Manuscript accepted on :16-11-2021
Published online on: 22-11-2021
Plagiarism Check: Yes
Reviewed by: Dr. Tejaswi Chavan Teju

Second Review by: Dr. Salman Ahmed Pharmacognosy

Final Approval by: Dr. Omar M. E. Abdel-Salam
Priyanka Kenkare1 , Shravan Shetty1*
, Shravan Shetty1* , Utkarsh Mangal2
, Utkarsh Mangal2 , Ashith MV1
, Ashith MV1 and Siddarth Shetty1
and Siddarth Shetty1
1Department Of Orthodontics and Dentofacial Orthopaedics, Manipal College of Dental Sciences, Mangalore, Manipal Academy of Higher Education, Manipal, Karnataka, India-576104.
2Department of Orthodontics, Yonsei University College of Dentistry, Seoul, South Korea.
Corresponding Author E-mail: shravan.shetty@manipal.edu
DOI : https://dx.doi.org/10.13005/bpj/2307
Abstract
The first important step in orthodontic treatment is an accurate diagnosis and precise treatment planning to correct the malocclusion. This process entails a proper examination and understanding of the nature of malocclusion and the anomaly of the underlying structures. The emergence of three dimensional (3D) technology has transformed the field of orthodontics. The present article aims to take into account some of the applications of 3D technology in the field of orthodontics.
Keywords
Bone Plates; Clear Aligner Appliances; Bone anchored maxillary protraction; 3D Imaging; Orthodontic Appliance Design; Three Dimensional Printing
Download this article as:| Copy the following to cite this article: Kenkare P, Shetty S, Mangal U, Ashith M. V, Shetty S. The Utilization of Three-Dimensional Technology for an Accurate Diagnosis and Precise Treatment Planning in the Field of Orthodontics. Biomed Pharmacol J 2021;14(4). |
| Copy the following to cite this URL: Kenkare P, Shetty S, Mangal U, Ashith M. V, Shetty S. The Utilization of Three-Dimensional Technology for an Accurate Diagnosis and Precise Treatment Planning in the Field of Orthodontics. Biomed Pharmacol J 2021;14(4). Available from: https://bit.ly/3FD6T2A |
Introduction
An accurate Orthodontic diagnosis involves evaluation of all the dimensions of the facial skeleton, determining the nature of the malocclusion and any underlying asymmetry as it might be a combination of hard-tissue, dental and soft-tissue components. Conventional treatment planning with two-dimensional (2D) imaging, are reported to have suboptimal outcomes especially in patients for treatment of the facial asymmetry requiring a correction of pitch, roll and yaw.1
Conventional treatment planning involving the use of lateral cephalograms and orthopantomograms is now revolutionized with the advent of Cone Beam Computed Tomography (CBCT). CBCT is a technique which overcame the shortcomings of conventional computed tomography scan and also reduced the amount of radiation exposure for patients.2 The use of CBCT allows a better understanding of the skeletal anomalies by providing a three-dimensional visualization of the facial skeleton including a thorough assessment underlying skeletal morphology and temporomandibular joint complex. The paradigm shift from 2D to three-dimensional (3D) technology has not only facilitated sound diagnosis and efficient treatment planning by eliminating overlap of structures and parallax error but also allowed the orthodontist to assess risk factors, predict treatment outcomes, assess skeletal growth changes and treatment progress.3 The use of CBCT along with 3D simulation, treatment planning coupled with additive manufacturing has revolutionized the field of orthodontics as it allows the practitioner to emulate the clinical scenario in the confines of the laboratory setting.
Applications of 3D workflow module in Orthodontics
Virtual setup for diagnosis
The advantages of using virtual models over conventional dental casts is the possibility of spatial registration. Virtual models made during the treatment can be combined on the same co-ordinate system.4 In 3D diagnosis and treatment planning initially a scan of the teeth and adjacent structures is captured either by direct intraoral scanning or using table-top scan of the plaster model of the patients’ to acquire digital data [data type: Standard Triangle Language (STL), Polygon File Format (PLY), Wavefront OBJect (OBJ)]. The digitized data file can now be transferred from the scanner to the Computer Aided Designing (CAD) software [ex. Planmeca Romexis 3D Ortho Studio (Planmeca,Oy, Helsinki, Finland)].The software allows the orthodontist to create virtual orthodontic study models. The virtual models are oriented as per the occlusion and segmented to finalize the virtual setup. The individual teeth then can be moved into the desired positions with the required amount of tip, torque and mesio-distal, bucco-lingual and vertical displacements. It is also possible to simulate individual jaw movements to obtain an ideal digital setup akin to the Kesling setup which signifies the final occlusion of the patient (Figure 1A and 1B).
