Manuscript accepted on :18-11-2021
Published online on: 09-12-2021
Plagiarism Check: Yes
Reviewed by: Dr. Hind Shakir
Second Review by: Dr. Maha Jalal
Final Approval by: Dr. Fai poon
Carolina Muñoz-Corona1 , Elia Lara-Lona2
, Elia Lara-Lona2 , Christian Andrés Díaz- Chávez3
, Christian Andrés Díaz- Chávez3 , Gilberto Flores- Vargas4
, Gilberto Flores- Vargas4 , Daniel Alberto Díaz- Martínez5
, Daniel Alberto Díaz- Martínez5 , Francisco Javier Magos-Vázquez5
, Francisco Javier Magos-Vázquez5 , Daniela Peña-Succar1
, Daniela Peña-Succar1 and Nicolás Padilla- Raygoza4
and Nicolás Padilla- Raygoza4
1Division of Health Sciences, Campus Leon, Universidad de Guanajuato. Leon, México; C.P. 37670
2Department of Medicine and Nutrition, Division of Health Sciences, Campus Leon, University of Guanajuato, León, México C.P. 37670
3Department of Statistics, General Directorate of Planning and Development, Institute of Public Health of the State of Guanajuato, Guanajuato, Mexico C.P. 36250
4Department of Research and Technological Development, Directorate of Teaching and Research, Institute of Public Health from Guanajuato State, Guanajuato, Mexico C.P. 36250
5Directorate of Health Services, Institute of Public Health from Guanajuato State, Guanajuato, Guanajuato, Mexico C. P. 36000
Corresponding Author E-mail: npadillar@guanajuato.gob.mx
DOI : https://dx.doi.org/10.13005/bpj/2313
Abstract
Background. COVID-19 has caused 244,830 deaths in Mexico. Evaluating the severity of this contingency is possible if the hospital fatality rate of COVID-19 is described because hospitalized patients present more severe conditions. Objective. To analyze the fatality of COVID-19 in hospitalized patients. Methods. A quantitative, descriptive, analytical, cross-sectional, and retrospective study was conducted using open database from Ministry of Health in Mexico. Results. The analysis included 71,189 discharges from patients diagnosed with COVID-19 in the Mexican Ministry of Health Hospitals during 2020. Of them, 27,403 were due to death, predominantly in men and age groups from 50 to 69 years. The general hospital fatality due to COVID-19 was 38.49%, a hospital fatality of 40.75% in men and 35.03% in women. The 55-to-99-year-old age groups, Baja California, Puebla, and Coahuila had a higher hospital fatality than the general fatality. Conclusion. Besides the deaths caused directly by COVID-19 (those that occurred due to respiratory failures), many deaths were indirect in persons with comorbidities exacerbated by this disease. Access to health services, social changes derived from job loss, home protection, and changes in social dynamics, facts expressed in the general mortality excess, cannot be quantified in our study. There are similar patterns with other persons infected worldwide: this disease is more severe for males and older age subjects.
Keywords
COVID-19; Discharges; Death; Hospital Fatality
Download this article as:| Copy the following to cite this article: Corona C. M, Lona E. L, Chávez C. A. D, Vargas G. F, Martínez D. A. D, Vázquez F. J. M, Succar D. P, Raygoza N. P. Analysis of Hospital Lethality of COVID-19 in Mexico. Biomed Pharmacol J 2021;14(4). |
| Copy the following to cite this URL: Corona C. M, Lona E. L, Chávez C. A. D, Vargas G. F, Martínez D. A. D, Vázquez F. J. M, Succar D. P, Raygoza N. P. Analysis of Hospital Lethality of COVID-19 in Mexico. Biomed Pharmacol J 2021;14(4). Available from: https://bit.ly/3y8P7S8 |
Introduction
In December 2019, in Wuhan, China, there were alerts about cases of pneumonia of unknown etiology 1. On February 11, 2020, the World Health Organization (WHO) named its causative agent Coronavirus disease 2019 (COVID-19), while the International Committee on Taxonomy of Viruses (ICTV) named it a type of severe acute respiratory syndrome virus. -2 (SARS-CoV-2) 2. The WHO declared it a pandemic in March 2020 3. The first case of COVID-19 in Mexico was confirmed on February 28, 2020. As of June 25, 2021, 2,684,128 cases of COVID-19 had been confirmed with 244,830 deaths 4,5.
