Manuscript accepted on :12-06-2023
Published online on: 05-07-2023
Plagiarism Check: Yes
Reviewed by: Dr. Dito Anurogo and Dr. Anjaneyulu Konuri
Second Review by: Dr. Sonal Deshpande
Final Approval by: Dr. Eman Refaat Youness
Drobchak M1 , Kitsera N1,2
, Kitsera N1,2 , Osadchuk Z1
, Osadchuk Z1 , Kech N1
, Kech N1 , Bondarenko M2
, Bondarenko M2 and Kozovyi R2
and Kozovyi R2
1Institute of Hereditary Pathology, National Academy of Medical Sciences of Ukraine, Lviv, Ukraine
2Ivano-Frankivsk National Medical University, Ivano-Frankivsk, Ukraine.
Corresponding Author E-mail: nkitsera@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2690
Abstract
Prader-Willi syndrome (PWS) is a genetic disease characterized by mental retardation, as well as autism spectrum disorders, obesity and mood disorders. The aim of our study was to research a spectrum of genetic heterogenity and different clinical neurodevelopmental manifestations. Materials and methods: clinical, molecular, genetic and psychological methods were used. We observed 9 children (5 boys and 4 girls) with Prader-Willi syndrome from Lviv and Ivano-Frankivsk regions (Western Ukraine) who were diagnosed and followed-up at the Institute of Hereditary Pathology, National Academy of Medical Sciences of Ukraine, Lviv, for 4 years (2019–2022) and underwent molecular genetic testing. The ages of children ranged from 1 month to 7 years, with the mean value amounting to 3.6 years of age. Results: Our study revealed that 6 (66.7%) out of 9 children with PWS had birth defects. At ultrasound during pregnancy, we observed certain clinical features of the fetus, including fetal intrauterine development delay –5 (55.5%), and higher nuchal translucency measurement – 3 (33.3%). According to the checklist of autism spectrum disorders (CASD), 3 of the examined children with autism syndrome were at risk and required further monitoring, while 5 children scored 18-20 points, which indicated the presence of autistic spectrum and required in-depth monitoring during diagnosis. Stereotypical and repetitive play as a manifestation of problems with social interaction was observed in 3 boys with PWS. In our study, parents had no complaints about aggressive behavior in children with this syndrome. Conclusions: In cases if the children have signs of autism or developmental delay, they should undergo genetic counseling.
Keywords
Birth Defects; Clinical Manifestations; Prader-Willi Syndrome; Neurodevelopmental Disorders
Download this article as:| Copy the following to cite this article: Drobchak M, Kitsera N, Osadchuk Z, Kech N, Bondarenko M, Kozovyi R. Neurodevelopmental Manifestations and Birth Defects in Prader-Willi Syndrome: Findings from a Study in Western Ukraine. Biomed Pharmacol J 2023;16(2). |
| Copy the following to cite this URL: Drobchak M, Kitsera N, Osadchuk Z, Kech N, Bondarenko M, Kozovyi R. Neurodevelopmental Manifestations and Birth Defects in Prader-Willi Syndrome: Findings from a Study in Western Ukraine. Biomed Pharmacol J 2023;16(2). Available from: https://bit.ly/3PDfdYk |
Introduction
Prader-Willi syndrome (PWS) is the most common genetic obesity syndrome with associated neuroendocrine deficits, learning difficulties and behavioural and psychiatric problems. Hormonal deficiencies and metabolic complications cause early physiological and neurodevelopmental disorders. This genetic syndrome is caused by a lack of paternally derived imprinted material on chromosome 15q11–q13 1.
The frequency of PWS ranges from 1/10,000 to 1/30,000. This syndrome is present in both women and men, in all ethnic groups and races of our planet 2. PWS is caused by the absence of paternally expressed genes on chromosome 15q11–13. Most often, part of the father’s 15th chromosome is deleted in 70-75% of cases in children with PWS syndrome. In the remaining 20-25% of cases, the patient has two copies of maternal chromosome 15 from the mother and no paternal copy 1. Since parts of the maternal chromosome are disabled through imprinting, they do not have working copies of certain genes 3.
Many individuals with PWS also have co-occurring psychosis, autism spectrum disorders (ASDs), dysregulated sleep and eating and mood disorders. PWS is very often characterized by irritability, tantrums, compulsive behaviors, hyperphagia, growth hormone dysregulation. Patients with PWS require attention because they have a big problem with food-seeking behaviors, needs, compulsions and other neurodevelopmental disorders 4,5.
