Manuscript accepted on :29-06-2022
Published online on: 01-07-2022
Plagiarism Check: Yes
Reviewed by: Dr.Nishu Raina, Dr. Randa Salah
Second Review by: Dr. Ahmed Salah
Final Approval by: Dr. H Fa Poon
Department of Basic Medical Sciences, College of Medicine, Prince Sattam bin Abdulaziz University, Al-Kharj 11942, Saudi Arabia
Corresponding Author E-mail: dr.shahid90@yahoo.com
DOI : https://dx.doi.org/10.13005/bpj/2399
Abstract
Testis-determining factor (TDF) is an alternative term for the sex-determining region (SRY) gene found on the Y chromosome. SRY gene mutations can cause a wide range of sex development issues. The single-exon SRY gene is a short and intronless sex-determining gene with a DNA-binding high mobility group (HMG) box that is highly conserved. We performed cytogenetic analysis on one patient with Turner syndrome having a 45,X/46,XY chromosomal composition. Further, we used polymerase chain reaction, single-stranded conformational polymorphism, and automated DNA sequencing to detect a substitution of C→A (missense mutation) at codon 139, which led to an amino acid shift from Proline to Glutamine (P139Q) outside but downstream of the HMG box in the SRY gene. No further alterations in the SRY gene were discovered in the patient. The absence of one X chromosome in 88% of the patient’s cells might have resulted in a wide variety of phenotypic complications.
Keywords
Mosaicism; Primary amenorrhea; SRY gene; Turner syndrome
Download this article as:| Copy the following to cite this article: Shahid M. Mutation Analysis of the SRY Gene in a Patient with Turner Syndrome. Biomed Pharmacol J 2022;15(2). |
| Copy the following to cite this URL: Shahid M. Mutation Analysis of the SRY Gene in a Patient with Turner Syndrome. Biomed Pharmacol J 2022;15(2). Available from: https://bit.ly/3adLQJE |
Introduction
Turner syndrome (TS) is a common genetic condition mainly affecting women. It is triggered by a defective, complete, or moderately deleted X chromosome1. TS can cause various medical and developmental problems, such as short height, ovarian failure, infertility, cardiac anomalies, gonadal dysgenesis, and dysmorphic characteristics such as neck webbing2. Most cases have a 45,X chromosomal constitution, while the others have either fundamentally defective sex chromosome or a mosaic karyotype3. Patients with TS having a mosaic 45,X/46,XY chromosomal makeup and mutated SRY gene may have an increased risk of developing gonadoblastoma4. A majority of female patients with TS are infertile because of gonadal dysgenesis and a streak ovary having no eggs or follicular derivatives5,6. One of the essential genes in sex determination is the Y chromosomespecific SRY gene3. It is a 204-aminoacid protein that codes a testis-specific transcription factor important in sex determination and is found on the p-arm of the Y chromosome7. SRY is a short and intronless gene containing a conserved DNA-binding high mobility group (HMG) box, indicating that it controls gene expression. In humans, sex is determined by a single-exon SRY gene. SRY gene mutations cause testicular failure and abnormal sex determination with different impacts on an individual’s phenotype and genotype8. In mammals, the SRY gene is required for testis development and male sex determination. SRY gene alterations have been found to be responsible for about 15% of XY sex reversal cases9. To our knowledge, more than 65 alterations have been detected in the open reading frame (ORF) region of the SRY gene. A majority of these have been found within the HMG box, demonstrating the importance of this domain. Several mutations have been found outside the HMG box in the 5′ and 3′ regions upstream and downstream10, (Table1)11. We presented a substitution in a patient with TS having 45,X (88%)/46,XY (12%) mosaic chromosomal makeup. To our knowledge, no mutation at this position has ever been reported in the literature.
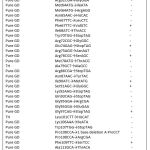 |
Table 1: SRY gene mutations that have been discovered so far11 |
Participants and Methods
All the control participants and patient provided informed consent to participate in this investigation. The study was approved by the Ethics Committee and Biosafety Committee at both the hospital and the university.
