Manuscript accepted on :10-01-2022
Published online on: 21-01-2022
Plagiarism Check: Yes
Reviewed by: Dr. Tahmineh Mokhtari
Second Review by: Dr. Mangala Kohli, Dr. Sundarapandian S
Final Approval by: Dr. Ian Iames Martin
Janani Yoganandham1* , Arathi Mariappan Senthiappan1
, Arathi Mariappan Senthiappan1 , Suba Ananthi Kumarasamy2
, Suba Ananthi Kumarasamy2 , Vidhya Ramakrishnan3
, Vidhya Ramakrishnan3  and Ramesh Palanisamy4
and Ramesh Palanisamy4
1Department of Anatomy, Chettinad Academy of Research and Education, Chennai, Tamilnadu-600103, India
2Department of Anatomy, Indira Gandhi Medical College and Research Institute, Puducherry, Tamilnadu- 605009, India
3Department of Anatomy, International Medical School, MS Ramaiah Group of Institutions, Bangalore, Karnataka- 560054, India
4Department of Anatomy, Sri Siddhartha Medical College and Hospital, Tumakuru, Karnataka -572107, India
Corresponding Author E-mail: dryjanani@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2386
Abstract
Aim: To study the parameters that can help release the median nerve and its branch, the anterior interosseous nerve from entrapment neuropathies and various other lesions warranting surgical correction and infective and traumatic disorders of adjacent structures of the region. Materials and methods: Sixty four upper limbs belonging to South-Indian population were carefully dissected using the Cunningham’s Manual of Practical Anatomy, the axillary region was exposed, the cords of brachial plexus were traced and median nerve was identified with its relation to axillary artery. The upper limbs used were all disarticulated. The median nerve was further traced and exposed in the arm and forearm. Acromion process and medial epicondyle were considered as prominent bony landmarks for median and anterior interosseous nerves respectively. Measurements were taken using a non-stretchable thread and scale with the arm consistently placed in supine position. Results: The formation of the median nerve by the union of the lateral and medial roots was 11.83±2.36 cm and 11.58±2.057 cm on the right and left sides respectively located distal to the acromion process. The distance between the origin of the anterior interosseous nerve and the medial epicondyle was 8.946±1.084 cm on the right side and 8.875±1.109 cm on the left side. Conclusion: The knowledge of the level of union of two roots of median nerve and the origin of anterior interosseous nerve can be of use to surgeons and anatomists while marking the median nerve on the surface and also releasing the median and anterior interosseous nerves to relieve from various entrapment syndromes. The present study provides data that can facilitate easy identification of the prominent landmarks of the nerve during surgical procedures.
Keywords
Anterior Interosseous Nerve; Entrapment; Median nerve; Morphometry
Download this article as:| Copy the following to cite this article: Yoganandham J, Senthiappan A. M, Kumarasamy S. A, Ramakrishnan V, Palanisamy R. The Morphometric Measurements of Median and Anterior Interosseous Nerve in Entrapment Syndromes in South Indian Population – An Anatomical Guide. Biomed Pharmacol J 2022;15(1). |
| Copy the following to cite this URL: Yoganandham J, Senthiappan A. M, Kumarasamy S. A, Ramakrishnan V, Palanisamy R. The Morphometric Measurements of Median and Anterior Interosseous Nerve in Entrapment Syndromes in South Indian Population – An Anatomical Guide. Biomed Pharmacol J 2022;15(1). Available from: https://bit.ly/3fHw7Sm |
Introduction
The median nerve, also called the labourer’s nerve is among the largest branches of the brachial plexus arising from the medial and lateral cords through the union of its medial and lateral roots. The median nerve is very closely related to axillary and brachial arteries. The union of two roots of median nerve (lateral and medial) is usually anterior to the third part of axillary artery. Usually after crossing over the brachial artery in the arm, the nerve lies as the medial most content of the cubital fossa1. Despite an established knowledge regarding the median nerve’s origin, a lacuna was noted on the level of union of the two roots of median nerve and hence was attempted in this study. This can even be used as a landmark to mark the nerve on surface for surgical as well as teaching purposes.
