awareness about the possible risks associated with long-term PPI usage. According to their understanding of the risks inherent with prolonged use of PPIs, just 16% of the resident doctors were aware of a higher risk of community-acquired pneumonia. The hazards of Clostridium difficile infection and hip fractures or osteoporosis associated with chronic use of PPI were also less well understood.16 A study by Patel et al. on the usage of acid suppressants also concluded that excessive PPI prescriptions may be a risk factor for negative side effects, medication interactions, additional cost, and even incorrect prescriptions.26 According to a recent study, Wu B et al reported six AKI (acute kidney injury) and CKD (chronic kidney disease) signals related to PPI. The median duration for CKD was greater than for AKI; however, the authors here indicate that a significant percentage of patients experienced renal damage after one year of PPI medication. A meta-analysis by Yang et al. in 2017 also revealed that PPI use might be linked to untoward effects on the kidneys in patients with certain risk factors, like young age, high-dose PPI use, existing kidney damage, concurrent use of nephrotoxic agents, etc. Hence, PPI-associated kidney injury should be considered a major risk with chronic use of this class of drugs, and the significance of prudent PPI use should be highlighted in clinical settings.27,28
In the present study, 61% of residents stated that drug interactions can happen with the co-administration of PPI with other medications. But besides one or two drugs mentioned in Table 1, none of the participants was aware that all drugs mentioned could have possible drug–drug interactions when co-administered with PPIs. Inappropriate PPI prescriptions may cause adverse drug reactions. Only a small number of PPI-drug interactions are clinically important, since different PPIs have varying propensities to interact with other medications. According to a study conducted by Blume H et al., in contrast to lansoprazole, pantoprazole, and rabeprazole, which have lesser affinities for particular CYP isoenzymes, omeprazole and esomeprazole have a higher possibility for drug interactions (high affinity for CYP2C19 and moderate affinity for CYP3A4).29
Doctors’ lack of knowledge of these could exacerbate the problem of PPI usage. Therefore, rational prescribing is necessary when using PPIs in hospital practice.
There is no institute or unit policy in the current study set up for prescribing PPIs with documentation of indications in accordance with guidelines. Rational PPI use can benefit from simple, resident-driven quality improvement initiatives that use valid approaches for reviewing the patient’s indication. Also, specific measures like regular audits, feedback to prescribers, and educational interventions for rational prescribing of PPIs may be helpful in preventing PPI abuse.
Despite the helpful findings gathered from our study, a few limitations need to be mentioned. Firstly, our findings regarding knowledge, attitude, and behavior about PPI usage among resident doctors may be influenced by self-reporting bias and an overestimation of positive information. Secondly, the applicability of the findings from this data may be constrained because this survey only included resident doctors in a single tertiary teaching hospital.
Conclusion
PPI overuse is still a regular practice in Indian hospitals. There is a lack of understanding about the proper indications for PPI use, as our study participants recommended PPI over any other acid-reducing medication to the majority of their patients, primarily as a consultant’s policy. Low level of knowledge regarding adverse drug reactions, drug-drug interactions with PPIs, and specific approaches for PPI delivery regimens was also noticed.
Conflict of Interest
There is no conflict of interest
Funding Sources
There are no funding source
References
- Verma N, Tayal V, Roy V. Proton Pump Inhibitors: Prescribing Practices, Appropriateness of Use, and Cost Incurred in a Tertiary Care, Public, Teaching Hospital in New Delhi, India. MAMC J Med Sci 2019; 5:113-20.
CrossRef - Heidelbaugh JJ, Kim AH, Chang R et al. Overutilization of proton-pump inhibitors: what the clinician needs to know. Therapeutic advances in gastroenterology. 2012;5(4):219-32.
CrossRef - Akram F, Huang Y, Lim V Et al. Proton pump inhibitors: are we still prescribing them without valid indications? The Australasian Medical Journal. 2014;7(11):465.
CrossRef - Ahrens D, Behrens G, Himmel W et al. Appropriateness of proton pump inhibitor recommendations at hospital discharge and continuation in primary care. Int J Clin Pract 2012;66:767-73.
CrossRef - Ramirez E, H Lei S, M Borobia A et al. Overuse of PPIs in patients at admission, during hospitalisation, and at discharge in a terciary Spanish hospital. Current clinical pharmacology. 2010;5(4):288-97.
CrossRef - Zeng W, Finlayson AE, Shankar S et al. Prescribing efficiency of proton pump inhibitors in China: influence and future directions. BMC health services research. 2015;15(1):1-9.
CrossRef - Garuolienė K, Godman B, Gulbinovič J et al. Differences in utilization rates between commercial and administrative databases: implications for future health-economic and cross-national studies. Expert review of pharmacoeconomics & outcomes research. 2016;16(2):149-152.