SARS-CoV-2 is a single-stranded RNA virus. It belongs to the Coronaviridae family and is a beta Coronavirus 6. Inhalation of respiratory droplets and aerosols is the main route of transmission 7. It has an incubation period of 1 to 14 days, where the clinical manifestations usually appear between the third and seventh day with typical signs and symptoms such as sore throat, fever, cough, fatigue, myalgias, nasal congestion, and runny, anosmia, difficulty in breathing 8. There are also atypical complaints such as diarrhea, nausea, and vomiting 9,10.
80% of SARS-CoV-2 cases resolve without requiring hospitalization, 15% require hospitalization, 5% require intensive therapy and support with invasive mechanical ventilation. Therefore, these last two scenarios present a severe condition due to COVID- 19 11. Being a man, having an advanced age and comorbidities such as diabetes mellitus, high blood pressure, obesity, cancer, and chronic kidney disease, predisposes to a severe COVID-19 due to SARS-CoV-2 8,12.
Hospital fatality
The number of patients infected by COVID-19 is underestimated. Some of the reasons are that besides the impossibility to carry out an adequate number of tests for its detection, asymptomatic patients, and those with mild symptoms or with scarce access to health services do not attend to medical revision 13,14. The Secretary of Health of the United Mexican States established guidelines to regulate the conduct of its health care staff during the contingency due to SARS-CoV-2 and has studied the impact of this disease by quantifying the number of confirmed cases and the observed mortality. Nevertheless, the lack of identification of patients infected by COVID-19 causes bias when calculating mortality, showing an unreliable picture to analyze the severity of this pandemic 15,16.
Hospitalized patients present a more severe disease due to this infection. Therefore, knowing how many of those hospitalized died (that is, knowing the hospital fatality) offers the possibility of identifying the severity of this pandemic more realistically. It is known that lethality is not synonymous with mortality; the first quantifies the severity of a disease, and the second measures the number of deaths that occurred in a determined population 17.
The coding of the International Classification of Diseases (ICD-10) has allowed the registration of patients from COVID-19 care centers in national platforms for easy monitoring of the pandemic. In this way, the ICD-10 code U071 is designated to cases of COVID-19 confirmed with a positive laboratory result. On the other hand, patients with suspected SARS-CoV-2 infection that meet clinical and epidemiological criteria, with proof of inconclusive or unavailable laboratory, are given the ICD-10 code U072 18. Thanks to national platforms, it is possible to calculate the hospital fatality rate of COVID-19 through its ICD-10 code since they allow to know the number of infected who required hospitalization and the number of deaths from this cause.
Institutions and countries have studied the behavior of the SARS-CoV-2 pandemic based on lethality. According to the WHO, the fatality rate for this disease ranges from 0.00% to 1.63% 19. The Pan American Health Organization estimated that Mexico had a fatality rate of 11%, becoming the country with the highest fatality rate in Latin America after the first 90 days of the pandemic 20. Hospital fatality has also been analyzed in other countries; In France, a hospital fatality rate from COVID-19 was 0.174% 21, in Italy, it was 29.7% 22. In Mexico, hospital fatality, studied in patients with invasive mechanical ventilation, was 80.9% 23.
This study aims to describe the hospital lethality of COVID-19 (or SARS-CoV-2) during 2020 in Mexican Hospitals from the Ministry of Health. For this purpose, we considered the patients registered with the condition ICD-10 U071 or ICD-10 U072.
Material and methods
Study design
The research protocol was approved by Ethics on Research Committee from Hospital General Silao from the Institute of Public Health from Guanajuato State (ISAPEG).
A quantitative, descriptive, analytical, cross-sectional, and retrospective study was performed.
It was used the preliminary registry of the National System on Basic Information in Health from the Secretary of Health. Discharges with the principal condition CIE-10 U071 and CIE-10 U072 from 2020 were identified in the database [24] to determine the hospital lethality of COVID-19.
The variables reviewed for this study were sex, age group, discharge cause (death and non-death), and the Mexican entity of discharge. Registries with non-specified data were included.
Statistical analysis
Descriptive statistics are presented for the variables of age group, sex, and Mexican entity of discharge. The Chi-Square test was used for the difference in proportions between men and women regarding the discharge cause. The hospital fatality rate of COVID-19 was calculated for overall registries, sex, discharge status, and age groups. For comparing the expected and observed lethality, and among females and males, z tests for proportions were performed.
The alpha value was set at 0.05 to assess statistical significance. The statistical analysis was performed in STATA 13.0’ ® (Stata Corp., College Station, TX, USA).
Results and Discussion
The number of registries included in the analysis was 71,189. From them, 43,786 corresponded to persons discharged for a reason distinct to death, and the remaining 27,403 due to death.