Since there is no screening of newborns for this pathology in Ukraine, the clinical manifestations of this syndrome may not be noticed by parents or doctors in the early stages of the disease. As PWS is accompanied by various birth defects, such children are seen by different doctors. Most often, parents and doctors pay attention when a child has a speech disorder over the age of 3.
The aim of our study wastodescribe cases of Prader-Willi Syndrome in both sexes with mutations and different clinical neurodevelopmental manifestations.
Materials and methods
We observed 9 children (5 boys and 4 girls) with Prader-Willi syndrome from Lviv and Ivano-Frankivsk regions (Western Ukraine) who were diagnosed and followed-up at the Institute of Hereditary Pathology, National Academy of Medical Sciences of Ukraine, Lviv, for 4 years (2019–2022) and underwent molecular genetic testing. The ages of children ranged from 1 month to 7 years, with the mean value amounting to 3,6 years. The final diagnosis of PWS was given to 8 children aged 3-7 years. PWS was confirmed by a molecular genetic method at the age of 1 month only in one girl.
Inclusion criteria included children with sedentary lifestyle, muscle hypotonia, mental retardation.
Exclusion criteria encompassed patients with obesity and without neurodevelopmental disorders, without molecular genetic confirmation of PWS.
PWS was suspected in 21 patients, thus the parents turned to a geneticist for consultation. Due to the war started by the aggressor country Russia, 4 children were forced to leave Ukraine and emigrate abroad. The parents of 5 children went to defend their native land from the enemy, so the problem of establishing an accurate diagnosis receded into the background. Three mothers refused to undergo molecular genetic testing due to the stress experienced by their children after missile attacks in other regions of Ukraine. Therefore, the group size is small (9 children with molecular genetic tests), and the study only focuses on children from two regions in Western Ukraine.
The control group consisted of 30 practically healthy children (13 girls and 17 boys) aged 2-5 without birth defects and neuropsychological disorders.
During the study, we have used the following:
card for monitoring the child’s behavior; it included data on gross motor skills and visual-motor coordination, balance, lateralization (main arm/leg), response to hearing, manual skills, graphomotor skills, aggressive and auto-aggressive behavior, relationship with the therapist, imitation, concentration of attention, child’s behavior during the visit.
Checklist for Autism Spectrum Disorder (CASD) for autism assessment with high reliability and accuracy 7. We used CASD as a fast and reliable method for screening children’s diagnosis to identify the level and degree of manifestation of neurodisorder in PWS. The Questionnaire for Autism Spectrum Disorders (CASD) included 30 symptom-questions that determined the child’s behavior problems in 6 areas:
Problems with social interaction;
Obsessive actions (perseveration);
Body-sensory (somatosensory) disorders;
Deviation in communication and development;
Mood disorder;
Problems with attention and understanding of danger.
A questionnaire for parents to assess the degree of development of all of the child’s communicative personality qualities and interpersonal relationships, designed for expert assessment of the communicative personality qualities of children, as well as their relationships with the surrounding people.
Cytogenetic and molecular-genetic analyses (FISH), DNA methylation.
Since the CASD is one of the auxiliary tools in the diagnosis of a neurodisorder, all 9 children with PWS were additionally consulted by a psychologist and a psychiatrist. The findings of these specialists during a more in-depth psychodiagnostic examination confirmed the key symptoms of the neurodisorder and the specifics of their manifestation.
The obtained data were standardized according to the Tenth Revision of the International Classification of Diseases (ICD – 10) and processed using the variational statistics method, the “Statistica 5” program package, and Microsoft Excel – 2000: the study considered the arithmetic mean value (M), deviations from the arithmetic mean value (m), the value of statistical significance (p) 6.
Clinical manifestations and molecular results were collected from the medical records of the patients. All study personnel data were anonymized prior to the analysis.
Informed written consent was obtained from the parents of all participants. The present research was conducted following the Declaration of Helsinki principles and approved by the Bioethics Committee of SI «Institute of Hereditary Pathology, National Academy of Medical Sciences of Ukraine», Lviv, Ukraine, № 71, 02.03.2023.