CrossRef - Godman B, Kurdi A, Leporowski A et al. Initiatives to increase the prescribing of low cost generics: the case of Scotland in the international context. Medical Research Archives. 2017;5(3):1-34.
CrossRef - Haroon M, Yasin F, Gardezi SK et al. Inappropriate use of proton pump inhibitors among medical inpatients: a questionnaire-based observational study. JRSM short reports. 2013;4(8): 2042533313497183.
CrossRef - Padhy BM, Bhadauria HS, Gupta YK. Attitude and knowledge of Indian emergency care residents towards use of proton pump inhibitors. International scholarly research notices. 2014;2014.
CrossRef - Biswas S, Sufian AA, Sarkar PK et al. Over prescription of proton pump inhibitors on discharge of medical inpatients. Journal of Medicine. 2017;18(1):27-9.
CrossRef - Churi S, Jogani A. Prospective assessment of prescribing pattern of intravenous proton pump inhibitors in an Indian Tertiary-Care Teaching Hospital. Indian Journal of Pharmacy Practice. 2014;7(4):2-7.
CrossRef - Lanza FL, Chan FK, Quigley EM; Practice Parameters Committee of the American College of Gastroenterology. Guidelines for prevention of NSAID-related ulcer complications. Am J Gastroenterol. 2009;104(3):728-738.
CrossRef - Satoh K, Yoshino J, Akamatsu T et al. Evidence-based clinical practice guidelines for peptic ulcer disease 2015. J Gastroenterol 51, 177–194 (2016).
CrossRef - Thomas JS, Dennis MJ. Gastrointestinal bleeding. In Feldman M, Lawrence SF, Lawrence JB, eds. Sleisenger and Fordtran’s Gastrointestinal and Liver Disease. New York: Elsevier. 2010. pp302-3.
- Kinoshita Y, Ishimura N, Ishihara S. Advantages and disadvantages of long-term proton pump inhibitor use. Journal of neurogastroenterology and motility. 2018;24(2):182.
CrossRef - Raosoft.com.2016 Sample size calculator[Online] Available at http://www.raosoft.com/samplesize.html [Accessed on Feb.4, 2022]
CrossRef - Crilly P, Patel N, Ogunrinde A et al. Community pharmacists’ involvement in research in the United Kingdom. Pharmacy. 2017;5(3):48.
CrossRef - Tan WL, Siti R, Shahfini I et al. Knowledge, attitude and practice of antibiotics prescribing among medical officers of public health care facilities in the state of Kedah, Malaysia. Med J Malays. 2015; 70(5):307–11.
- Huang Y, Gu J, Zhang M et al. Knowledge, attitude and practice of antibiotics: a questionnaire study among 2500 Chinese students. BMC medical education. 2013;13(1):1-9.
CrossRef - Eid SM, Boueiz A, Paranji S et al. Patterns and predictors of proton pump inhibitor overuse among academic and non-academic hospitalists. Internal medicine. 2010;49(23):2561-8.
CrossRef - Mares-García E, Palazón-Bru A, Martínez-Martín Á et al. Non-guideline-recommended prescribing of proton pump inhibitors in the general population. Current medical research and opinion. 2017;33(10):1725-9.
CrossRef - Kaplan GG, Bates D, McDonald D et al. Inappropriate use of intravenous pantoprazole: extent of the problem and successful solutions. Clinical Gastroenterology and Hepatology. 2005;3(12):1207-14.
CrossRef - Heidelbaugh JJ, Nostrant TT, Kim C, Harrison RV. Management of Gastro esophageal Reflux Disease. American Family Physician. 2003;68(7):1311-1319.
- van den Bemt PM, Chaaouit N, van Lieshout EM et al. Noncompliance with guidelines on proton pump inhibitor prescription as gastroprotection in hospitalized surgical patients who are prescribed NSAIDs. European journal of gastroenterology & hepatology. 2016;28(8):857-62.
CrossRef - Patel HR, Dhande PP. Imprudent gastro-protective approach in majority of specialists’ clinics of a tertiary hospital. Journal of Clinical and Diagnostic Research (JCDR). 2016;10(3):FC12.
CrossRef - Wu B, Li D, Xu T et al. Proton pump inhibitors associated acute kidney injury and chronic kidney disease: data mining of US FDA adverse event reporting system. Scientific reports. 2021;11(1):1-8.
CrossRef - Yang Y, George KC, Shang WF et al. Proton-pump inhibitors use, and risk of acute kidney injury: a meta-analysis of observational studies. Drug design, development and therapy. 2017;11:1291.
CrossRef - Blume H, Donath F, Warnke A et al. Pharmacokinetic drug interaction profiles of proton pump inhibitors. Drug safety. 2006;29(9):769-84.
CrossRef