The incidence of entrapment syndromes of median nerve at the level of forearm and elbow has been increasing significantly and the risk of injury to the anterior interosseous nerve also seem to be high due to various surgical procedures pertaining to the elbow joint. The origin of this branch has been measured with reference to many bony landmarks viz., anterior interosseous nerve origin was reported to be 4 ± 1.6 cm from humeral bi-epicondylar line according to Dubois de Mont-Marin G2. However, its distance from medial epicondyle was not measured and hence an attempt was made on this aspect. To ease out locating the nerve and also due to lesser intervening neurovascular structures between the nerve and the medial epicondyle, it was the chosen the point of reference in the present study.
Linell et al, studied the morphological measurements for the branches of median nerve i.e., the point of origin of the branch and the point of its entry into a muscle from specific bony landmarks. 3 In the present study, the origin of anterior interosseous nerve, a larger branch of the median nerve was calculated from the medial epicondyle of humerus was attempted due to its proximity to the same bony landmark. The medial epicondyle of humerus was considered the reference point as there are no major neurovascular structures present medial to the nerve here in the cubital fossa. This minimises any comorbidities that can arise due to involvement of adjacent neurovascular structures. Similar studies in the past took the lateral epicondyle of humerus as a reference point. 3,4 A study also says that the origin of the anterior interosseous nerve is roughly around 4cm distal to medial epicondyle and 5-8cm distal to lateral epicondyle. 5 A study by Kibar S et al., also described the mean origin of the nerve 37.58±11.25 mm distal to the interepicondylar line6.
The level at which the two roots of median nerve united was studied from coracoid process of scapula7. The distance from the anterior border of acromion process to where the roots of median nerve united was not found to be measured in the previous studies and hence was attempted in this study as the acromion process is easy to locate on surface. Also, the distance can be of great use while marking the topography of the nerve. The wide range of variations pertaining to the level of origin of median nerve made the study worth conducting.
Materials and methods
Sixty four upper limbs were dissected in Department of Anatomy at Chettinad Hospital and Research Institute. The laterality of the limbs was taken into account while the age and sex were not included. The study was conducted only on disarticulated upper limbs to maintain uniformity. Limbs that showed variations in the formation and median nerve were excluded from the study. The limbs were placed in normal anatomical position and measurements were recorded. The level of union of two roots of median nerve was measured from the anterior border of the acromion process. Pronator teres muscle was cut at its centre to trace the median nerve completely and thereby to locate the point of origin of anterior interosseous nerve. The distance at which the anterior interosseous nerve branched out was also measured with respect to the medial epicondyle. Both the measurements were done manually using a non-stretchable thread and scale. The measurements mentioned above were done thrice and the average calculated to avoid parallax errors.
Results
The average distance between the point of union of the two roots of median nerve from anterior border of acromion process was 11.83±2.36 cm and 11.58±2.057cm distally on the right and left sides respectively (Figure 1 & Graph 1). Paired t-test was done and the p-value was 0.67424 and was not significant (p-value was not <0.05). The point of origin of anterior interosseous nerve was 8.946±1.084 cm distal to the medial epicondyle on the right side and 8.875±1.109 cm from the same bony landmark on the left side (Figure 2 & Graph 2). Paired t-test was done and the p-value was 0.72001 and not significant as the p-value was >0.05. From both Graph 1 and 2, it can be elicited that there was not much difference between the right and left sides for both the parameters. The sex of the cadaver was not taken into account as the limbs were all disarticulated. The distance between the median nerve and the medial epicondyle was approximately 1.5±0.85 cm in the cubital fossa.