Results
The socio-economic status of the families was of average wealth and did not affect the access and availability of medical services until February 2022. All plans were interrupted by the war with Russia, which insidiously attacked our land, began bombing peaceful towns and villages, destroyed power plants in order to isolate Ukrainians from normal living conditions.
Parents consulted a geneticist because they saw that their child was lagging behind peers for various reasons (Table 1). Among the 9 children, 5 had developmental delays up to one year, which their parents noticed, such as problems with swallowing (1 boy and 1 girl), sedentary child (1 boy and 1 girl), obesity (1 boy and 1 girl). Although only the parents of 2 children complained of excess weight, obesity was diagnosed in 6 children during the endocrinologist’s consultation. At the age of 3.5, the bone X-ray of patient K. (case 3 – 46 ХХ, upd(15)mat) corresponds to the child’’s age of 1 year and 9 months. At the same time, the X-ray of the hands of patient A. (case 2 – 46 ХY, ish del (15)(q11-13)(D15S10-, D15Z1+, PML+) aged 9, exceeded the age norm and corresponded to a 12-year-old child.
In the maternity hospital, birth defects due to ICD-10-CM were diagnosed in 4 boys and 1 girl with PWS: cryptorchidism (Q.53) in 3 cases, congenital shortening of upper limb, bilateral (Q.71.81) and other congenital malformations of vulva (Q52.7). In addition to cryptorchidism, one boy was also diagnosed with congenital malformations and deformations of the musculoskeletal system, namely congenital dislocation of left hip (Q.65.0) and right congenital torticollis (Q.68.01). Birth defects of the heart were diagnosed in two children under 1 year of age. The girl (case 8 -46, XX, del (15) (q11.2-12.2)) was diagnosed with an atrial septal defect (Q.21.1), the boy (case 7 -46 ХY, del (15) (q11.2-13)) was diagnosed with a ventricular septal defect (Q.21.0) along with a previously diagnosed birth defect.
In our study, PWS had a multifaceted and complex clinical appearance. Usually, problems with swallowing arose in the first days after the birth of a child. One boy even had a feeding tube used because the child was sedentary and had muscle hypotonia. Muscular system pathology was most often observed in children, it was present in 7 (77.8%) cases: muscular hypotonia, hip dysplasia, scoliosis; while damage to the gastrointestinal tract was the least observed, it was present in 2 (22.2%) girls: chronic constipation (case 5 – 46 ХХ, ish del (15) (q11-13) (SNRPN)) and hepatomegaly (case 3 – 46 ХХ, upd(15)mat). Hyperphagia is a pervasive problem affecting individuals with PWS that increases with age. Disturbances from the endocrine (goiter and/or obesity) and ophthalmological systems (most often strabismus) were found in 5 (55.6%) children.
According to the statistical data, the average age of mothers at the birth of their first child in Ukraine is 26.2 years 8. In our study, the age of mothers who gave birth to a child with PWS ranged from 22 to 36 years (Table 2), and the average was 25.1±4.4 years of age. No statistical difference was found regarding the age of the mothers of the control group – 24.9±5.1 (р>0.05). The mother D. gave birth to a healthy son from her first pregnancy, and from her second pregnancy, at the age of 22, a boy with PWS (case 4 – 46, XY.ish del(15)( q11-13)(D15Z1+, D15S10-, PML+).
Studying the reproductive anamnesis of the mothers, it was established that it was the first pregnancy for 5 (55.6%) women. It was the second pregnancy for two women, and a healthy child was born from the first one. In a 36-year-old woman, it was the 4th pregnancy, where the girl was diagnosed with PWS at 1 month. Healthy children were born from the previous three pregnancies from another husband.
Among the 9 surveyed families and the control group, there were no consanguineous marriages. Only in 1 (11.1%) case was there a delay in mental and physical development in the cousin on the mother’s line. In the remaining 8 families, such pathology was absent. 6 (66.7%) women had contractions during pregnancy. Most often, women noticed the inactivity of the fetus. In 3 (33.3%) women, the pregnancy was uneventful. At ultrasound during pregnancy, only two women had no obvious pathology of the fetus and placenta. Higher nuchal translucency measurement, sedentary fetus, in combination with fetal intrauterine development delay was observed in 3 (33.3%) cases.