 |
Figure 1: A) Pre-treatment maxillary and mandibular intra-oral photographs, B) 3D treatment simulation on maxillary and mandibular virtual setup. |
The adjustments made are assessed for bilateral symmetry, occlusion and Kesling accuracy in 1st, 2nd and 3rd order specifications. This virtual setup obtained is more precise than the Kesling setup laboratory procedures.5
Lingual orthodontics
In the recent times, with an increase in demand of adult orthodontics, there is also an increase in the demand for inconspicuous esthetic orthodontic procedures. Lingual orthodontics and clear aligners provide the solution to this by giving successful treatment outcomes without compromising the facial aesthetics during the orthodontic treatment.
Lingual orthodontics involves the bonding of orthodontic appliances on the lingual or palatal aspect of the teeth facilitating an esthetically acceptable orthodontic appliance. However, it is difficult to attain a precise bracket positioning due to reduced visibility and varied or complex anatomy of the lingual or palatal aspect of the teeth. A number of lingual orthodontic techniques such as HIRO technique, CLASS system (custom labial/lingual appliance setup service), KIS system (Korean indirect system), TAD –BPD (torque angulation device – bracket positioning device), TARG (torque angulation reference guide) and Incognito technique6-9 allow accurate bracket positioning and successful treatment outcomes. Amongst these, the HIRO technique is most commonly used as it is simple and economical.6 However, it is a highly technique sensitive system and relies on fabrication of an accurate orthodontic set-up upon which the final finishing of the lingual orthodontic treatment depends.
The use of digital technology such as 3D scanning of models, virtual treatment simulation with 3D printing options has transformed the technique of lingual indirect bonding.10 It allows precise bracket positioning with appropriate tip and torque incorporation in the bracket base facilitating optimum orthodontic tooth movement. Incognito technique9 allows us to customize the brackets and wires using CAD/CAM technology on a 3D model of the patient’s dentition. The brackets boned onto the tooth surfaces have an inbuilt torque and tip required for specific tooth movement. The brackets and wires are manufactured in gold alloys and the wire bending is done by wire-bending robot.
Hybrid Hiro technique10 uses digital models scanned from the patients’ study models. 3D treatment simulation is done using a software and a virtual setup representing the final treatment outcome is created (Figure 2) before printing. The 3D printed models are used as a template for bracket positioning. The models are duplicated in plaster and a 0.017” x 0.025” mushroom arch shaped rectangular stainless-steel wire is adapted to the plaster models. The lingual brackets are later positioned and bonded onto the model using the 0.017”x 0.025” mushroom arch wire as guide.5,10
 |
Figure 2: A) Pre-treatment maxillary intraoral photograph, B) Pre-treatment digital model of the maxilla, C) Treatment simulation of the maxillary dentition. |
Transfer trays are fabricated using Memosil (Heraeus Kulzer, Hanau, Germany) and after bracket preparation, these brackets are transferred to the patient’s mouth (Figure 3) using the indirect bonding technique. This procedure allows an accurate bracket positioning, facilitating a precise control over tooth movements and optimum treatment outcomes.
 |
Figure 3: A) 3D printed model of maxillary dentition representing final treatment outcome, B) Pre-treatment intraoral photograph with brackets bonded by indirect bonding. |
Clear aligners
Although lingual appliances are inconspicuous, some patients find them uncomfortable and unhygienic. The increasing demand for esthetic and comfortable orthodontic treatment has been met with clear aligners. They are transparent, comfortable and can be worn all day. Studies show that clear aligners are used to treat various kinds of malocclusion, however it lacks the ability to perform certain complex orthodontic tooth movements such as extrusion, severe rotations.11-13 In the recent years, certain improvements have been made to the appliance to allow better control of tooth movements.14,15
The technique of fabrication of the clear aligners involves the use of digital models and computerized 3D technology to visualize and virtually move the teeth in an ideal position. Following the virtual treatment simulation, a series of models are 3D printed which signifies the entire sequence of tooth movement and correction of malocclusion from the beginning to the end. Sequential array of stage-specific aligners are then vacuum formed over the then 3D printed models.