Table 1: Master chart (* AIN- Anterior interosseous nerve)
| S.No. | Union of 2 roots(Right) | Union of 2 roots (Left) | Origin of AIN* (Right) | Origin of AIN* (Left) |
| 1 | 8.4 | 9 | 5.2 | 5.5 |
| 2 | 12.9 | 9.2 | 5.7 | 9.4 |
| 3 | 9.7 | 9.4 | 6.8 | 9.3 |
| 4 | 10.4 | 9.7 | 9.4 | 9.2 |
| 5 | 19.8 | 11.2 | 9.6 | 9.3 |
| 6 | 13.2 | 10.8 | 9.2 | 8.2 |
| 7 | 13.6 | 11.3 | 8.2 | 9.2 |
| 8 | 9.4 | 10.4 | 9.5 | 9.4 |
| 9 | 10.8 | 9.4 | 8.5 | 9.3 |
| 10 | 10.2 | 10.1 | 9.5 | 8.2 |
| 11 | 11.1 | 10.4 | 9.2 | 9.3 |
| 12 | 13.7 | 12.6 | 8.9 | 9.1 |
|
13 |
8.9 | 11.1 | 9.2 | 9.4 |
| 14 | 14.6 | 9.9 | 9.1 | 8.3 |
| 15 | 10.2 | 11.9 | 9.2 | 8.3 |
| 16 | 10.7 | 11.2 | 9.3 | 9.3 |
| 17 | 14.4 | 11.2 | 9.2 | 9.4 |
| 18 | 10.8 | 11.8 | 9.4 | 9.2 |
| 19 | 14.2 | 12.8 | 8.9 | 9.3 |
| 20 | 16.1 | 20.2 | 10.0 | 8.2 |
| 21 | 9.6 | 9.9 | 9.4 | 9.4 |
| 22 | 10.8 | 11.2 |
9.2 |
9.4 |
| 23 | 11.4 | 12.7 | 9.2 | 9.2 |
| 24 | 11.2 | 12.6 | 9.3 | 6.8 |
| 25 | 10.3 | 13.4 | 9.4 | 9.2 |
| 26 | 12.8 | 12.6 | 8.4 | 9.3 |
| 27 | 11.3 | 11.8 | 9.5 | 8.2 |
| 28 | 10.2 | 11.7 | 9.6 | 9.2 |
| 29 | 10.8 | 13.8 | 9.7 | 9.3 |
| 30 | 12.4 | 12.6 | 9.7 | 8.7 |
| 31 | 10.8 | 13.6 | 9.2 | 9.3 |
| 32 | 13.9 | 11.3 | 9.7 | 9.2 |
| Average | 11.83125 | 11.5875 | 8.946 | 8.875 |
| SD | 2.361988 | 2.057 | 1.084 | 1.10947 |
| Median | 10.8 | 11.2 | 9.2 | 9 |
| Range | 8.4 – 19.8 | 9-20.2 | 5.2-10 | 5.5-9.4 |
| t-Test | p value -0.67424 | p value -0.72001 | ||
|
Significance |
Not significant |
Not significant |
||
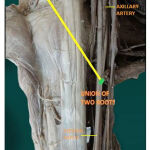 |
Figure 1 |
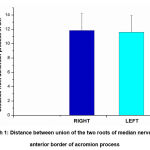 |
Graph 1: Distance between union of the two roots of median nerve and anterior border of acromion process |
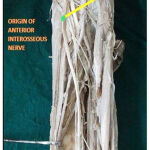 |
Figure 2 |
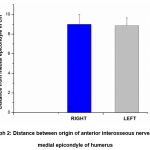 |
Graph 2: Distance between origin of anterior interosseous nerve and medial epicondyle of humerus |
Discussion
The median nerve and its branches can get compressed at very many places along its course which makes the study pertaining to the nerve very significant. One of the common reasons for compression of median nerve near its formation is the presence of Langer’s axillary arch. The nerve can be compressed due to the presence of a hypertrophied pectoralis minor, thickened clavipectoral fascia and sometimes by lipoma arising from adjoining soft tissue as well. Occasionally, aneurysms of the regional arteries can also result in its compression.