In 4 (44.4%) cases, the pregnancies ended with cesarean section. The weight of the fetus varied from 2800 to 3700 g (average weight – 3212.2±295.5 g). The height of children who were subsequently diagnosed with PWS ranged from 48 to 53 cm, with the average value equaling 50.4±1.5 cm. No statistical difference (р>0.05) was found regarding the weight (3180.4±321.7 g) and height (50.1±2.2 cm) of the children in control group in comparison with patients with PWS. A cesarean section was performed on a pregnant woman with preeclampsia, the child was born weighing 2800 g (case 1). Only at the age of 5, due to molecular genetic testing, the boy was diagnosed with PWS (case 6 – 46 ХY, arr 15q11.2).
According to the questionnaire for parents, the main complaints of the parents were hyperphagia and problem behavior, which contributed to the deterioration of the well-being and quality of life of both the child and relatives. Parents of children with PWS emphasized the fact that they must constantly take care of the child, pay attention to its nutrition and changes in mood and behavior.
In our group the neurodevelopmental disordersand pathogenic gene spectrum between patients were different (Table 3). Only in one case, in a newborn, a 1-month-old girl (case 1) with muscular hypotonia and sedentary behavior was diagnosed with PWS using molecular genetic testing – 46, XX, rsa 15q11.2(P245)x1.
Specialists suspected the diagnosis of autism in several children (cases 2, 4, 5), therefore, along with other methods, a Questionnaire on Checklist for Autism Spectrum Disorder (CASD) was used. It should be noted that impaired neurodevelopment of a child can be one of the causes of syndromic autism. Each Questionnaire on CASD was scored 1 point in the presence of certain developmental abnormalities, while normal development of the child was defined as 0 points (Table 3). The procedure for examination of children with PWS was carried out individually. The duration of a one-time meeting was determined by the individual needs and capabilities of the child and lasted 30-50 minutes on average.
The total number of points according to the results of the survey for children with PWS determined the risk of the autistic spectrum disorder at 15 points. Accordingly, a higher number of points (> 15) scored on this survey corresponded to a moderate and severe degree of autism. Therefore, 3 of the examined children with PWS are at risk and need further monitoring, while 5 children scored 18-20 points, which indicates the presence of autism spectrum and requires in-depth diagnosis and long-term treatment. In our study, this test was not performed in 1 girl (case 1 – 46, XX, rsa 15q11.2(P245)x1), as the diagnosis was made at the age of 1 month. The oldest among the children who were tested was a 7-year-old boy (case 9 -46 ХY, ish del (15) (q11.2-12)), who scored 14 points.
Children with PWS have problems with social interaction – most of the children observe play with peers, but do not interact with them. In 5 children (cases 2, 4, 5, 6, 7) with this syndrome, limited interpersonal interaction was found, 3 children (cases 5, 6, 7) needed additional motivations to establish visual contact, and 2 boys (cases 2, 4) did not look into the eyes of the interlocutor at all (Table 3). Egocentrism was clearly traced in two children (cases 2, 4) – they did not pay attention to the presence of others and understood the manifestations of social interaction poorly.
Stereotypical and repetitive play as a manifestation of the disorder was observed in 3 boys with PWS (cases 2, 4, 7). Parents also noted that these children often had unusual repetitive movements, such as clapping the palms in excitement. Among the somatosensory disorders, atypical craving for twisting and rocking were noted in two boys (cases 2, 4). In our study 3 girls and 2 boys (cases 3, 4, 5, 6, 8, 9) had problems with nutrition, in particular the inability to chew hard and large pieces, and to keep food in the mouth for a long time without swallowing it. Only 2 girls and 1 boy (cases 3, 8, 9) did not show hypersensitivity to certain sounds. Parents observed sleep disorders in 3 children (cases 5, 6, 7).
All children experienced atypical communication and development, which were manifested by varying degrees of deceleration of language development and limitation of spoken speech. 3 children (cases 5, 6, 7) had mood swings and hyperactivity. Emotional lability was inherent in 3 boys (cases 2, 4, 7). There were no difficulties with the expression and recognition of emotions in 2 girls and 1 boy (cases 3, 8, 9). The ability to focus excessively on a particular activity or object was observed in 3 children (cases 7, 8, 9), the other 5 children had problems with attention and personal safety. Impulsiveness was inherent in 2 girls and 3 boys (cases 2-6), 2 boys and 1 girl (cases 7, 8, 9) were fussy.
