Manuscript accepted on :14-03-2023
Published online on: 04-07-2023
Plagiarism Check: Yes
Reviewed by: Dr. Mario Vincenzo Russo and Dr. Patel Maulik
Second Review by: Dr. M Mohan Varma
Final Approval by: Dr. Patorn Piromchai
Basma Abdallah1,2,3,4 , Hassan Ait Benhassou1
, Hassan Ait Benhassou1 , Laila Sbabou2
, Laila Sbabou2 , Régine Janel-Bintz4
, Régine Janel-Bintz4 , Laurence Choulier3
, Laurence Choulier3 , Véronique Pitchon5
, Véronique Pitchon5 and Pierre Fechter4*
and Pierre Fechter4*
1Prevention & therapeutics center, Moroccan Foundation for Science, Innovation & Research (MAScIR), Rabat, Morocco.
2Laboratory of Microbiology and Molecular Biology, University Mohamed V Rabat, Faculty of Sciences, Rabat, Morocco
3CNRS, UMR 7021, Laboratoire de Bioimagerie et Pathologies, Faculté de Pharmacie, Université de Strasbourg, 67401 Illkirch, France
4CNRS, UMR 7242, Biotechnologie et Signalisation Cellulaire, Institut de Recherche de l’Ecole de Biotechnologie de Strasbourg, Université de Strasbourg, 67400 Illkirch-Graffenstaden, France
5CNRS, UMR7044, Archéologie et Histoire Ancienne : Méditerranée- Europe, MISHA, Université de Strasbourg, Strasbourg, France
Corresponding Author E-mail: p.fechter@unistra.fr
DOI : https://dx.doi.org/10.13005/bpj/2656
Abstract
The proliferation and prevalence of antibiotic-resistant bacteria despite modern medicine is considered as one of the most alarming threats to global health. The fear that antibiotics that work today might not work tomorrow makes it imperative to search and develop novel drugs or therapeutic strategies to fight against micro-organisms resistant to our current approaches. From many centuries, people have sought solutions to combat infections and proposed countless remedies, traces of which can be found in manuscripts preserved over the past centuries. The re-examination and exploitation of these ancient remedies might be a key to a vast pool of potential therapeutic strategies or drug candidates against antibiotic-resistant pathogens. This, however, would first require the consideration of these ancient solutions as scientifically pertinent leads for new therapies. The aim of this review is to highlight arguments in favor of a rationality in the scientific approach of these past physicians as well as of a medicinal interest in studying these ancient pharmacopeias. To narrow the scope of our research, we focused on the Arab Medieval Golden Medical Age, which inspired occidental medicine hundreds of years after its preeminence. We further highlight the possibility of integrating this knowledge into innovative, modern therapeutic approaches.
Keywords
Antibiotic Resistance; Arab Medieval Pharmacopeia; Natural Remedies; Pathogens
Download this article as:| Copy the following to cite this article: Abdallah B, Benhassou H. A, Sbabou L, Bintz R. J, Choulier L, Pitchon V, Fechter P. History as a Source of Innovation in Antimicrobial Drug Discovery. Biomed Pharmacol J 2023;16(2). |
| Copy the following to cite this URL: Abdallah B, Benhassou H. A, Sbabou L, Bintz R. J, Choulier L, Pitchon V, Fechter P. History as a Source of Innovation in Antimicrobial Drug Discovery. Biomed Pharmacol J 2023;16(2). Available from: https://bit.ly/44slNVN |
Introduction
Pharmacy emerged from human efforts to relieve their physical suffering through remedies prepared with natural ingredients. Ancient and medieval pharmacopeias contain information on the use of medical material, that may be from plant, mineral, or animal origin. It is thus still possible that these thousand-year-old pharmacopeias hold secrets that could contribute to nowadays medicines. Many leading drugs (anticancer, antimalarial, painkillers, etc.) are indeed derived from these ancestral traditional pharmacopeias [1]. However, of the > 30,000 plants described in traditional pharmacopeias, less than 5,000 have been studied [2]. The question is whether and how to exploit this vast pool of potential therapeutics [3,4].
In the last decade, medicinal plant research has turned to old medicinal-botanical texts, to study the history and evolution of pharmacopeias, and to identify lead compounds for new drug discovery [5–8]. Despite this pivot in research focus, experiments that test the activities of entire historical remedies are rare, difficult to conduct, and the subject of much misunderstanding. This is due to several factors including:
The folkloric image associated with ancient medicines. It is difficult to evaluate remedies objectively due to the frequent intrusion of magical and sacred although their development remained rationally designed at its base. It may therefore be difficult to evaluate the biological effect of each ingredient. However, very often this interference is not constitutive, but superadded: the rational/irrational association can usually be clearly separated. Further, the diagnosis of a malady can also be complex, often involving supernatural aetiologies alongside natural causes. In contrast to modern medicine, which seeks a direct cause for a pathology, ancient systems often seek to flush out deep-seated causes. This disorganizes and devalues the care provided, which is nevertheless often rational.
The difficulty of transposing ancient practices into our present culture. This requires a huge interdisciplinary research effort alongside, a dialogue between disciplines, very well explained by Harrisson and Connelly [9]. Furthermore, on the opposite to current medicines containing a single active ingredient, medieval remedies are usually preparations made from several ingredients, acting synergistically [10–12]. It is thus possible that each ingredient taken individually does not carry a strong activity, but that the combination can bring a certain, desired effectiveness. Nonetheless, the effectiveness of a remedy, which is the sum of its multiple actions, will be more difficult to evaluate and to determine, and is not necessarily favored by current research.