The process of manufacturing of the aligners is evolving continuously to develop biologically compatible resins with ideal safety profiles and physical properties that can be used for extended duration inside the mouth, and to attempt to use these resins to produce direct-3D printed aligners.16
Bone anchored maxillary protraction
Bone anchored maxillary protraction involves the use of skeletal anchorage by means of plates anchored to the infrazygomatic or lateranasal region of the maxilla and symphyseal or parasymphyseal region of the mandible to bring about true orthopedic changes. In these cases, an accurate adaptation of the plates over the bony contours of the maxilla and mandible for maxillary protraction is of utmost importance as it affects their stability and thereby the treatment outcomes. A stable plate placement will allow application of sufficient force required for protraction of the maxilla to correct a Class III skeletal malocclusion. It is also imperative that the orthodontist must have a proper control over the force vector, i.e. the elastics must be engaged in such a way that the force vector is at an angle of 30o to the occlusal plane. This force vector will allow for proper downward and forward protraction of the maxilla.17
Adaptation of the plates during the surgical procedure is cumbersome and will increase the duration of the surgery. It is difficult for the orthodontist to determine the positions of the plates as the adaptation and placement will be done by the oral surgeon. Benefitting from the 3D workflow setup, preoperative adjustments of the plate allows the orthodontist to have a full control on the plate positioning. The patient’s CBCT scan is used to obtain a DICOM (Digital Imaging and Communications in Medicine) file, which is later converted to a STL file for 3D printing. A 3D printed model of the patient’s maxilla and mandible is later constructed. These models replicate the bony contours of the patient’s facial skeleton and are used to pre-adapt the plates according to these bony contours (Figure 4). The pre-adapted plates are then sterilized and placed at the planned positions on the patient’s maxilla and mandible by the surgeon. This procedure facilitates precise plate placement in accordance with the orthodontists’ treatment plan, allowing a precise control over the force vector to allow for optimum maxillary protraction and successful treatment outcomes.
 |
Figure 4: Plates adapted on 3D printed models of maxilla and mandible. |
Orthognathic surgery
The correction of skeletal discrepancies involved orthognathic surgery alone without any orthodontic treatment till 1960s.18 This led to a poor stability of the correction due to presence of occlusal imbalance.
Thus the concept of pre-orthognathic orthodontic treatment was introduced to increase the stability of correction and reduce the amount of relapse. The correction of severe dentofacial anomalies conventionally consists of three stages, pre-orthognathic orthodontic treatment to relieve the dental compensations followed by the orthognathic surgical procedure and finally post-surgical orthodontics to settle the occlusion. However, dental decompensation prior to surgery might lead to worsening of the patients’ esthetics, masticatory discomfort, psychosocial problems due to delay in addressing the patients’ chief complaint, iatrogenic problems due to long term orthodontic treatment.
The procedure of pre-orthodontic orthognathic surgery was introduced by Behrman and Behrman19 in 1988 to overcome the disadvantages of pre-surgical orthodontic treatment. They noted that the soft tissues settles the teeth post-surgically, reducing the time for post-surgical orthodontics and overall treatment time.20 The indications for this approach include cases with well aligned to mildly crowded anteriors, normally inclined or slightly proclined teeth, minimal transverse discrepancies, severe skeletal discrepancies without any dental decompensations.19 In this approach, occlusion cannot be used as a guide to establish treatment goals. Comprehensive treatment planning is required to assess the skeletal disharmony and to predict the post-surgical occlusion which will require orthodontic correction.
Conventionally, orthognathic surgery planning involved the use of plaster models, face bow transfer and articulators. Mock up surgery is done initially with the use of plaster models and articulators, and later this set-up is used to make intermediate and final splints. These surgical splints are fabricated using acrylic and are used for the final positioning of the maxilla and mandible during the surgical procedure. The manual procedure is more time consuming. However, inaccuracy has been observed in each step of this procedure which is transferred the next step.21-24
The use of three-dimensional technology allows us to plan the surgical procedure digitally. Using the patients three dimensional imaging file, the surgical osteotomies, reposition of osteotomized bones, can be simulated and the predicted postoperative results of the skeletal, dental and soft tissues can be visualized in 3D on the computer screen. Later, the corresponding inter-maxillary splint files are generated virtually (Figure 5). These splint files are then 3D printed and sterilized before transferring them to the operating room.