Most often, neurodevelopmental disorders with the condition of children assessed at 20 points, were observed in boys aged 3 (case 4 -46, XY.ish del(15)( q11-13)(D15Z1+, D15S10-, PML+)) and 4 (case 2 -46 ХY, ish del (15)(q11-13)(D15S10-, D15Z1+, PML+)).
In our study, different genotypes seemed to account for the difference in phenotype in PWS patients. We found a delay in time of the diagnosis in these patients, although the majority of children had neonatal hypotonia and other suggestive phenotypic features, again emphasizing the need for increased awareness of this syndrome as well as genetic counseling.
In children with PWS, the course of the pathology may be accompanied by symptoms from other organs and systems (digestive, skin, ophthalmic, skeletal-muscular, endocrine, cardiac and hepatobiliary systems), which are often left out attention of clinicians. According to the data of the individual development program of the child with PWS, specialists selected appropriate rehabilitation measures that focused on the development of the emotional and volitional sphere, sensory, motor and language activities. 3 months after the classes, 5 (55.6%) parents noticed an improvement in the child’s condition. In 2 (22.2%) children, the slow progress of social skills and the development of the emotional and volitional sphere were noted. However, in 2 (22.2%) children who previously worked with specialists, regression was observed due to frequent anxiety attacks caused by the war in Ukraine, which occurred 3-4 times a day and lasted up to 1.5-3 hours. Children and parents experienced post-traumatic stress disorder. After the children were diagnosed with PWS, they were referred to specialists of various profiles (ophthalmologist, neurologist, endocrinologist, psychologist) and received treatment as needed. Appropriate treatment for various manifestations of PWS was prescribed by doctors of various profiles, in particular, 2 patients were prescribed somatotropic hormone.
 |
Table 1: Clinical manifestations of Prader-Willi syndrome in children. |
Table 2: Peculiarities of the reproductive history of mothers of children with Prader-Willi syndrome
|
Case |
Reproductive Anamnesis |
Family History |
Pregnancy |
USG during Pregnancy |
Mother’s age at delivery |
Delivery |
Weight, g |
Hight, cm |
|
1
|
3 pregnancies – three healthy children from another man |
no |
reduced fetal movements |
delay in intrauterine development of the fetus |
36 |
breech birth |
2800 |
52 |
|
2 |
– |
yes |
anemia, grade II, chronic tonsylit, chronic cholecystitis |
higher measurement of nuchal translucency, reduced fetal movements, delay in intrauterine development of the fetus |
22 |
caesarean section |
3460 |
51 |
|
3 |
– |
no |
reduced fetal movements |
delay in intrauterine development of the fetus |
25 |
breech birth |
3400 |
49 |
|
4 |
1 healthy son |
no |
normal |
higher measurement of nuchal translucency, reduced fetal movements, delay in intrauterine development of the fetus |
22 |
normal |
3400 |
51 |
|
5 |
1 miscarriage |
no |
gestosis |
higher measurement of nuchal translucency, reduced fetal movements, delay in intrauterine development of the fetus |
23 |
caesarean section |
3000 |
48 |
|
6 |
– |
no |
anemia grade I, gestosis |
reduced fetal movements |
24 |
caesarean section |
2950 |
50 |
|
7 |
1 healthy daughter |
no |
normal |
normal |
27 |
normal |
3200 |
50 |
|
8 |
– |
no |
normal |
normal |
24 |
caesarean section |
3700 |
53 |
|
9 |
– |
no |
reduced fetal movements |
reduced fetal movements |
23 |
normal |
3000 |
50 |
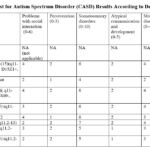 |
Table 3: Checklist for Autism Spectrum Disorder (CASD) Results According to Detected Mutations |
Discussion
PWS is a multi-system genetic disorder caused by chromosomal changes in segment 15q11-q13, individuals with this syndrome usually present in neonatal period with poor sucking with hypotonia, developmental delay, mental, behavioral symptoms and a specific physical phenotype. In our study, we reported the results of the genetic analysis, clinical features and neurodevelopmental disorders in children with PWS that match the data 9. Typical PWS manifestations in our 9 infants included hypotonia – 5 (55.6%), absence of sucking and swallowing reflexes – 2(22.2%), breech birth – 2(22.2%) and reduced fetal movements – 5(55.6%). Mothers of children with PWS with hypotonia noted that they had difficulty in feeding the babies immediately after birth. After examination by doctors, feeding tube was used in 2 cases.