Of the 71,189 discharges, 43,080 (60.51%) were men, 28,103 (39.48%) were women, and 6 (0.01%) did not have a specified sex. Regarding discharges due to death (n = 27,403), the majority occurred in men, with a total of 17,555 (64.06%) deaths, women registered a total of 9,845 (35.93%) deaths and 3 (0.01%) deaths occurred in discharges without specified sex.
According to the chi-squared test result (p <0.05), the sex and discharge are statistically related (Table 1).
Table 1: Distribution by sex and discharge cause in Mexico, 2020
| Men
n % |
Women
n % |
X2, df, P-value | |
| Discharges by death | 17,555 64.07 | 9,845 35.93 | <0.05 |
| Discharged alive | 25,525 58.30 | 18,258 41.70 | – |
| Total discharges | 43,080 | 28,103 | – |
Df Degree of freedom
The age at discharge was analyzed and categorized into five-year age groups. Most discharged persons were between 55-59 years (9,037, which represents 12.69% of the total number of discharges), followed by the group of 50-54 years (8,549, corresponding to 12.01%). Regarding the distribution of discharges due to death, the group of 60-64 years concentrated the highest number of registries (3,739, which represents 13.64%). The subsequent groups, in decreasing order, were the group of 55-59 years (3,614, corresponding to 13.19%); the group of 65-69 years (3,466, corresponding to 12.65%) deaths and the group of 50-54 (3,093, corresponding to 11.29%). Almost half of the discharges due to death corresponded to persons between 50 and 69 years (13,912, which equals 50.77% of the total) (Table 2).
Three of the 32 states of the Mexican Republic concentrated the highest number of discharges. The Mexico state, with 10,025 (14.08%), Mexico City, with 9,697 (13.62%), and Guanajuato, with 6,735 (9.46%). Also, these three states concentrated the highest number of discharges due to death. The Mexico state, with 4,400 (16.06%), Mexico City, with 3,543 (12.93%), and Guanajuato, with 2,212 (8.07%). On the other hand, the three states that concentrated the least number of discharges were Nayarit, with 153 (0.21%), Colima, with 138 (0.19%), and Aguascalientes, with 23 (0.03%). Likewise, these states registered the lowest number of discharges due to death: Colima, with 37 (0.14%), Nayarit, with 20 (0.07%), and Aguascalientes, with 4 (0.01%) (Figure 1).
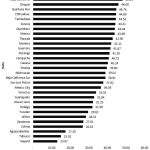 |
Figure 1: Hospital fatality for COVID-19 by Mexican states |
Hospital fatality of COVID-19 in Mexico during 2020
The hospital fatality rate was 38.49%. The hospital fatality calculated for sex was 40.75% for men and 35.03% for women. Therefore, men exceeded the general hospital lethality. Regarding the hospital fatality of COVID-19 by five-year age groups, it stands out that the age groups that range from 55 years to 99 years obtained hospital mortality from COVID-19 higher than the general one (Table 2). A Z test was performed for the hospital fatality proportions in terms of sex, obtaining that the difference in hospital mortality proportions between men and women is statistically significant (p <0.05).
Table 2: Distribution of hospitalized COVID-19 cases, by sex and age groups, in 2020
| Group | Discharge by deaths (n) |
Total discharges (n) |
Hospital fatality (%) |
| Discharge of patients | 27,403 | 71,189 | 38.49 |
| Sex
Men Women Non-specified |
17,555 9,845 3 |
43,080 28,103 6 |
40.75 35.03 50 |
| Age groups (year) Under 1 |
65 | 461 | 14.1 |
| 1 to 4 | 22 | 205 | 10.73 |
| 5 to 9 | 17 | 139 | 12.23 |
| 10 to 14 | 22 | 196 | 11.22 |
| 15 to 19 | 53 | 466 | 11.37 |
| 20 to 24 | 161 | 1,109 | 14.52 |
| 25 to 29 | 315 | 1,928 | 16.34 |
| 30 to 34 | 510 | 2,828 | 18.03 |
| 35 to 39 | 898 | 3,954 | 22.71 |
| 40 to 44 | 1,520 | 5,405 | 28.12 |
| 45 to 49 | 2,418 | 7,443 | 32.49 |
| 50 to 54 | 3,093 | 8,549 | 36.18 |
| 55 to 59 | 3,614 | 9,037 | 39.99 |
| 60 to 64 | 3,739 | 8,416 | 44.43 |
| 65 to 69 | 3,466 | 7,063 | 49.07 |
| 70 to 74 | 2,848 | 5,486 | 51.91 |
| 75 to 79 | 2,137 | 3,993 | 53.52 |
| 80 to 84 | 1,440 | 2,594 | 55.51 |
| 85 to 89 | 762 | 1,347 | 56.57 |
| 90 to 94 | 230 | 423 | 54.37 |
| 95 to 99 | 64 | 110 | 58.18 |
| 100 or more | 5 | 13 | 38.46 |
| Non-specified | 4 | 24 | 16.67 |
Nayarit, Tabasco, and Aguascalientes are among the three states with the lowest hospital fatality due to COVID-19. On the other hand, the Mexican states with the highest hospital fatality due to COVID-19 in 2020 were Coahuila, Puebla, and Baja California (Figure 1).