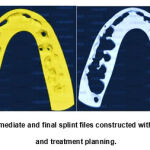 |
Figure 5: Intermediate and final splint files constructed with 3D simulation and treatment planning. |
This three-dimensional technology helps in reducing the inaccuracies seen with the manual technique, attain stable post-surgical outcomes with an understanding of the developing malocclusion, saving surgical preparation time and more precise treatment planning.25
Distraction Osteogenesis
The technique of distraction osteogenesis was first introduced by Ilizarov26-28 for elongation of long bones. This similar concept can be used for the bones of the facial skeleton such as the maxilla and mandible. This is indicated in cases presenting with craniofacial anomalies requiring reconstruction of the craniofacial structures. In comparison with the distraction osteogenesis of the long bones, distraction of the bones of the facial skeleton is more complex as there is a requirement of 3D distraction.29 A meticulous treatment planning with precise adaptation of the distractor onto the bony contours of the maxilla and the mandible, determination of the force vectors, accurate placement of the osteotomy cuts, treatment simulation and an accurate transfer of the appliance onto the patient skeleton is of utmost importance for successful treatment outcomes.30
The distraction can be done by using an intraoral or extraoral distractor. The use of 3D printed stereolithographic models allows the operator to adapt the appliance precisely onto the bony contours to allow for increased stability and a control over the force vector exerted for distraction.31
Conclusion
The use of three dimensional simulation and treatment planning has overcome a number of shortcomings seen in the conventional treatment planning which was mainly based on two dimensional records. It has enhanced the precision of treatment planning and allowed the orthodontist to predict the treatment outcomes.
Acknowledgment
None
Conflict of Interest
There is no conflict of interest.
Funding Sources
There is no funding source.
References
- Moro A, Correra P, Boniello R, Gasparini G, Pelo S. Three-dimensional analysis in facial asymmetry: comparison with model analysis and conventional two-dimensional analysis. J Craniofac Surg. 2009 Mar;20(2):417-22.
CrossRef - Halazonetis DJ. From 2-dimensional cephalograms to 3-dimensional computed tomography scans. Am J Orthod Dentofacial Orthop. 2005 May;127(5):627-37.
CrossRef - Valiathan A, Dhar S, Verma N. 3D CT imaging in orthodontics: adding a new dimension to diagnosis and treatment planning. Trends Biomater Artif Organs. 2008 Jan 1;21(2):116-20.
- Grauer D, Cevidanes LH, Tyndall D, Styner MA, Flood PM, Proffit WR. Registration of orthodontic digital models. Craniofacial growth series. 2011;48:377.
- Barreto MS, Faber J, Vogel CJ, Araujo TM. Reliability of digital orthodontic setups. Angle Orthod. 2016 Mar;86(2):255-9.
CrossRef - Hiro T, De la Iglesia F, Puigdollers A. Indirect bonding technique in lingual orthodontics: the HIRO system. Prog Orthod 2008;9(2):34-55.
- Fillion D. Lingual orthodontics: a system for positioning the appliances in the laboratory. L’ Orthodontie Francaise. 1989 ;60 Pt 2:695-704.
- Sheffield P. Labial/Buccal indirect bonding: A new manual method. APOS Trends in Orthodontics. 2012 Jul 1;2(4):4.
CrossRef - Wiechmann D, Rummel V, Thalheim A, Simon JS, Wiechmann L. Customized brackets and archwires for lingual orthodontic treatment. Am J Orthod Dentofacial Orthop 2003;124:593-9.
CrossRef - Mattua N, Virupakshab AM, Reddyc S. “The Hybrid HIRO”-Conventional HIRO System Integrated with 3D Scanning and Resin Prototyping. Journal of Contemporary orthodontics. 2017 March;1(2);32-40.
- Rossini G, Parrini S, Castroflorio T, Deregibus A, Debernardi CL. Efficacy of clear aligners in controlling orthodontic tooth movement: a systematic review. Angle Orthod. 2015 Sep;85(5):881–9.
CrossRef - Li W, Wang S, Zhang Y. The effectiveness of the Invisalign appliance in extraction cases using the the ABO model grading system: a multicenter randomized controlled trial. Int J Clin Exp Med. 2015;8(5):8276–82.
- Simon M, Keilig L, Schwarze J, Jung BA, Bourauel C. Treatment outcome and efficacy of an aligner technique–regarding incisor torque, premolar derotation and molar distalization. BMC Oral Health. 2014 Jun 11;14:68.