In our study, at ultrasound during pregnancy, we observed certain clinical features of the fetus, including fetal intrauterine development delay – 5 (55.5%) and higher nuchal translucency measurement – 3 (33.3%). Our study indicates that the pathology was not detected in 2 (22.2%) pregnant women during the ultrasound examination.
Similar to our subject, experts note that reduced fetal movements, malpresentation of the fetus, severe intrauterine growth restriction include the prenatal sonographic phenotype of PWS. Since these findings are not specific for PWS, however, the combination of some of them (especially severe intrauterine growth retardation and polyhydramnios) may prompt clinicians to perform invasive testing leading to prenatal molecular cytogenomic diagnosis 10.
According to Italian doctors 11 newborns with PWS in 1988-2018 showed a lower average birth weight by 1/2 kg and a shorter average birth height by 1 cm than healthy newborns. In contrast, in our study, only 1 girl was born with a weight of 2800 g, all other children weighed more than 3000 g. Another girl, who was born by caesarean section, was 48 cm of height and weighed 3000 g, which met the neonatal anthropometric standards.
Argentinian physicians indicate that 22% patients with PWS had birth defects, with a risk 5.4 to 18.7 times higher than the general population 12. Doctors from the Netherlands indicate the presence of cryptorchism in 95.9% of boys 13. Our study revealed that 6 (66.7%) out of 9 children with PWS, had birth defects: 5 malformations were diagnosed in the maternity hospital, and 1 other child had a heart defect diagnosed during the year of observation.
Our data are consistent with the study by scientists who report that hypotonia, hypophagia, and abnormal genital development are common characteristics of neonates with PWS in the Chinese population 14. In our study, after the birth of the child, the mother observed inactivity, lethargy, lack of sucking reflex, so the doctors suspected PWS (case 1). Since the clinical signs were strongly suggestive of PWS, the mother was strongly recommended to do molecular genetic testing of her daughter. As parents point out, they are most concerned about hyperphagia and obesity in children with PWS, as well as difficulties with sleep, as it violates the family life. In addition, such children have problem with visual-spatial functions. In our group, the main clinical characteristics were represented by short stature, obesity, muscular hypotonia, developmental delay, cognitive disability and behavioral diseases.
As doctors note, the diagnosis is not always possible to make in time, and 14.3% of patients were diagnosed with PWS at the age of 4-10 years 9. In our study, 5 (55.5%) children aged 4-7 years were given this diagnosis.
A high degree of variability in clinical severity is observed within PWS, across clinical features such as language and motor function. Our observations regarding clinical manifestations coincide with the data of doctors, who note that PWS is accompanied by neuroendocrine disorders, as well as behavioral and psychiatric problems 5,15.
This study also illustrates the potential importance of early diagnosis and careful detection of ophthalmic pathology, since 5 (55,5%) children were diagnosed with strabismus, astigmatism and swelling of the optic nerve discs of both eyes. Our data are consistent with the Global PWS Registry (USA), where the prevalence of strabismus, amblyopia, and hyperopia are considerably higher in the PWS population represented 16.
Scientists from the Netherlands note that 17% of patients with ASD have hypothyroidism 17. In contrast, in our group of 9 children, 4 (44.4%) were diagnosed with goiter. Perhaps this is due to the fact that the Lviv and Ivano-Frankivsk regions belong to the goitre endemic zone.
Sleep disturbances in children with PWS are indicated by many authors 18,19, in particular, in our group, the parents of 3 children drew attention to this symptom.
Maladaptive behaviors among 9 children with Prader-Willi syndrome were assessed using the Checklist for Autism Spectrum Disorder. Studying the psychological characteristics of patients in our group, it was established that 5 children were included in the autism risk group according to the Checklist for Autism Spectrum Disorder. Patient С. (case 3) with mutation 46XX,upd(15)mat, which was detected by DNA methylation, was found to have a low level of probability of autism. There are observations that indicate the positive role of training game exercises when children with PWS were involved in them 20.
Patients with different mutations were diagnosed with different levels of neurodevelopmental disorders 4. At that time, many articles described the presence of aggressive behavior in children 6,21, but in our study, parents had no complaints about this.