Of the 32 states of the republic, 19 exceeded the general hospital lethality of the country (38.49%). Puebla and Coahuila were the only two states where hospital lethality from COVID-19 was higher than 50% (Table 3).
Table 3: States with hospital fatality higher than general
| Mexican State | Total discharges (n) | Discharges by death (n) | Hospital fatality
(%) |
| Baja California Sur | 478 | 186 | 38.91 |
| Michoacán | 1,974 | 770 | 39.01 |
| Sinaloa | 1,980 | 788 | 39.80 |
| Oaxaca | 1,173 | 472 | 40.24 |
| Campeche | 663 | 270 | 40.72 |
| Durango | 602 | 248 | 41.20 |
| Guerrero | 1,075 | 448 | 41.67 |
| Morelos | 589 | 248 | 42.11 |
| Tlaxcala | 1,338 | 574 | 42.90 |
| México | 10,025 | 4,400 | 43.89 |
| Querétaro | 1,301 | 573 | 44.04 |
| Sonora | 1,914 | 848 | 44.31 |
| Tamaulipas | 2,349 | 1,046 | 44.53 |
| Chihuahua | 2,430 | 1,086 | 44.69 |
| Quinta Roo | 874 | 391 | 44.74 |
| Chiapas | 437 | 201 | 46.00 |
| Baja California Norte | 2,548 | 1,228 | 48.19 |
| Puebla | 3,717 | 1,977 | 53.19 |
| Coahuila | 930 | 498 | 53.55 |
Regarding the general discharges, most occurred in men, like the reported in the literature, since men have a more severe condition due to COVID-19 25, 26. The same phenomenon is present in older ages where there is a higher possibility of aggravated symptoms and death from COVID-19, a situation observed in the age groups between 50 and 69 years 27.
Mexico state, Mexico City, and Guanajuato concentrated the highest number of discharges, compared to Nayarit, Colima, and Aguascalientes, with the lesser discharge numbers. During the first three months of the pandemic, Mexico state and Mexico City were already listed as states with many cases with COVID-19, while Nayarit and Colima also did so as states with fewer cases 16.
Regarding hospital lethality, Mexico surpassed countries like Italy and France with a hospital lethality of 38.49% against a lethality of 29.7% and 0.174%, respectively 21,28. Compared to the first three months of the pandemic in Mexico, during 2020, the lethality increased from 9.67% to 38.49%. However, it continued to exceed the global lethality, which, according to the WHO, ranges from 0.00% to 1.63% 16,19. It is verified in this and other studies that hospital mortality is higher in males and older ages 22.
It is worth noting that states such as Nayarit, Tabasco, and Aguascalientes, have a fatality rate close to that reported by PAHO after the first three months of the pandemic in Mexico. Comparing these results with the obtained for other states, it is possible an under-registration of discharges due to COVID-19 in those states.
Despite having been two of the states with the highest number of discharges due to SARS-CoV-2, Mexico City and Guanajuato did not exceed general hospital lethality. Maybe the health structure in these two states contributed to the COVID-19 graduates receiving better care and, therefore, a more favorable outcome. In Mexico state was observed a hospital lethality rate higher than the average. Perhaps caused by high attrition of its health personnel and fatal results in graduates, something already hypothesized in the literature, where a higher number of patients was concentrated 21.
Although Puebla and Coahuila were not among the states with the highest number of discharges, they had a high hospital fatality rate. It may be due to management deficiencies of hospitalized patients or an ineffective registry of COVID-19 cases in the other states.
Limitations
Due to the constant actualization of the National System on Basic Information in Health from the Secretary of Health, the statistical analysis was made with preliminary data. Hence, maybe a lower number of discharges was considered, resulting in a lower hospital fatality rate than the real one.