The juxtaposition of two medicines, traditional and modern. While modern medicine gained power and prestige, traditional medicine felled victim to trivialization and/or the increasingly untrained bodies of people practicing it over the course of many years. This resulted in the degradation of ancient knowledge, and a more superficial scientific approach. It is thus necessary to restore confidence and rationality in the study of traditional medicines, and to find room for dialogue between both approaches, that are ultimately rather complementary than opposed, i.e. [13–17].
Although discredited in recent years, traditional medicines have nevertheless been marked throughout their history by a rationality, and a scientific approach that enabled the emergence of remedies that we could quite rightly consider as innovative by modern standards despite being designed millennia ago. It is important to remember that traditional practices were characterized by the seal of research, carried out by prominent scientists who led to major discoveries and developments. Ancient pharmacopoeias could again be considered as a relevant starting point for the search for new remedies. This will be illustrated through a few examples from the scientific literature. This review will focus on the medieval Arab period perceived as the golden age of ancient medicine, and through the lens of the fight against microbial infections, one of the major medical concerns of the medieval era.
Antibiotic resistance
Infections have marked human history. Today, aside from the COVID-19 pandemic, infections are considered less anxiety-provoking compared to other pathologies like cancer, but this was not always the case: at medieval times, drinking water, cutting, or injuring oneself could lead to dangerous or even fatal infections. As these infections were a daily preoccupation, physicians also developed many leading remedies to counter them [4].
The advent of antibiotics, with Fleming’s discovery of penicillin in 1928, a compound produced by the fungus Penicillium notatum, revolutionized the treatment of infections [18,19], leading to the belief that microbial infections were ‘over’. The use of traditional medicines was thus no longer relevant and lost much of its prestige. This was nevertheless regardless of the ability of bacteria to resist antibiotics. If microbes can produce antibiotics (most of the antibiotics used are of microbial origin), it is indeed logical that other microbes have found ways to resist these same antibiotics. The resistances have then spread widely with the unreasonable use of antibiotics, i.e. [20–22].
Bacteria strains resistant to antibiotics were detected quite quickly after their introduction to the market. This was the case for penicillin, with resistant Staphylococcus aureus found in the 1940s [23,24]. Streptococcus pyogenes resistant to sulfonamide was also readily detected in military hospitals during the second World War [25–27]. Mycobacterium tuberculosis with streptomycin resistance was revealed as well in 1948 [28]. Resistance to multiple drugs was first observed in the late 1950s to 1960s among enteric bacteria, like Escherichia coli, or other from the Shigella and Salmonella genus [29]. These resistances caused also a gradual re-emergence of pathologies like tuberculosis, since the 1980s, mainly due to multi-drug resistant strains, and was aggravated by the emergence of the human immunodeficiency virus [30].
As a consequence of the pervasiveness of the above bacterial strains, the emergence of antibiotic resistance has been rising rapidly all over the world. Ultimately, a new resistance appeared with every new antibiotic synthesized (Figure 1). We are therefore faced with a growing global health threat. In 2019, a study showed the involvement of antibiotic-resistant bacteria in the deaths of more than 1.2 million people [31]. This may be attributed to different factors, such as the abusive use of antibiotics, as well as a shortage of new drug development by the pharmaceutical industry, etc… [32].
In the fear that antibiotics that are effective today might no longer be functional tomorrow, and with the rapid spread of antibiotic resistance, there is an important need to develop new strategies to limit the use antibiotics and to find new therapeutic solutions. Ancient societies have used and/or combined countless natural substances to treat diseases, trying, testing, and improving these strategies over the course of many centuries. Thus, ancient methodologies could serve as basis for the discovery of novel therapeutic strategies. However, the establishment of interdisciplinary consortia dedicated to the study of these remedies must be implemented, as well as the demonstration of the interest, feasibility, and future prospects of such approaches.
Rationality in the design of remedies
If different studies already highlighted some interest in studying past remedies or highlighted antibiotic use from past records, i.e. [33–40], the consideration of these past remedies as a reservoir of pertinent strategies to combat infection would require more complex and coordinated strategies, involving intense collaboration between art, social and experimental sciences.
A pioneering interdisciplinary consortium (Ancientbiotic, https://ancientbiotics.co.uk/) has been set up to study a 10th Century medical text known as ‘Bald’s Leechbook’ containing a plentitude of remedies. From this book, a collyrae (Table 1) has been chosen to highlight the potential of these medicines to combat infections. The goal was to study the medical approaches of past physicians and to demonstrate the efficacy of an ancient remedy. By faithfully reproducing this remedy, the authors demonstrated that it drastically limited the growth of bacterial pathogens like Staphylococcus aureus, Pseudomonas aeruginosa or Neisseria gonorrhoeae in vitro, and/or on a mouse model of eye infection, with a reasonable safety profile [41–44].
The same study also showed that the mixture of ingredients in Bald’s eye drops is more effective than the addition of each individual components. This imply that the combination of specific ingredients, none of which may have significant antibacterial activity, may enhance their bioactivity. It seems thus possible that some of the combinations developed by these physicians were designed through rational methods. It could therefore be possible to construct remedies of significant therapeutic potential from a combination of ingredients that exhibit no significant bioactivity as isolated components. The idea would be to consider these ingredients in the context of all or part of the remedies, rather than investigating each ingredient individually.
As a follow-up of this study, the consortium also developed a software to analyze the entire manuscript in order to highlight the most promising remedies. Groups of ingredients were revealed, some of them often used together, such as aloe vera and sarcocolla [45]. Another recent computer analysis equally highlighted the recurring appearance of combinations of ingredients, like saffron and opium or fennel and celery seeds, when analyzing remedies for urinary tract diseases identified in different Arabic pharmacopeias spanning over the course of more than 3 centuries [46]. These re-occuring combinations point to a rational approach in the development of treatment remedies, where a base of certain ingredients would have been maintained and used as a framework for the design of new candidates. The same ingredients could produce synergistic activity if combined, and should deserve special attention. Thanks to these studies, it becomes more and more evident that the science of medicine in medieval times was the result of a very rational and scientific approach, far from the folkloric image it usually has. Further studies of remedies from other manuscripts and ancient practices will be required to confirm these initial hypotheses and/or to possibly allow the identification of innovative active principles from complex combinations or even unexpected materials [35,47].