Among 9 children there were no seizures, although they were examined by doctors, which is supported by the data of researchers who did not find a reliable difference between epileptic seizures and this genetic syndrome 22.
Our observations are consistent with other authors who point to repetitive interests and behaviors of such children. This is especially noticeable at the doctor’s appointment, when the child sees a picture on the wall in the office and asks something dozens of times. Since PWS is a neurodevelopmental disorder associated with social cognitive challenges, the behavior of children with PWS has a significant and dramatic impact on the daily functioning and quality of life of the patient and their families. After a period of impaired social sensitivity, they develop behavioral problems such as temper tantrums, stubbornness, and excessive foraging. According to the observations of Australian doctors on 50 patients with PWS, such persons require intensive supervision by relatives, which can negatively affect the quality of life of all family members 19.
Our study revealed that 6 (66.7%) out of 9 children with PWS had birth defects: 5 malformations were diagnosed in the maternity hospital, and 1 other child had a heart defect diagnosed during the year of observation.
At ultrasound during pregnancy, we observed certain clinical features of the fetus, including fetal intrauterine development delay – 5 (55.5%) and higher nuchal translucency measurement – 3 (33.3%).
According to the checklist of autism spectrum disorders (CASD), 3(33.3%) of the examined children with autism syndrome are at risk and require further monitoring, and 5(55.5%) children scored 18-20 points, which indicates the presence of an autistic range and requires in-depth monitoring during diagnosis.
A multisystem approach should be applied to families with a child with PWS, which includes consultation with doctors of various specialties, such as neurologists, genetics, endocrinologists, psychologists, ophthalmologists, nutritionists, etc.
At the moment the issue of improving the algorithm for early diagnosis of impaired neurodevelopment in children caused by genetic and hereditary diseases remains unresolved. Our findings may increase clinical awareness of the early clinical signs of PWS, enabling early diagnosis and start of multidisciplinary treatment.
Conclusion
Our study revealed that 6 (66.7%) out of 9 children with PWS had birth defects.
At ultrasound during pregnancy, we observed certain clinical features of the fetus, including fetal intrauterine development delay – 5 (55.5%) and higher nuchal translucency measurement – 3 (33.3%).
According to the checklist of autism spectrum disorders (CASD), 3(33.3%) of the examined children with autism syndrome are at risk and require further monitoring, and 5(55.5%) children scored 18-20 points, which indicates the presence of an autistic range and requires in-depth monitoring during diagnosis.
A multisystem approach should be applied to families with a child with PWS, which includes consultation with doctors of various specialties, such as neurologists, genetics, endocrinologists, psychologists, ophthalmologists, nutritionists, etc.
In cases if the children have signs of autism or developmental delay, they should undergo genetic counseling.
Conflict of Interest
The authors have no conflicts of interest to declare.
Funding Sources
Authors state no funding involved.
Literature
- Angulo MA, Butler MG, Cataletto ME. Prader-Willi syndrome: a review of clinical, genetic, and endocrine findings. J Endocrinol Invest. 2015;38(12):1249-1263. doi:10.1007/s40618-015-0312-9
CrossRef - Bohonowych J, Miller J, McCandless SE, Strong TV. The Global Prader-Willi Syndrome Registry: Development, Launch, and Early Demographics. Genes (Basel). 2019;10(9):713. doi:10.3390/genes10090713
CrossRef - Wu J, Lei M, Wang X, et al. Prader-Willi syndrome patient with atypical phenotypes caused by mosaic deletion in the paternal 15q11-q13 region: a case report. Ital J Pediatr. 2022;48(1):204. doi:10.1186/s13052-022-01398-0
CrossRef - Lavryk AS, Pylypenko VM, Halych SP, et al. Prader-Willi syndrome: new opportunities in treatment of adolescents and adults. Problems of Endocrine Pathology.2022;79(1):43-49.
- Schwartz L, Caixàs A, Dimitropoulos A. et al. Behavioral features in Prader-Willi syndrome (PWS): consensus paper from the International PWS Clinical Trial Consortium. J Neurodevelop Disord.2021; 13 (25). https://doi.org/10.1186/s11689-021-09373-2
CrossRef - Walters SJ, Campbell MJ, Machin D. Medical Statistics: A Textbook for the Health Sciences, 5th Edition. Wiley-Blackwell, 2021: 448 p.