Patient
A 26-year-old woman visited the hospital with a complaint of primary amenorrhea. A height of 128 cm was discovered on clinical and physical testing, along with multiple Turner stigmata (i.e., webbed neck, broad shield-like chest with evenly spaced nipples, presence of Mullerian structures, high arched palate, cubitus valgus, sexual infantilism at puberty, high blood pressure, and glucose intolerance). This patient also had scoliosis, nail dysplasia, and ear defects. In streak gonads, the histological examinations showed white fibrous stromal tissue. The endocrinological examinations revealed hypogonadotropic hypogonadism and normal levels of testosterone and androstenedione. The hair on the axilla and pubis was few. The patient’s blood karyotype was 45,X/46,XY (88% and 12% respectively) according to the cytogenetic examination in the peripheral blood.
Cytogenetic and molecular genetic analyses
G-banding was used to analyze metaphase spreads in the patient’s peripheral blood. Proteinase K digestion, phenol-chloroform isolation, and precipitation using isopropanol with cold 3M sodium acetate (pH 5.2) were used to isolate genomic DNA from the peripheral-blood leukocytes from the patient and normal male controls. The genomic DNA quality and quantity were calculated using the gel electrophoresis technique after vacuum-drying the DNA samples and dissolving them in Tris-EDTA.
PCR analysis
Overlapping primers were used to examine the whole SRY exon; the required primers, which aided in identifying this mutation, were stated. The following two sets of primers were employed in polymerase chain reaction (PCR) to magnify the segments of 254 and 351 bp from the ORF region of the SRY gene: F1 5ʼ-CATGAACGCATTCATCGTGTGGTC-3ʼ, R15ʼ-CTGCGGGAAGCAACTGCAATTCTT-3ʼ, F2, 5ʼ-CAGTGTGAAACGGGAGAAAACAGT-3ʼ, and R2, 5ʼ-GTTGTCCAGTTGCACTTCGCTGCA-3ʼ. Further, the primers F1 5ʼ-TACTCCCCTGCCCTCAACAA-3ʼ and R1, 5 ʼ-CATCGCTATCTGAGCAGCGC-3ʼ were used to magnify exon 5 of the p53 gene as a control. PCR amplification was carried out in a 25-µL mixture having 10 mmol/L Tris-HCl (pH 8.4), 50 mmol/L KCl, 1.5 mmol/L MgCl2, 200 µmol/L each of deoxynucleotide triphosphates, 5 pmol primers, and 100–500ŋg patient’s DNA with Taq DNA polymerase. The following PCR cycle settings were used: a 4-min denaturation at 95°C, followed by 30 s at 55°C and 30 s at 72°C, and a final extension step at 72°C for 5 min. Each PCR involved both negative and positive controls. On an ultraviolet transilluminator, ethidium bromide was used to run PCR on 2% agarose gels. A 100-bp ladder (as size standard) was used on all agarose gels.
Single-stranded conformational polymorphism
After 15 more PCR cycles, the PCR products were labeled with (α-p32) deoxycytidine triphosphate and run on a 6% non-denaturing polyacrylamide gel with 5% glycerol. The electrophoresis was performed overnight at 200 V and 17 ± 1oC. The dried gel was exposed to an x-ray film at –70°C for 48 hrs. The dried gel was subjected to 48-hrsX-ray film exposure at –70°C.
Automated DNA sequencing
Ammonium acetate ethanol precipitation techniques were used to purify mutant and control PCR products. An ABI Prism 310 automated sequencer was used to perform automated DNA sequencing of PCR products. The purified PCR products were cycle sequenced using a GeneAmp PCR 9700 with BigDye Terminator Sequencing Ready Reaction Mix and AmpliTaq DNA Polymerase FS. The PCR settings were 96°C for 10s, 56°C for 5s, and 60°C for 4 min for 25 cycles. The extension yields were cleaned by an ethanol/sodium acetate precipitation method to remove any unincorporated dye-labeled terminators after cycle sequencing. The samples were heat-denatured, freeze-dried, and placed on a Prism 310 sequencer after adding the template suppressor reagent. Sequencing analysis software 3.4.1 was used to examine the sequences on a Mac OS 9.1 computer.