While traditional remedies were developed from common ingredients, many remedies also contain toxic molecules, among which the most emblematic being heavy metals, such as lead, mercury, and arsenic. Reconsidering these remedies for future development requires to prove that ancient physicians perfectly mastered the use of these ingredients, took into account their toxicities, and did not take ill-considered risks concerning the health of their patients. For example, lead was widely used since antiquity to prepare make-up products (including kohl) or remedies. Two recent studies have analyzed these uses, based on makeup found in Egyptian tombs [48], and the reconstitution of a cutaneous remedy reported by Al Kindi (Table 1), from the medieval Arab period [49]. These two studies demonstrated that ancient alchemists mastered the transformation of metals and were able to confer them different therapeutic potentials, depending on the transformation processes used. In the “khols” used for make-up, litharge was transformed into laurionite and phosgenite, with pro-inflammatory properties, which prevented infections [48]. Reconstruction and analysis of the ancient remedy showed that alchemists produced soluble lead with anti-inflammatory properties, to promote healing [49]. Moreover, the toxicity of lead was reported as early as antiquity [50]. As an anti-infective, it was mostly used cutaenously. This limited the diffusion of the metal in the body, restricting its action on the local site of infection. These precautions may therefore have changed the benefit-risk balance of lead. Overall, the evidence suggests that ancient physicians knew about the inherent toxicity of toxic ingredients like metals, and handled carefully their use.
These few exemples demonstrate that the study of the history of medicine combined with modern investigation could prove the rationality of the approaches followed by these physicians. One of the periods where this scientific approach was at its peak, both in terms of the variety of actors and of the scientific approach, was the medieval Arab period (Table 1). The methodology applied by these scientists could still be relevant today and will be explained in the following section.
The Arab medieval Golden age of medicine
Medicine was certainly the most studied and the most developed science studied in the medieval Arab world. This was the Golden Age of Arab medicine with considerable scientific contributions between the 9th and 13th centuries, i.e. [51–55]. Many of the achievements of Arab-Muslim physicians were based on the legacy of Greek and Roman physicians [51,56]. This effervescence of knowledge and intelligence then spread throughout the world and significantly influenced medical theory, surgical practice and other disciplines.
Origin of the Golden Age
Several factors led to this Golden Age, including religious support. Religion could indeed easily favor, delay, or condemn medical progresses. In this context, the guidelines of the Prophet clearly encouraged such studies. The extension of the Muslim Empire during this time also brought out an exchange of ideas from India to Iran, or Spain (Figure 2). Communication routes became safer, facilitating travel and trade. Alongside these developments, Arabic language was identified as an international one, which facilitated the exchange of scholarly ideas [54]. The ancient manuscripts of greek, latin or even sansktit [57] were translated in Arabic by the most competent scholars. Another significantly contribution to the Golden Age was the establishment of a paper mills in Baghdad (for a long time the nerve center of the Arab-Muslim world [58]) to replace parchment (skin of animals) or papyrus (plant origin) by paper using linen. This enabled many people to gain access to books and develop their education [54]. The most precious texts were stored in the House of Wisdom, founded in Baghdad in 1005 by the Caliph Al Mamun [56].
There were also significant advances in chemistry, where Arab alchemists became familiarized with plants and developed different techniques such as distillation, crystallization, calcination, etc… [54]. An entire outgrowth of alchemy consisted in isolating and studying a broad spectrum of natural sources, minerals, and compounds, to discover a ‘magic elixir’ or a medical potion that would preserve people from all fatal diseases.
Likewise, in microbiology, plague and leprosy were considered as infective and contagious diseases. For example, Islamic practitioners introduced the concept of quarantining (XIth century) as a form of disease control. Hygienic methods were also implemented at the same time, in the form of proper sterilization, putting in place practices such as the use of alcohol prior to surgery and skin wounds treatment [54].
Developments also occurred in pharmacology. Practitioners became acquainted with herbs, introduced new drugs such as camphor, musk, sandalwood, developed excipients, created flavoring extracts, and experimented with poisons and antidote [59,60]. The first pharmacy was established in Baghdad in 754. Four centuries later, the pharmacology science was separated from both medicine and alchemy, these disciplines becoming independent (illustrated Figure 3).
Medical education and institution
Physicians during this era followed long training courses, often being six to seven years. This education comprised an initial theoretical training in sciences, followed by clinical training in hospitals. The medical practice was even governed by a code of ethics towards patients, colleagues, and the community [61,62].
Secular hospitals were established throughout the Arab world, starting in Damascus in 706. These hospitals were well equipped. Patient monitoring, drug development and clinical trials were reported and provided key records for the development of the scientific method [63].
Famous figures of the Arab medicine age
Among the era’s many prominent figures was Zakarya Al-Razi, known in Latin as Rhazes (Figure 2, Table 1), a pharmacologist and physician of Persian origin who headed the hospital founded in Baghdad [64]. Zakarya Al-Razi devoted his life to medical research and became the founder of chemotherapy by using mineral drugs for external and internal use in cancers [64]. Since his youth, he was interested in alchemy, and later he became the first to develop metal-chemical preparations such as arsenic, copper sulfate, iron sulfate, and different forms of mercury to develop novel drugs [65]. He went on to write his famous book Al-Hawi, a 30 volumes encyclopedia that provides a general description of disorders, fevers, plagues, and skin diseases, accompanied with a complete pharmacopeia, tables of terminology, weights, and measures [65]. He was the first to administer opium as an anesthetic after testing it on animals [64].