The level of union of the two roots i.e., the level of formation of the median nerve with respect to the anterior border of acromion process was measured bilaterally following dissection (Fig.1). The average level of formation of the nerve on the right side was 11.83±2.36 cm while on the left side it was found to be 11.58±2.057cm. The range obtained, common to both sides was 8.4 cm to 20.2 cm (right side: 8.4 cm to 19.8 cm; left side: 9 cm to 20.2 cm). The mean values obtained were almost similar on both sides (Graph 1).
The median values were also calculated. The median value for the right sided limbs was 10.8 cm while that for the left sided limbs was 11.2 cm. These values can probably be of use to the surgeons while marking the nerve topographically as soon after this, the nerve courses over the brachial artery and is in proximity with the same at the middle of arm. The nerve can be located along the lateral wall of axilla at the junction of anterior 2/3rd and posterior 1/3rd of the arm. This point coincides with the midpoint between the lower borders of pectoralis major and teres major muscle and also with the point of origin of brachial artery. However, owing to the nerve’s superficial relation to the artery, its identification intra-operatively should not be cumbersome.
Hence to mark median nerve on the surface, the distance between the acromion process and the point of union denoting the region at which both formative roots of the nerve unite, in front of the third part of axillary artery can be taken as the first point. The second point can be marked at the centre of the cubital fossa and the third point can be marked just lateral to the palmaris longus tendon at the level of the wrist. The line joining the three points can represent the median nerve. Apart from being useful to the surgeons, this can also be used for educating the undergraduate and postgraduate students regarding marking the median nerve on the surface.
The tendon of palmaris longus can be identified for its presence by one of the following methods:
Schaeffer’s test (Standard test): Opposition of thumb to the little finger followed by flexion of the wrist. 8
Thompson’s test: A fist is made followed by flexion of the wrist and opposition of the thumb over the flexed fingers.9
Mishra’s test 1: Flexion of wrist following passive hyperextension at metacarpo-phalangeal joints.10
Mishra’s test 2: With the wrist in palmar flexion, the thumb is abducted against resistance.10
Pushpakumar’s two-finger sign method: Extension of middle and index finger followed by flexion of other fingers and wrist, completed by opposition and flexion of thumb.11
The above mentioned tests are useful in detecting the presence of palmaris longus tendon. Various other available methods can also be used to detect the tendon of palmaris longus like open hand test, Lotus test, four finger test , Gangata test , Bhattacharya’s flexion test. In a study done by Kigera et.al., Schaeffer’s test was found to show the presence of the tendon in many number of cases. 12 However in case of absence of the tendon, an alternate method has to be identified to mark the third point for the median nerve which roughly corresponds to the middle of the anterior wrist.
A study on the brachial plexus and the length of various branches of median nerve- from the point of origin and entry into the muscle was studied,3 However, the point of union of the two roots of median nerve was not measured by this investigator.
Level of origin of Anterior interosseous nerve:
The entrapment syndrome of this nerve was first described by Parsonage and Turner in 1948 followed by Kiloh and Nevin’s description (Kiloh-Nevin syndrome) of it as a lesion of anterior interosseous nerve alone in 1952. Since then, multiple treatment options, both surgical and non-surgical have been tried with varying degree of outcome. The anatomy of anterior interosseous nerve was studied in detail in previous studies.[13] Due to the increased risk of compression of the nerve in anterior interosseous nerve syndrome, it is worthy to study the point of origin of the nerve in order to prevent its injury or to undertake decompression procedures. The origin of anterior interosseous nerve measured from the medial epicondyle was found to be varying. The measurements were taken with respect to the medial epicondyle of the humerus. (Fig.2)
In the present study, the mean origin of the nerve from medial epicondyle, which is more prominent and a safer landmark than the lateral epicondyle (as neurovascular structures do not intervene in the same plane), on the right and left sides were found to be 8.946±1.084 cm and 8.875±1.109 cm respectively. The values obtained exhibited bilateral similarity. (Graph 2).