Results
We performed cytogenetic analysis on metaphase spreads from the cultured peripheral blood cells of the patient. Mosaic chromosomal makeup 45,X/46,XY (88% and 12%, respectively) was found in the patient with TS. The estradiol, LH, and FSH levels were abnormal, whereas the testosterone and androstenedione levels were normal in the patient. Based on the aforementioned findings, we designed a PCR to amplify a particular area of the SRY gene. In the SSCP experiment, the PCR product migrated abnormally. We identified a mutation in DNA from the patient’s blood using direct DNA automated sequencing of the SRY gene. This alteration was a missense mutation that caused an amino acid change from Proline to Glutamine (P139Q) immediately outside but downstream of the HMG box in the SRY gene (Figure1). SRY sequencing of 25 unrelated normal men revealed no mutations, ruling out the possibility of a polymorphism. These findings indicated that the aforementioned variations were mutations rather than ordinary polymorphisms.
 |
Figure 1: HMG box partial upstream and downstream sequences, as well as the mutation’s site (Affected residue, amino acid in the arrow)11. |
Discussion
The SRY gene, which is found on the Y chromosome, is shown to be essential for appropriate male sex determination12. Many investigations of human intersex disorders support the designation of SRY as the testis-determining factor9,11,13-15. The timing and expression of this gene are extremely controlled, facilitating testis development in the growing embryo16. A mosaic 45,X/46,XY chromosomal make-up with a mutant SRY gene may enhance the incidence of gonadoblastoma in TS patients. Numerous medical and developmental issues, including low stature, ovarian failure, infertility, heart malformations, gonadal dysgenesis, and dysmorphic features including neck webbing, may be brought on by TS2. The Y chromosome-specific SRY gene is one of the crucial genes in sex determination. In the present study, the patient had 45,X/46,XY chromosomal makeup (88% and 12%, respectively) with multiple Turner stigmata. In this patient, the levels of estradiol, LH, and FSH were abnormal, while the levels of testosterone and androstenedione were normal. We identified a change in DNA from the patient’s blood sample. This mutation resulted in a missense alteration in the SRY gene, causing an amino acid change from Proline to Glutamine (P139Q) just outside but downstream of the HMG box. The patient’s male relatives declined to have their DNA tested, even though some of them were already fathers to healthy children. This mutation might induce a change in a non-functional protein, as evident from the failure to produce male sex structures. A complex mix of genetic and nongenetic elements determines early embryonic sexual differentiation17. Sufficient evidence shows that SRY is important for determining sex, and altered gene expression has been linked to gonadal dysgenesis3. Few studies have reported patients with a clinical presentation similar to TS, who have a large segment of cells with the imitative Y chromosome. A hormonal malfunction was observed during male sexual differentiation despite the existence of a structurally defective SRY gene17. In the present case, the alteration in the SRY gene and the occurrence of the overriding 45,X cell line together might have led to a cause-effect connection. A small percentage of 45,X cell line appeared to be adequate to block the male sex-determining activity of the SRY gene18-20. This showed that neither aberrant sex chromosomal pairing nor deletion of the SRY region of the Y chromosome led to the problem. In the present case, the nondisjunction loss of the Y chromosome following normal disomic fertilization might have resulted in the mosaic karyotype. Although the Y chromosome appeared to be normal, changes in other genes on the chromosome, which were essential for chromosomal reliability, might have eventually caused its loss21. The SRY protein belongs to the SOX transcription factor family. It is defined as an HMG domain with DNA-binding and bending characteristics, the capacity to mediate protein–protein interactions and the presence of nuclear import signals22. We described a case of a female patient with a codon change in the SRY gene (substitution of C→A) and a missense mutation that caused an amino acid change from Proline to Glutamine (P139Q) directly outside but downstream of the HMG box. The mutation facilitated protein–protein interactions and comprised nuclear import signals. It was conceivable that the mutant SRY protein could not reach the nucleus and damaged the nuclear localization signal required for male gene expression. This alteration might have resulted in an electrostatic and hydrophobic connection between DNA’s phosphate and sugars. This caused changes in the main groove’s particular orientation and binding to DNA bases22. The interactions of SRY with DNA might have been completely or partially inhibited by this alteration23. A mutant SRY protein was previously identified in patients with TS having a mosaic 45,X/46,XY karyotype. This anomaly increased the functional relevance of the alteration, which probably resulted in a protein that had lost some of its ability to stabilize23. Dysgenetic gonads, perhaps caused by SRY mutations, often lead to gonadoblastoma. However, the molecular cause of gonadoblastoma is yet unknown. During development, some gonads do not mature into testes, resulting in a girl with delayed puberty and amenorrhea24. A proto-oncogene implicated in the genesis of malignant tumors is considered to be found in the GBY gene in the Yq region24. TSPY is normally expressed in adult testis spermatogonia and is thought to be involved in mitotic proliferation25. The control of the major genital ridge by the 45, X cell line during initial embryonic phases may be responsible for the appearance of streak gonads. This is supported by the fact that the mutations in oncogenes, tumor suppressor genes, and DNA repair genes accumulate with age, leading to tumor formation in the streak gonads26. Many people with SRY gene abnormalities do not acquire secondary sexual characteristics when they reach puberty. Previous studies have shown that the entire Y chromosome is associated with an elevated risk of gonadoblastoma in patients with TS. Most of the SRY gene alterations discovered so far are inside the conserved motif, resulting in changes in DNA-binding/bending activity and, subsequently, individuals with 46,XY chromosomal makeup27. To the best of our knowledge, more than 10 mutations outside the HMG box have been discovered so far, and each has a diverse influence on the patients’ phenotype. The areas beyond the HMG box are thought to be needed to stabilize protein binding and produce specificity by helping in the differentiation of protein–protein interactions19. The capacity of SRY protein to bind to DNA and bend has been shown to be critical for testis development11. The findings of this study, particularly the missense mutation downstream of the HMG box, highlighted the functional role of the SRY gene in the expression and activity of the patient.