- Mayes S. Checklist for Autism Spectrum Disorder (CASD) [Database record]. APA PsycTests. 2012. https://doi.org/10.1037/t03996-000
CrossRef - Mother’s mean age at first birth. https://www.cia.gov/the-world-factbook/
- Çizmecioğlu FM, Jones JH, Paterson WF, et al. Neonatal Features of the Prader-Willi Syndrome; The Case for Making the Diagnosis During the First Week of Life. J Clin Res Pediatr Endocrinol. 2018;10(3):264-273. doi:10.4274/jcrpe.0029
CrossRef - Yang L, Zhou Q, Ma B, et al. Perinatal features of Prader-Willi syndrome: a Chinese cohort of 134 patients. Orphanet J Rare Dis. 2020;15(1):24. doi:10.1186/s13023-020-1306-z
CrossRef - Salvatoni A, Moretti A, Grugni G, et al. Anthropometric characteristics of newborns with Prader-Willi syndrome. Am J Med Genet A. 2019;179(10):2067-2074. doi:10.1002/ajmg.a.61304
CrossRef - Torrado M, Foncuberta ME, Perez MF, et al. Change in prevalence of congenital defects in children with Prader-Willi syndrome. Pediatrics. 2013;131(2):e544-e549. doi:10.1542/peds.2012-1103
CrossRef - Grootjen LN, Uyl NEM, van Beijsterveldt IALP, et al. Prenatal and Neonatal Characteristics of Children with Prader-Willi Syndrome. J Clin Med. 2022;11(3):679. doi:10.3390/jcm11030679
CrossRef - Ge MM, Gao YY, Wu BB, et al. Relationship between phenotype and genotype of 102 Chinese newborns with Prader-Willi syndrome. Mol Biol Rep. 2019;46(5):4717-4724. doi:10.1007/s11033-019-04916-2
CrossRef - Azor AM, Cole JH, Holland AJ, et al. Increased brain age in adults with Prader-Willi syndrome. Neuroimage Clin. 2019;21:101664. doi:10.1016/j.nicl.2019.101664
CrossRef - Bohonowych JE, Vrana-Diaz CJ, Miller JL, et al. Incidence of strabismus, strabismus surgeries, and other vision conditions in Prader-Willi syndrome: data from the Global Prader-Willi Syndrome Registry. BMC Ophthalmol. 2021;21(1):296. doi:10.1186/s12886-021-02057-4
CrossRef - Pellikaan K, Snijders F, Rosenberg AGW, et al. Thyroid Function in Adults with Prader-Willi Syndrome; a Cohort Study and Literature Review. J Clin Med. 2021;10(17):3804. doi:10.3390/jcm10173804 CrossRef
- O’Hora KP, Zhang Z, Vajdi A, et al. Neurobehavioral Dimensions of Prader Willi Syndrome: Relationships Between Sleep and Psychosis-Risk Symptoms. Front Psychiatry. 2022;13:868536. doi: 10.3389/fpsyt.2022.868536.
CrossRef - Mackay J, Nixon GM, Lafferty AR, et al. Associations Between Hyperphagia, Symptoms of Sleep Breathing Disorder, Behaviour Difficulties and Caregiver Well-Being in Prader-Willi Syndrome: A Preliminary Study. J Autism Dev Disord. 2022;52(9):3877-3889. doi: 10.1007/s10803-021-05265-5.
CrossRef - Dimitropoulos A, Doernberg EA, Russ SW, Zyga O. Intervention Response by Genetic Subtype: PRETEND-Preschool Program for Children with Prader-Willi Syndrome via Remote Parent Training. J Autism Dev Disord. 2022;52(12):5191-5206. doi: 10.1007/s10803-022-05695-9.
CrossRef - Kennedy D, Marten H, O’Sullivan C, Catrone R. Biological, Behavioral, and Ethical Considerations of Prader-Willi Syndrome: A Primer for Behavior Analysts. Behav Anal Pract. 2021;15(2):562-570. doi:10.1007/s40617-021-00618-z
CrossRef - Elia M, Rutigliano I, Sacco M, et al. EEG Patterns in Patients with Prader-Willi Syndrome. Brain Sci. 2021;11(8):1045. doi:10.3390/brainsci11081045
CrossRef