However, a previous study reported the origin of the nerve to be approximately 5 cm from the lateral epicondyle 4. The median values were also calculated for the right and left sides. They were 9.2 cm and 9 cm on the right and left sides respectively. The range of level of origin of the nerve on the right side was from 5.2 cm to 10 cm, while on the left side it was from 5.5 cm to 9.4 cm. Linell EA found the anterior interosseous nerve to be originating at about 5.24 cm from the lateral epicondyle. 3 The nerve was reported to have taken origin 5cm from the lateral epicondyle. 4
Lesion of anterior interosseous branch alone is rare and is usually associated with other variants seen along the course of the nerve. 14 The median nerve can possibly get compressed between the pronator teres heads. The patient presents with dull ache in the upper forearm. The pain worsens on continued strenuous activity involving the muscle and nerve. It is associated with sensory loss in hand over its territory of distribution which helps in differentiating the condition from anterior interosseous nerve syndrome. The condition can be tested by applying resistance over the ventral aspect of wrist while asking the patient to pronate against resistance. Resistance is usually applied three finger breadths below the elbow over the pronator teres muscle.15
Median nerve and brachial artery have been reported as prone to injury while releasing lateral supracondylar muscle mass due to extracapsular elbow contractures by anterior dissection. The nerve if involved can result in transient median neuritis due to its stretching. 16 The injury to the neurovascular structures can be minimised by dissecting for the median nerve from the medial aspect as the brachial artery lies further lateral to the nerve itself.
Injury to the anterior interosseous branch of median nerve has been reported by various authors. There are various etiologies like spontaneous palsy,17-20 accessory head of flexor pollicis longus (Gantzer’s muscle), 21 crescentic band extending between the insertion of brachialis and aponeurosis on the deep surface of pronator teres,22 displaced forearm fracture (multiple and Galeazzi’s fracture),23,24 compression due to constrictive dressing post-operatively,25 injury due to blunt trauma, sleeping on the affected arm or a poorly applied cast 26, during venepuncture at cubital fossa 27, nerve tumor 28, post internal fixation of proximal end of radius 29, the Struthers ligament (extending between the medial epicondyle and supracondylar spur) compressing the nerve though it is seen in 1% of the population only 30 , lacertus fibrosis and arterial thrombosis31.
These values obtained above for the level of origin of anterior interosseous nerve, can be of great significance to the surgeons in order to prevent injury while operating on patients for release during pronator syndrome and anterior interosseous nerve syndrome. It can also be useful while operating on the bones of forearm during fractures or dislocation of the head of the radius from the annular ligament in case of children. These values should be borne in mind because it is a significant branch of the median nerve and the branch usually supplies muscles in the deeper aspects of anterior compartment of forearm.
Surgical significance
The median nerve can get compressed in the arm due to axillary arch, thickening of clavipectoral fascia and hypertrophy of pectoralis minor and lipoma of adjoining soft tissue[31,32]. Aneurysms of axillary and brachial artery can also compress the nerve at axilla and forearm[33]. The nerve can get injured while surgically correcting the diaphyseal fracture of humerus. At the cubital fossa, compression of the nerve can take place due to its course below the Struther’s ligament, due to thrombophlebitis of the antecubital vein, tendinous structures like origin of flexor digitorum superficialis, Gantzer’s muscle and bicipital aponeurosis. Ischaemic neuropathy following arterio-venous fistula can also occur result in numbness, paraesthesias, tingling sensation along its course of distribution. Other possible causes for injuries of the nerve can be trauma or electrical burns. This study conducted by us can prove highly significant in locating the formation as well as deep branch of median nerve during its surgical correction.