Conclusion
The current findings, particularly the missense mutation outside but downstream of the HMG box in the SRY gene, support its functional significance in this patient’s expression and activity. As a result, it is concluded that patients with TS must be evaluated using traditional cytogenetic, FISH, and molecular genetics techniques to determine the presence of the SRY gene as well as GBY region.
Acknowledgments
We appreciate the patient’s cooperation, as well as her family members and other research participants. Doctors and staff members from the Department of Obstetrics and Gynecology, as well as the Male Family Welfare Centre at Maulana Azad Medical College and Lok Nayak Hospitals in New Delhi, India, are also thanked. M.S. wishes to express her gratitude to the College of Medicine and Deanship of Scientific Research, Prince Sattam bin Abdulaziz University, Alkharj, Saudi Arabia, for their continued support in performing this research.
Conflict of Interest
There are no conflicting interests declared by the author.
Funding Sources
There are no funding source.
References
- Gimelli G, Gimelli S, Dimasi N, Bocciardi R, Di Battista E, Pramparo T and Zuffardi O. Identification and molecular modelling of a novel familialmutation in the SRY gene implicated in the pure gonadal dysgenesis.Eur. J. Hum. Genet., 2007; 15:76-80.
CrossRef - Jones K.L. Smith’s recognizable patterns of human malformation. 5th ed.Philadelphia: W. B. Saunders Co.,1997; 81–87
- Sinclair A. H, Beerta P, Palmer M. S, Hawkins J. R, Griffiths B. L, Goodfellow P. N and Fellous M. A gene from the human sex-determining region encodes aprotein with homology to a conserved DNA-binding motif. Nature., 1990;346:240-244.
CrossRef - Scully R. E. Gonadoblastoma: a review of 74 cases. Cancer., 1970;25:1340-1356.
CrossRef - Sokol R. Z. Infertility in men with cystic fibrosis. Curr.Opin.Pulm.Med., 2001; 7(6): 421-426.
CrossRef - Folsom L. J and Fuqua J. S. Reproductive issues in women with Turnersyndrome. Endocrinol.Metab.Clin. North. Am., 2015; 44(4): 723-737.
CrossRef - Koopman P, Gubbay J, Vivian N, Goodfellow P and Lovell-Badge R. Maledevelopment of chromosomally female mice transgenic for Sry. Nature.,1991; 351:117-21.
CrossRef - Harley V. R, Jackson D. I, Hextall P. J, Hawkins J. R, Berkovitz G. D, Sockanathan S,Lovell-Badge R and Goodfellow P. N. DNA binding activity of recombinant SRY from normal males and XY females. Science., 1992; 255:453-456.
CrossRef - Behlke M. A, Began J. S and Page D. C. Evidence that the SRY protein encodedby a single exon on the human Y-chromosome. Genomics., 1993;17:736-739.
CrossRef - Stenson P.D, Ball E.V, Mort M.E, Phillips A.D, Shiel J.A, Thomas N.S, Abeysinghe S.S, Krawczak M. and Cooper D.N. Human Gene Mutation Database (HGMD): 2003 update. Human Mutation., 2003; 6:577-581.