One of the most famous Muslim scientists is Abdu Ali Ibn Husayn ibn Abdullah Ibn Sina, also known as Avicenna (Figure 2, Table 1). Of Persian origin, from Rayy, he was known as the Prince of medicine and developed a methodological approach that would be taught in European universities until the 19th century [64]. His book Al-Qanun fi al-Tibb -Canon of Medicine– represented the first pharmacopeia, including medicinal, chemical, and physical properties of more than 600 herbal drugs [66]. In addition to these accomplishments, Avicenna was the first to describe many different microbiological diseases such as anthrax and tuberculosis, and emphasized the crucial role of hygiene and dietetics [54]. He stressed the need to study new drugs before releasing them to the patients by setting rules to test their effectiveness [64].
Another interesting figure in the history of medieval science is Abu Yusuf Yaaqub Ibn Ishaq Al Kindi (Figure 2, Table 1), considered as the Father of Arab philosophy. He was interested in a many fields including metaphysics, philosophy and logic to optics and pharmacology [67]. Among his many medical writings, the most reputable and well-known might well be the medical formulary “Aqrabadhin”. This term is derived from the Greek word for ‘list’. The book details the pharmaceutical preparations derived from botanical, animals, and minerals sources, in the form of lists of medications [67,68]. He also wrote a treatise Risala fi ma’ rifat quwwat al-adwiya al-murakkaba, translated as De gradibus, and exploited mathematical rules to quantify the strength of drugs [69].
Diya al-Din Abu Muhammad Abdallah Ibn Ahmad Ibn al Baytar (Figure 2, Table 1) is another famous Arab scientist, a Muslim botanist and pharmacologist of the Medieval era. His knowledge and passion for natural sciences was inspired by his father Ahmad Ibn Abd-al Malik [70]. He studied the Galenic pharmacopeia, based on the identification of the active principles of medicinal plant extracts. His most accomplished work, entitled, Kitab al-Gami’ li-mufradat al-adwiya wa-l-agdiya translated as ‘Collection of simple remedies and food’ [69] is considered as his seminal work. It was based on Dioscorides, Galien, Al-Razi and Ibn Sina, on which he applied his own observations and corrections and mentioned simple nutrients and about 1400 drugs based on plants, animals, and mineral [70].
Drug development during the Arab Medieval ages
During the Medieval ages, Arabs significantly contributed to health and medicine. During this time, the use of drugs still relied upon scientific hypotheses introduced by the Greeks, related to ‘the theory of bodily humors’. Essentially, this theory states that humans fall sick due to imbalances of bodily humors [71]. Hippocrates (Figure 2, Table 1) stated that the human body is made up of four substances: yellow bile, black bile, water, and blood. Arab physicians agreed with this theory [72] and affirmed that physical and spiritual wellbeing was essential, and that a disease should be viewed as an opportunity to purify and balance emotional and physical feelings through rest, healthy food, breathing fresh air, and practicing proper hygiene [73]. Even if this theory was proven incorrect, the development of drugs still adhered to scientific standards, and was further framed by ethical rules [74].
Table 1: Glossary of terms and names used in the review
|
Family term |
Name |
Description |
|
Infection |
|
|
|
|
Present definition |
Development in a living being of micro-organisms that can cause injury by multiplying and possibly secreting toxins or spreading through the bloodstream |
|
|
Past definition |
Infections are described by the symptoms they cause. Their description should inform us on the nature of the infection with today standards. This usually demands a broad-ranging, interdisciplinary approach, to study the manuscript, understand the description of the disease, symptoms, the curative ingredients and infer from these descriptions a plausible causing agent, that is not without difficulties [84–86]. |
|
Professionnals |
|
|
|
|
Physician |
A person able to practise medicine, from diagnosis to treatment (except surgery) |
|
|
Alchemist |
A person who practises alchemy, the medieval forerunner of chemistry, concerned with the transformation or transmutation of matter, through distillation, crystallization… |
|
|
Pharmacian |
A person who can prepare and sell certain drugs by prescription only. They were aware of the importance of raw materials, botanic and the importance of the preparation protocol precision |
|
|
scholar |
A person who is highly educated or has an aptitude for studying. |
|
Time period |
|
|
|
|
Antiquity |
30th century BC -5th century |
|
|
Medieval time |
5-15th century |
|
|
Arab medical golden age |
9-13th century |
|
Famous figures |
|
|
|
|
Hyppocrate
|
Born around 460 BC in Cos and died in 377 BC in Larissa, was a Greek physician of the Periclean century, but also a philosopher, traditionally considered as the father of medicine |
|
|
Dioscorides |
Born between 20-40 in Anazarbe and died around 90. He was a Greek physician, pharmacologist and botanist whose work was a major source of knowledge about plant, animal or mineral based remedies during the 1500s. He is the author of the treatise ‘De materia medica’. |
|
|
Zakarya Al-Razi
|
Born in 865 in the town of Clay, died around 925 in Tehran was a Persian multidisciplinary scholar who made important contributions to medicine, alchemy and philosophy |
|
|
Abu Yusuf Yaaqub Ibn Ishaq Al Kindi
|
Born in 801 in the town of Koufan, died in 873 in Bagdad. As an encyclopedic mind, he sought to synthesize, organize and evaluate all the knowledge of his time (philosophy, mathematics, astronomy, physics, chemistry, technology…) |
|
|
Abdu Ali Ibn Husayn Ibn Abdullah Ibn Sina |
born in 980 in Ravi, died in 1037 in Hamadan, philosopher and physician, author of reference works in medicine and philosophy |
|
|
Diya al-Din Abu Muhammad Abdallah Ibn Ahmad Ibn al Baytar |
born around 1197 in the province of Malaga and died in 1248 in Damascus, an Arab-Andalusian physician, who published several works in which he brought together the pharmaceutical knowledge of his time |
|
Remedies
|
|
|
|
|
collyrae from the Bald’s Leechbook |
Make an eye salve against a wen: take equal amounts of an Allium species and garlic, take equal amounts of wine and ox gall, mix with the alliums, put in a brass vessel, let stand for nine nights, clarify well, put in a horn and at night apply to the eye with a feather [44] |
|
|
Lead-based cutaneous remedy from Al Kindi.