The study can further be enhanced by taking into consideration the age, sex and length of the upper limbs dissected. Measurements of the median nerve from the medial epicondyle to the point of crossing-over of the median nerve and brachial artery in the arm can be taken into account. This can help in tracing of the median nerve topographically accurate. The point of origin of recurrent motor branch of median nerve can also be measured from the adjacent bony landmarks as this can be of use during the release of the nerve from carpal tunnel.
Conclusion
The median nerve is highly susceptible to variations. The level of union of the two roots of median nerve from the anterior border of acromion process can be of use while performing surgeries pertaining to the shoulder region. However, care has to be taken as the point of formation of the nerve is in close association with the axillary and brachial arteries and these vessels as well as their branches can be easily ruptured. The connection of the points mentioned above can be of use for both educative and surgical purposes as it helps in the identifying the nerve topographically. Both, the mean level of formation of median nerve and the mean level of origin of anterior interosseous nerve are is almost similar bilaterally. The level of origin of anterior interosseous nerve can also be of significance to the orthopaedic surgeons in particular due to the increasing frequency of surgeries performed in forearm for correction of fractures of radius and ulna and also while releasing the nerve from compression during its entrapment. Despite being rare, a weak flexor pollicis longus and radial flexor digitorum profundus are indicative of anterior interosseous nerve syndrome. The use of radiological investigations like MRI with other electrodiagnostic studies aid in the diagnosis of anterior interosseous syndrome along with its appropriate aetiology.
Acknowledgment
Our sincere gratitude to all the non-teaching staff who have helped us in the process of conducting the study.
Conflicts of interest
None
Funding source
None
References
- Gosling, J. A., Harris, P. F., Humpherson, J. R., Whitmore, I., Willan, P. L. T., & Gosling, J. A. (2017). Human anatomy: Color atlas and textbook. Upper limb :84
CrossRef - Dubois de Mont-Marin G, Laulan J, Le Nen D, Bacle G. Topographic anatomy of structures liable to compress the median nerve at the elbow and proximal forearm. Orthop Traumatol Surg Res. 2021;107(2):102813.
CrossRef - Linell EA. The distribution of nerves in the upper limb, reference to variabilities and their clinical significance. J Anat 1921; 55:79-112.
- Arenas AJ, Artazcoz FJ, Tejero A, Arias C. Anterior interosseous nerve injury associated with a Monteggia fracture-dislocation. Acta Orthop Belg 2001; 67:77-80.
- Abdulla Aljawder, Mohammed Khalid Faqi, Abeer Mohamed, and Fahad Alkhalifa Anterior interosseous nerve syndrome diagnosis andintraoperative findings: A case report Int J Surg Case Rep. 2016; 21: 44–47.
CrossRef - Kibar S, Bileceno¤lu B, Filgueira L, Uz A. Morphometry of the anterior interosseous nerve: a cadaveric study. Anatomy 2018;12(3):111–114
CrossRef - Iyer P, Rajagopal L. Variations in the formation of the median nerve. Natl J Integr Res Med 2016;7(3):17-20
- Schaeffer JP. On the variations of the Palmaris longus muscle. Anat Rec 1909; 3: 275-78.
- Thompson JW, Mcbatts J, Danforth CH. Hereditary and racial variations in the musculus palmaris longus. Am J Phys Anthro 1921; 4: 205-18.
CrossRef - Mishra S. Alternative tests in demonstrating the presence of palmaris longus. Indian J Plast Surg 2001; 34: 12-14.
- Pushpakumar SB, Hanson RP, Caroll S. The ‘two finger’ sign, clinical examination of palmaris longus (PL) tendon. Br J Plast Surg 2004; 57: 184-85.
CrossRef - Kigera JW, Mukwaya S. Clinical assessment of the palmaris longus: accuracy of common tests. Ann Afr Surg 2012;9:41–44.