CrossRef - Shahid M, Dhillion V.S, Jain N, Hedau S, Diwakar S, Sachdeva P, Batra S, Das B.C, and Husain S.A. Two new novel point mutations localized upstream and downstream of the HMG box region of the SRY gene in three Indian 46,XY females with sex reversal and gonadal tumour formation. Molecular Human Reproduction., 2004; 7:521-526.
CrossRef - Affara N. A, Chalmers I. J and Ferguson-Smith M. A. Analysis of theSRY gene in 22 sex-reversed XY females identifies four new pointmutations in the conserved DNA binding domain. Hum. Mol. Genet., 1993;2: 785–789.
CrossRef - Assumpcao J. G, Benedetti C. E, Maciel-Guerra A. T, Guerra G, BaptistaM. T. M, Scolfaro M. R and de Mello M. P. Novel mutations affectingSRY DNA-binding activity: the HMG box N65H associated with 46, XYpure gonadal dysgenesis and the familial non-HMG box R30I associatedwith variable phenotype. J. Mol. Med., 2002; 80,782–790.
CrossRef - Bilbao J. R, Loridan L and Castano L. A novel postzygotic nonsensemutation in SRY in familial XY gonadal dysgenesis. Hum. Genet., 1996; 97: 537–539.
CrossRef - Brown S, Yu C. C, Lanzano P, Heller D, Thomas L, Warburton D, Kitajewski Jand Stadtmauer L. A de novo mutation (Gln2Stop) at the 50 end ofthe SRY gene leads to sex reversal with partial ovarian function. Am. J. Hum.Genet., 1998; 62: 189–192.
CrossRef - Cameron F. J and Sinclair A. H. Mutations in SRY, SOX9: testis determining gene.Hum.Mutat., 1997; 9:388-395.
CrossRef - McElreavey K and Fellous M. Sex determination and the Y chromosome.Am J Med. Genet., 1999; 89:176–185.
CrossRef - Canto P, De La Chesnaye E, Lopez M, Cervantes A, Chavez B, Vilchis F,Reyes E, Ulloa-Auirre A, Kofman-Alfaro S and Mendez J. P. A mutation in the 5′non-high mobility group box region of the SRY gene in patients with Turner syndrome and Y mosaicism. J. Clin.Endocrinol.Metab., 2000; 85:1908-1911.
CrossRef - Fernandez R, Marchal J. A, Sanchez A and Pasaro E. A point mutation, R59G, within HMG-SRY box in a female 45, X/46, X, psudic(Y) (pter–>q11::q11–>pter). Hum. Genet., 2002; 111:242-246.
CrossRef - Shahid M, Dhillon V. S, Aslam M and Husain S. A. Three new novel pointmutations localized within and downstream of High-Mobility Group-boxregion in SRY gene in three Indian females with Turner syndrome. J.Clin.Endocrinol. Metab., 2005; 90:2429-2435.
CrossRef - McElreavey K, Vilain E, Abbas N, Costa J. M, Souleyreau N, Kucheria K,Boucekkine C, Thibaud E, Brauner R, Flamant F and Fellous M. XY sex reversal associated with deletion 5 to the SRY “HMG-box” in the testis determiningregion. Proc. Natl. Acad. Sci. USA., 1992; 89:11016–11020.
CrossRef - Capel B. The battle of sexes. Mech. Dev., 2000; 92: 89–103.
CrossRef - Werner M. H, Bianchi M. E, Gronenborn A. M and Clore G. M. NMR spectroscopicanalysis of the DNA conformation induced by the human testis determiningfactor (SRY). Biochemistry., 1995; 34:11998–12004.
CrossRef - Page D. C. Hypothesis: a Y chromosomal gene causes gonadoblastoma indysgenetic gonads. Development., 1987; 101:151-155.
CrossRef - Lau Y. F. Gonadoblastoma, testicular and prostate cancers, and the TSPYgene. Am. J. Hum. Genet., 1999; 64:921-927.
CrossRef - Knudson A. G. (1971) Mutation and cancer: statistical study of retinoblastoma.Proc. Natl. Acad. Sci. USA., 1971; 68: 820–823.
CrossRef - Wilson M and Koopman P. Matching SOX: partner proteins and co-factorsof the SOX family of transcriptional regulators. Curr.Opin. Genet. Dev., 2002; 12:441–446.
CrossRef