|
1 part of quicklime (CaO) and 1 part of litharge (PbO) are passed through a clay. They are covered with wine vinegar. Olive oil is added and also sheep fat. It is boiled together and stirred with a rod until it is mixed and almost black. The heating is renewed until the viscosity is like thick honey [49] |
The origin of drug development was founded on the accumulated knowledge from pre-Islamic periods, such as that of the Egyptian or Chinese medical systems, even if the Greek and Roman legacies still remained the basis of the developed knowledge throughout the Arab Medieval ages. Arab physicians improved this knowledge, and enhanced the concept of trials which is at the core of the scientific approach used today. Once a remedy was identified, either based on plants, animals, metals and/or minerals, its efficiency and toxicity was tested. Then, the administrated remedy could be either a simple diet, a simple drug based on plants, minerals and metals, or a mixture of one or more of the aforementioned (Figure 4) [74,75].
Ibn Sina extensively studied the nature and qualities of simple drugs in vol. 2 of the Canon. He then set rules to respect in the drug development process. This remained the basis of testing drugs [74]:
The drug must be cleaned from any foreign substances/impurities.
Drugs must be tested on two different diseases to be sure of the effects.
The mechanism of action must be evaluated.
The drug must be tested on animals and then on human, to prove their efficacy.
Altogether, the Arab physicians developed a scientific method based on experimentation, evidence-based knowledge, clinical trials, animal and/or human trials, concepts that are also found in the contemporary scientific method.
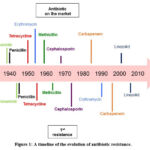 |
Figure 1: A timeline of the evolution of antibiotic resistance. |
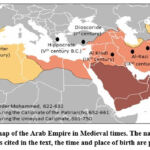 |
Figure 2: A map of the Arab Empire in Medieval times. The name of famous scientists cited in the text, the time and place of birth are provided. |
 |
Figure 3: Illustration of the preparation of a remedy. Folio from a dispersed manuscript of an Arabic translation of the Materia Medica of Dioscorides [56,82]. |
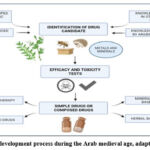 |
Figure 4: Drug development process during the Arab medieval age, adapted from [74,83]. |
Conclusions – Perspectives
Health care systems have always been deeply embedded in economic, religious, and societal beliefs, and are therefore the reflection of their perspective eras. When the era is religious, an inter-relationship between medicine and belief is widely found, through different forms, disturbing the perception and relevance of the medical and pharmacological advances of these periods. Nonetheless, these inter-relations did not prevent the rational development of medicine. All great civilizations developed a wisdom, an art of health and healing that is, empirically solid with proofs of effectiveness. It is this rationality that encourages to re-investigate ancient practices and pharmacopeias. Modern technological advances may enable to re-exploit these ancient remedies more easily [76–78].
The greatest benefit of history is its ability to integrate past and present knowledge to improve future understanding. Since ancient times, plants, insects, animals, minerals, turned out to be an exceptional source of bioactive molecules: they have already provided humans with new first-class remedies [79]. In comparison to isolated ingredients, these pharmacopeias provide remedies with synergistic combination of action. These remedies have enhanced therapeutic effects through the combination of ingredients that would be of little medicinal interest if isolated. These studies are nevertheless complex and require the establishment of important interdisciplinary networks, including history, biology, chemistry and pharmacology. Recognition of these networks and the valorization of their added value remain a challenge.
The Arabic Golden Age was an important period in the history of ancient medicines and paved the foundations for a modern scientific approach. Their knowledge largely inspired Western medicine from the Middle Ages to the Renaissance. The numerous manuscripts found allowed to collect a large amount of information on medical practices and pharmacopeias, and to follow these practices in time and space. By focusing mainly on remedies preserved over a wide geographical or temporal scale, ingredients of interest with the highest potential may be selected.
This approach is well suited for the search of antibacterial solutions, in the context of bacterial resistance to antibiotics. Infections were a daily concern in the Middle Ages, and the solutions proposed were numerous: we thus have access to a vast repertoire of potential solutions. These ancient pharmacopeias contain a vast array of information on both innovative molecules and synergistic strategies making it more difficult for bacteria to develop resistance, while potentially reducing the impact on the surrounding microbiota (bactericidal molecules taken individually being less deleterious). Thus, history holds a vast repertoire of remedies that might lead to medical innovation. In addition, some ancient remedies preserved throughout history, are still utilized today in the traditional Arab pharmacopeia. If their efficacy could be validated historically and by using today’s scientific methodology, they could even be adopted in the context of integrated healthcare.
Medical systems are constantly evolving. Novel medical systems are introduced when an old is challenged. This evolution often results in an interweaving of innovations and old practices, although the integration of ancient practices usually comes with parsimony or defiance [80]. This has always been the case, and is still true today, a time when we are witnessing a crisis in health care related to inadequate delivery and adaptation to changing patient expectations. This crisis amplifies the growing demand for complementary and alternative medicines, which have their origins in ancient and/or traditional practices. This is reflected in the growing number of patients (over 70% according to the WHO) who are already turning to these practices. Despite the complementarity between modern and traditional medicines, it is their connection that seems to be problematic today. The differences in the way health and pathology are defined, studied and perceived, could also be at the source of the difficulties in uniting them. Therefore, it is imperative to study the cultures and societies that laid the foundations of ancient medicine [81]. Characterizing the scientific approach by which medicine and pharmacopeias were developed, and understanding how the different health systems have intertwined with each other over time could help to rationalize the debate, and ultimately, why not, lay the foundations for a modern conception of a common medicine ?