- Spinner M. The anterior interosseous nerve syndrome with special attention to its variations. J Bone Joint Surg 1970; 52: 84-94.
CrossRef - O’brien MD, Upton ARM. Anterior interosseous nerve syndrome: A case report with neurophysiological investigation. J Neurol Neurosurg Psychiatry 1972; 35: 351.
CrossRef - Birnie R, Reider B. Elbow and forearm. In Reider B editor. The orthopaedic and physical examination, 1st Philadelphia: Saunders WB; 1999. P 81-93.
- Katolik LI, Cohen MS. Elbow stiffness: Lateral column release for extracapsular elbow contractures. In: Williams GR, Ramsey ML, Weisel SW, editor. Operative techniques in shoulder and elbow surgery, 5th Philadelphia: Wolter Kluwer, Lippincott Willaimas and Wilkins; 2011: 370.
- Nagano A. Spontaneous anterior interosseous nerve palsy. J Bone Joint Surg(Br) 2003; 85: 313-18.
CrossRef - Turner JW, Parsonage MJ, Neuralgic amyotrophy (paralytic brachial neuritis): with special reference to prognosis. The Lancet 1957; 270: 209-12.
CrossRef - Kiloh LG, Nevin S. Isolated neuritis of the anterior interosseous nerve. Br Med J 1952; 1: 850.
CrossRef - Vichare NA. Spontaneous paralysis of the anterior interosseous nerve. J Bone Joint Surg (B) 1968; 806-8.
CrossRef - Gunnal SA, Siddiqui AU, Daimi SR, Farooqui MS, Wabale RN. A study on the accessory head of the flexor pollicis longus muscle (Gantzer’s muscle). J Clin Diagn Res 2013; 7: 418-21.
- Fearn CB, Goodfellow JW. Anterior interosseous nerve palsy. J Bone Joint Surg Br 1965; 47:91-3.
CrossRef - Warren JD. Anterior interosseous nerve palsy as a compilation of forearm fractures. J Bone Joint Surg 1963; 45: 511-12.
CrossRef - Engber WD, Keene JS. Anterior interosseous nerve palsy associated with a Monteggia fracture. A case report. Clin Orthop Relat Res 1983; 174: 133-7.
CrossRef - Casey PJ, Moed BR. Fractures of forearm complicated by palsy of the anterior interosseous nerve caused by a constrictive dressing. A report of four cases. J Bone Joint Surg Case Connector 1997; 79: 122-4.
CrossRef - Puhaindran ME, Wong HP. A case of anterior interosseous nerve syndrome following peripherally inserted central catheter (PICC) line insertion. Singapore Med J 2003; 12: 653-4.
- Zubairy AI. How safe is blood sampling? Anterior interosseous nerve injury by venepucture. Postgrad Med J 2002; 78: 625.
CrossRef - Da silva MR, Vidinha V, Negarao P. Nerve tumour as a rare cause of anterior interosseous nerve palsy. J Hand Surg Eur 2013; 38: 562-3.
CrossRef - Hope PG. Anterior interosseous nerve palsy following internal fixation of the proximal radius. J Bone Joint Surg (Br) 1988; 70: 280-82.
CrossRef - Namerow NS, Campion DS, Bluestone R, Cracchiolo A. Peripheral nerve entrapments. West J Med 1977; 127: 299-313.
- Weinzweig N, Brownw EZ jr. Infraclavicular median nerve compression caused by a lipoma. Orthopaedics 1998; 1077-8.
CrossRef - Hossein Akhondi; Matthew Varacallo. Anterior Interosseous Syndrome StatPearls. NCBI Update: August 10, 2020. Bookshelf ID: NBK525956PMID: 30247831
- Ortiz-Pomales Y, Smith J, Weiss J, Casey K. Tortuous axillary artery aneurysm causing median nerve compression. Ann Vasc surg 2014; 28: 122.
CrossRef