CrossRef - Kravitz ND, Kusnoto B, BeGole E, Obrez A, Agran B. How well does Invisalign work? A prospective clinical study evaluating the efficacy of tooth movement with Invisalign. American Journal of Orthodontics and Dentofacial Orthopedics. 2009 Jan 1;135(1):27-35.
CrossRef - Haouili N, Kravitz ND, Vaid NR, Ferguson DJ, Makki L. Has Invisalign improved? A prospective follow-up study on the efficacy of tooth movement with Invisalign. Am J Orthod Dentofacial Orthop. 2020 Sep;158(3):420-425.
CrossRef - Nakano H, Kato R, Kakami C, Okamoto H, Mamada K, Maki K. Development of Biocompatible Resins for 3D Printing of Direct Aligners. Journal of Photopolymer Science and Technology. 2019 Jun 24;32(2):209-16.
CrossRef - Keles A, Tokmak EÇ, Erverdi N, Nanda R. Effect of varying the force direction on maxillary orthopedic protraction. Angle Orthod. 2002 Oct;72(5):387-96.
- Kim JH, Mahdavie NN, Evans CA. Guidelines for “surgery first” orthodontic treatment. Orthodontics-basic aspects and clinical considerations. New York: InTech Publishing. 2012 Mar 9:265-300.
- Behrman SJ, Behrman DA. Oral surgeons considerations in surgical orthodontic treatment. Dent Clin North Am 1988: 32: 481-507.
- Peiró-Guijarro MA, Guijarro-Martínez R, Hernández-Alfaro F. Surgery first in orthognathic surgery: A systematic review of the literature. Am J Orthod Dentofacial Orthop. 2016 Apr;149(4):448-62.
CrossRef - Zizelmann C, Hammer B, Gellrich NC, Schwestka-Polly R, Rana M, Bucher P. An evaluation of face-bow transfer for the planning of orthognathic surgery. J Oral Maxillofac Surg. 2012 Aug;70(8):1944-50.
CrossRef - Utz KH, Müller F, Lückerath W, Fuss E, Koeck B. Accuracy of check-bite registration and centric condylar position. J Oral Rehabil. 2002 May;29(5):458-66.
CrossRef - Sharifi A, Jones R, Ayoub A, Moos K, Walker F, Khambay B, McHugh S. How accurate is model planning for orthognathic surgery? Int J Oral Maxillofac Surg. 2008 Dec;37(12):1089-93.
CrossRef - Bamber MA, Harris M, Nacher C. A validation of two orthognathic model surgery techniques. J Orthod 2001;28:135-142.
CrossRef - Zinser MJ, Sailer HF, Ritter L, Braumann B, Maegele M, Zöller JE. A paradigm shift in orthognathic surgery? A comparison of navigation, computer-aided designed/computer-aided manufactured splints, and “classic” intermaxillary splints to surgical transfer of virtual orthognathic planning. J Oral Maxillofac Surg. 2013 Dec;71(12):2151.e1-21.
CrossRef - Ilizarov GA. The principles of the Ilizarov method. Bull Hosp Jt Dis Orthop Inst. 1988 Spring;48(1):1-11.
CrossRef - Ilizarov GA. The tension-stress effect on the genesis and growth of tissues. Part I. The influence of stability of fixation and soft-tissue preservation. Clin Orthop Relat Res. 1989 Jan;(238):249-81.
CrossRef - Ilizarov GA. The tension-stress effect on the genesis and growth of tissues: Part II. The influence of the rate and frequency of distraction. Clin Orthop Relat Res. 1989 Feb;(239):263-85.
CrossRef - Gateno J, Allen ME, Teichgraeber JF, Messersmith ML. An in vitro study of the accuracy of a new protocol for planning distraction osteogenesis of the mandible. J Oral Maxillofac Surg. 2000 Sep;58(9):985-90; discussion 990-1.
CrossRef - Poukens J, Haex J, Riediger D. The use of rapid prototyping in the preoperative planning of distraction osteogenesis of the cranio-maxillofacial skeleton. Comput Aided Surg. 2003;8(3):146-54.
CrossRef - Varol A, Basa S. The role of computer-aided 3D surgery and stereolithographic modelling for vector orientation in premaxillary and trans-sinusoidal maxillary distraction osteogenesis. Int J Med Robot. 2009 Jun;5(2):198-206.
CrossRef