Acknowledgments
We would like to thank Cody Bowens for critical reading of the manuscript and Mutale Joan Chanda for her diligent proofreading of the manuscript.
Conflict of Interest
The authors declare no conflict of interest
Funding Sources
This project was financially supported by the French Ministry of Europe and Foreign Affairs, Ministry of Higher Education, Research and Innovation and the French Institute of Rabat (PHC TOUBKAL 2019, Grant Number: 41520SE; PHC MAGHREB 2022 Grant No 47455NH; by the University of Strasbourg (projet Interdisciplinaire – Emergence) Grant Number CF/PN/CB/N°2017-974-3, and by the program METALLO-MIX of CNRS – Grant Number 21887. B. Abdallah was financed by the Mascir Foundation (Rabat), and by the PHC TOUBKAL.
References
- Pan S-Y, Litscher G, Gao S-H, Zhou S-F, Yu Z-L, Chen H-Q, et al. 2014. Historical Perspective of Traditional Indigenous Medical Practices: The Current Renaissance and Conservation of Herbal Resources. Evid Based Complement Alternat Med 2014: 525340.
- Porras G, Chassagne F, Lyles JT, Marquez L, Dettweiler M, Salam AM, et al. 2021. Ethnobotany and the Role of Plant Natural Products in Antibiotic Drug Discovery. Chem Rev 121: 3495–3560.
- Krishnaprabu DS. 2020. Therapeutic potential of medicinal plants: A review. J Pharmacogn Phytochem 9: 2228–2233.
- Perumal Samy R, Gopalakrishnakone P. 2010. Therapeutic Potential of Plants as Anti-microbials for Drug Discovery. Evid Based Complement Alternat Med 7: 283–294.
- Dal Cero M, Saller R, Weckerle CS. 2014. The use of the local flora in Switzerland: A comparison of past and recent medicinal plant knowledge. Journal of Ethnopharmacology 151: 253–264.
- Lardos A, Heinrich M. 2013. Continuity and change in medicinal plant use: The example of monasteries on Cyprus and historical iatrosophia texts. Journal of Ethnopharmacology 150: 202–214.
- Staub PO, Casu L, Leonti M. 2016. Back to the roots: A quantitative survey of herbal drugs in Dioscorides’ De Materia Medica (ex Matthioli, 1568). Phytomedicine 23: 1043–1052.
- Touwaide A, Appetiti E. 2013. Knowledge of Eastern materia medica (Indian and Chinese) in pre-modern Mediterranean medical traditions: A study in comparative historical ethnopharmacology. Journal of Ethnopharmacology 148: 361–378.
- Harrison F, Connelly E. 2019. Could Medieval Medicine Help the Fight Against Antimicrobial Resistance? De Gruyter.
- Caiazzo I. 2019. Le mélange et la complexion chez les médecins du XIIe siècle. De l’homme, de la nature et du monde. 225–240.
- Zhou X, Seto SW, Chang D, Kiat H, Razmovski-Naumovski V, Chan K, et al. 2016. Synergistic Effects of Chinese Herbal Medicine: A Comprehensive Review of Methodology and Current Research. Front Pharmacol 7: 201.
- Yarnell E. 2015. Synergy in Herbal Medicines. Journal of Restorative Medicine 4: 60.
- Christie VM. 1991. A dialogue between practitioners of alternative (traditional) medicine and modern (western) medicine in Norway. Social Science & Medicine 32: 549–552.
- Drakulich A. 2018. Challenges Faced When Implementing an Integrative Care Model. Available from https://www.practicalpainmanagement.com/meeting-summary/challenges-faced-when-implementing-integrative-care-model. Accessed Jul. 27, 2022.
- Inserm pressroom. 2020. Artemisia miracle plant, really? Available from https://presse.inserm.fr/en/artemisia-miracle-plant-really/40111/. Accessed Jul. 27, 2022.
- Lampiao F, Chisaka J, Clements C. 2019. Communication Between Traditional Medical Practitioners and Western Medical Professionals. Frontiers in Sociology 4.
- Roth AD. 2016. A Dialogue on Traditional Medicine: East Meets West. China Media Research 12: 58–92.
- Gaynes R. 2017. The Discovery of Penicillin—New Insights After More Than 75 Years of Clinical Use. Emerg Infect Dis 23: 849–853.
- Ligon BL. 2004. Penicillin: its discovery and early development. Seminars in Pediatric Infectious Diseases 15: 52–57.
- Aslam B, Khurshid M, Arshad MI, Muzammil S, Rasool M, Yasmeen N, et al. 2021. Antibiotic Resistance: One Health One World Outlook. Front Cell Infect Microbiol 11: 771510.
- Llor C, Bjerrum L. 2014. Antimicrobial resistance: risk associated with antibiotic overuse and initiatives to reduce the problem. Ther Adv Drug Saf 5: 229–241.
- McEwen SA, Collignon PJ. 2018. Antimicrobial Resistance: a One Health Perspective. Microbiol Spectr 6.
- Barber M, Rozwadowska-Dowzenko M. 1948. Infection by penicillin-resistant staphylococci. Lancet 2: 641–644.
- Lobanovska M, Pilla G. 2017. Penicillin’s Discovery and Antibiotic Resistance: Lessons for the Future? Yale J Biol Med 90: 135–145.
- Damrosch DS. 1946. Chemoprophylaxis and sulfonamide resistant streptococci. J Am Med Assoc 130: 124–128.
- Hamburger M, Mattman LH. 1946. Susceptibility to sulfadiazine of hemolytic streptococci recovered in Army camps. Am J Med 1: 23–27.
- Sköld O. 2000. Sulfonamide resistance: mechanisms and trends. Drug Resist Updat 3: 155–160.
- Crofton J, Mitchison DA. 1948. Streptomycin resistance in pulmonary tuberculosis. Br Med J 2: 1009–1015.
- Watanabe T. 1963. Infective heredity of multiple drug resistance in bacteria. Bacteriol Rev 27: 87–115.
- Levy SB, Marshall B. 2004. Antibacterial resistance worldwide: causes, challenges and responses. Nat Med 10: S122–S129.
- Murray CJ, Ikuta KS, Sharara F, Swetschinski L, Aguilar GR, Gray A, et al. 2022. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. The Lancet 399: 629–655.
- Michael CA, Dominey-Howes D, Labbate M. 2014. The Antimicrobial Resistance Crisis: Causes, Consequences, and Management. Front Public Health 2: 145.
- Al-Snafi AE. 2015. Therapeutic properties of the medicinal plants: a review of their antibacterial activity (Part 1). International Journal of Pharmacy Review & Research 5: 328–337.
- Bassett EJ, Keith MS, Armelagos GJ, Martin DL, Villanueva AR. 1980. Tetracycline-labeled human bone from ancient Sudanese Nubia (A.D. 350). Science 209: 1532–1534.
- Behroozian S, Svensson SL, Davies J. 2016. Kisameet Clay Exhibits Potent Antibacterial Activity against the ESKAPE Pathogens. mBio 7: e01842-15.
- Brennessel B, Drout MDC, Gravel R. 2005. A reassessment of the efficacy of Anglo-Saxon medicine. Anglo-Saxon England 34: 183–195.
- Fratini F, Cilia G, Mancini S, Felicioli A. 2016. Royal Jelly: An ancient remedy with remarkable antibacterial properties. Microbiol Res 192: 130–141.
- Gabbay GB and J. 2009. Copper, An Ancient Remedy Returning to Fight Microbial, Fungal and Viral Infections. Available from https://www.eurekaselect.com/93409/article. Accessed Oct. 26, 2020.
- Photos-Jones E, Keane C, Jones AX, Stamatakis M, Robertson P, Hall AJ, et al. 2015. Testing Dioscorides’ medicinal clays for their antibacterial properties: the case of Samian Earth. Journal of Archaeological Science 57: 257–267.
- Wagner CS, De Gezelle J, Robertson M, Robertson K, Wilson M, Komarnytsky S. 2017. Antibacterial activity of medicinal plants from The Physicians of Myddvai, a 14th century Welsh medical manuscript. J Ethnopharmacol 203: 171–181.
- Anonye BO, Nweke V, Furner-Pardoe J, Gabrilska R, Rafiq A, Ukachukwu F, et al. 2020. The safety profile of Bald’s eyesalve for the treatment of bacterial infections. Sci Rep 10: 17513.
- Fuchs AL, Weaver AJ, Tripet BP, Ammons MCB, Teintze M, Copié V. 2018. Characterization of the antibacterial activity of Bald’s eyesalve against drug resistant Staphylococcus aureus and Pseudomonas aeruginosa. PLoS One 13: e0208108.
- Furner-Pardoe J, Anonye BO, Cain R, Moat J, Ortori CA, Lee C, et al. 2020. Anti-biofilm efficacy of a medieval treatment for bacterial infection requires the combination of multiple ingredients. Sci Rep 10: 12687.
- Harrison F, Roberts AEL, Gabrilska R, Rumbaugh KP, Lee C, Diggle SP. 2015. A 1,000-Year-Old Antimicrobial Remedy with Antistaphylococcal Activity. mBio 6.
- Connelly E, Del Genio CI, Harrison F. 2020. Data Mining a Medieval Medical Text Reveals Patterns in Ingredient Choice That Reflect Biological Activity against Infectious Agents. mBio 11.
- Braud A, Dolques X, Fechter P, Lachiche N, Ber FL, Pitchon V. 2021. Analyzing the composition of remedies in ancient pharmacopeias with FCA, p 9. . Strasbourg.
- Pitchon V, Aubert E, Vonthron C, Fechter P. 2022. Chapter 14 – How history can help present research of new antimicrobial strategies: the case of cutaneous infections’ remedies containing metals from the Middle Age Arabic pharmacopeia, pp 459–478, In Chassagne F (ed.), , Medicinal Plants as Anti-Infectives. . Academic Press.
- Tapsoba I, Arbault S, Walter P, Amatore C. 2010. Finding Out Egyptian Gods’ Secret Using Analytical Chemistry: Biomedical Properties of Egyptian Black Makeup Revealed by Amperometry at Single Cells. Anal. Chem. 82: 457–460.
- Abdallah B, Seguin C, Aubert E, Ait BenHassou H, Sbabou L, Choulier L, et al. 2022. Past mastering of metal transformation enabled physicians to increase their therapeutic potential. Journal of Trace Elements in Medicine and Biology 71: 126926.
- Lanoë C. 2002. La céruse dans la fabrication des cosmétiques sous l’Ancien Régime (XVIe-XVIIIe siècles). Techniques & Culture. Revue semestrielle d’anthropologie des techniques.
- Ahmed S, Hasan M. 2016. Muslim heritage in medicine: A concise review on Greco-Arabic contribution. Journal of Pharmacognosy and Phytochemistry 5: 273–283.
- Anawati GC 1905-1994. 1974. Les Médicaments De L’Oeil Chez Hunayn Ibn Ishãq. Arabica 21: 232.
- Bachour HT. 2002. The Contributions Of Arabs Physicians in Dermatology. JISHIM 2: 43–45.
- Falagas ME, Zarkadoulia EA, Samonis G. 2006. Arab science in the golden age (750–1258 C.E.) and today. The FASEB Journal 20: 1581–1586.
- Théodoridès J. 1955. La Parasitologie et la Zoologie dans l’œuvre d’Avenzoar. Revue d’histoire des sciences 8: 137–145.
- Hajar R. 2013. The Air of History Part III: The Golden Age in Arab Islamic Medicine An Introduction. Heart Views 14: 43–46.
- Kahl O. 2019. On the Transmission of Indian Medical Texts to the Arabs in the Early Middle Ages. Arabica 66: 82–97.
- Hannawi AA. 2012. The Role of the Arabs in the Introduction of Paper into Europe. MELA Notes 14–29.
- Bos G, Käs F, eds. 2021. Ibn al-Jazzār’s Zād al-musāfir wa-qūt al-ḥāḍir. Provisions for the Traveller and Nourishment for the Sedentary: Book I&II. Brill.
- Hooper D, Field H. 1937. Useful plants and drugs of Iran and Iraq / by David Hooper. With notes by Henry Field. Chicago,.
- Haddad FS. 1993. Arab contribution to medicine. Bull Soc Liban Hist Med 21–33.
- Pitchon V. 2016. To feed and to care according to the dietetics orinciples: preparation and distribution of food and medicine in an Arabic hospital during the medieval period. Food and History 14: 13–33.
- Kahl O. 2004. Fragments of an anonymous old dispensatory in ar-Razi’s Kitab al-Ḥawi. Journal of Semitic studies 49: 289.
- Masic I, Skrbo A, Naser N, Tandir S, Zunic L, Medjedovic S, et al. 2017. Contribution of Arabic Medicine and Pharmacy to the Development of Health Care Protection in Bosnia and Herzegovina – the First Part. Med Arch 71: 364–372.
- Behbehani AM. 1984. Rhazes: The Original Portrayer of Smallpox. JAMA 252: 3156.
- Colgan R. 2012. Advice to the Healer: On the Art of Caring. 2nd ed. 2013 edition. Springer, New York.
- Prioreschi P. 2002. Al-Kindi, A Precursor Of The Scientific Revolution. JISHIM 2: 17–20.
- Erdemi̇r AD. 2018. Abu Yusuf Yaqub ibn Ishaq ibn al-Sabbah al-Kindi (Alkindi, Alchindi)’nin (803-873) İslam Tıp Tarihindeki Yeri ve Bazı Orijinal Sonuçlar. Turkiye Klinikleri J Med Ethics 26: 23–34.
- Ahmed, O, Moulay, S. 2004. L’apport scientifique arabe à travers les grandes figures de l’époque classique. Unesco.
- Cabo Gonzalez AM, Lanly C. 1997. Ibn al-Baytār et ses apports à la botanique et à la pharmacologie dans le Kitāb al-Ğāmï. Médiévales 16: 23–39.
- Kalachanis K, Michailidis IE. 2015. The Hippocratic View on Humors and Human Temperament. European Journal of Social Behaviour 2: 1–5.
- Ormos I. 1987. The theory of humours in Islam (Avicenna). Quaderni di Studi Arabi 5/6: 601–607.
- AlRawi SN, Fetters MD. 2019. Traditional Arabic and Islamic Medicine Primary Methods in Applied Therapy. GJHS 11: 73.
- Saad B, Said O. 2011. Greco arb and islamic herbal medicine. Wiley.
- Saad B, JadAllah R, Daraghmeh H, Said O. 2009. Medicine and methods of therapy in teh arab and islamic world. Available from https://www.aaup.edu/publication/harbi.darghmeh/article/medicines-and-methods-therapy-arab-and-islamic-world. Accessed Jul. 26, 2022.
- Harvey AL, Edrada-Ebel R, Quinn RJ. 2015. The re-emergence of natural products for drug discovery in the genomics era. Nat Rev Drug Discov 14: 111–129.
- Qaraghuli MMA, Alzahrani AR, Niwasabutra K, Obeid MA, Ferro VA. 2017. Where Traditional Drug Discovery Meets Modern Technology in the Quest for New Drugs. Annals of Pharmacology and Pharmaceutics 2: 1061.
- Salam AM, Quave CL. 2018. Opportunities for plant natural products in infection control. Curr. Opin. Microbiol. 45: 189–194.
- Veeresham C. 2012. Natural products derived from plants as a source of drugs. J Adv Pharm Technol Res 3: 200–201.
- Petri RP, Delgado RE, McConnel K. 2015. Historical and Cultural Perspectives on Integrative Medicine | Medical Acupuncture. Medical Acupuncture 27: 309–317.
- Green MH. 2009. Integrative Medicine: Incorporating Medicine and Health into the Canon of Medieval European History. History Compass 7: 1218–1245.
- Dioscorides Pedanius, Osbaldeston TA, Wood RPA. 2000. De materia medica: being an herbal with many other medicinal materials: written in Greek in the first century of the common era: a new indexed version in modern English. IBIDIS, Johannesburg.
- Ahmed S, Siddiqui MUA, Mallick IA, Hasan MM. 2021. Zootherapeutics (Animal-based remedies) for urolithiasis: History, current scenario and future dimensions. J Pharmacogn Phytochem 10: 08–11.
- Crawford S, Lee C. 2014. Social dimensions of medieval disease and disability / edited by Sally Crawford, Christina Lee. Archaeopress, Oxford, England.
- Müller R, Roberts CA, Brown TA. 2015. Complications in the study of ancient tuberculosis: non-specificity of IS6110 PCRs. STAR: Science & Technology of Archaeological Research 1: 1–8.
- Tu Y. 2011. The discovery of artemisinin (qinghaosu) and gifts from Chinese medicine. Nat Med 17: 1217–1220.