Conclusion
Besides the deaths caused directly by COVID-19 (those that occurred due to respiratory failures), many deaths were indirect in persons with comorbidities exacerbated by this disease. Access to health services, social changes derived from job loss, home protection, and changes in social dynamics, facts expressed in the general mortality excess, cannot be quantified in our study.
Undoubtedly, Mexico has a high hospital fatality rate compared to other countries. Since it is a country with a large territory divided into sovereign states, it is expected that each state has different levels of health system efficiency, and therefore to observe differences in hospital lethality due to the SARS-CoV-2 pandemic. However, there are similar patterns with other persons infected worldwide: this disease is more severe for males and older age subjects.
Author Contributions
CMC: designed the protocol, analyzed the data, and wrote the final report. ELL: participated in designing the protocol, analyzing the data, and writing the final report. CADC: reviewed the data analysis and participated in writing the final report. GFV: reviewed the data analysis and participated in writing the final report. DADM: obtained the database from dynamic cubes and participated in writing the final report. FJMV: reviewed the data extraction and participated in writing the final report. NPR: reviewed the manuscript critically and corrected it. DPS: participated in designing the protocol and analyzed the data.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding Sources
No funding for this research.
References
- Khan M, Adil SF, Alkhathlan HZ, Tahir MN, Saif S, Khan M, et al. COVID-19: A Global Challenge with Old History, Epidemiology and Progress So Far. Molecules. 2020; 26(1):31 https://doi.org/10.3390/molecules26010039
CrossRef - Liu YC, Kuo RL, Shih SR. COVID-19: The first documented coronavirus pandemic in history. Biomed J. 2020; 43(4): 328-333 . https://doi.org/10.1016/j.bj.2020.04.007
CrossRef - Zhou M, Zhang X, Qu J. Coronavirus disease 2019 (COVID-19): a clinical update. Front Med. 2020; 14(2): 126-135. https://doi.org/10.1007/s11684-020-0767-8
CrossRef - CONACYT. COVID-19 México. Gobierno de México. 2021. Available in: https://datos.covid-19.conacyt.mx/
- Ministry of Health. 077. Imported case of coronavirus COVID-19 confirmed in Mexico. 2020. Available in: https://www.gob.mx/salud/prensa/077-se-confirma-en-mexico-caso-importado-de-coronavirus-covid-19
- Xu X, Chen P, Wang J, Feng J, Zhou, H, Li X, et al. Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. Sci China Life Sci. 2020; 63(3): 457-460 https://doi.org/10.1007/s11427-020-1637-5
CrossRef - Dirección General De Salud Pública. Enfermedad por coronavirus, COVID-19. 2021. Available in: https://www.mscbs.gob.es/profesionales/ saludPublica/ ccayes/alertasActual/nCov/documentos/ITCoronavirus.pdf
- World Health Organization. Coronavirus disease (COVID-19). 2020. Available in: https://covid19.who.int/
- Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet. 2020;395(10223): 497-506. doi: https://doi.org/10.1016/S0140-6736(20)30183-5
CrossRef - Mishra SK, Tripathi T. One year update on the COVID-19 pandemic: Where are we now? Acta Tropica,2021;214: 105778. doi: https://doi.org/10.1016/j.actatropica.2020.105778
CrossRef - Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109:102433. doi: https://doi.org/10.1016/j.jaut.2020.102433
CrossRef - Izcovich A, Ragusa MA, Tortosa F, Lavena Marzio MA, Agnoletti C, et al. Prognostic factors for severity and mortality in patients infected with COVID-19: A systematic review. PLOS ONE. 2020, 15(11). https://doi.org/10.1371/journal.pone.0241955
CrossRef - Medeiros de Figueiredo A, Daponte A, Moreira Marculino de Figueiredo DC, Gil-García E, Kalache A. Letalidad de la COVID-19: ausencia de patrón epidemiológico. Gaceta Sanitaria. 2021; 35(4);355-357. https://doi.org/10.1016/j.gaceta.2020.04.001
CrossRef - Moreno-Altamirano A, López-Moreno S, Corcho-Berdugo A. Principales medidas en epidemiología. Salud Pública de México. 2000; 42(4): 337-348. Available in: https://www.redalyc.org/pdf/2232/223219928011.pdf
CrossRef - Mexican Goverment. Grupo Interinstitucional Para La Estimación Del Exceso De Mortalidad Por Todas Las Causas. Boletín estadístico sobre el exceso de mortalidad por todas las causas durante la emergencia por COVID-19. 2020. Available in: https://coronavirus.gob.mx/wp-content/uploads/2020/11/Boletin_VI_Exceso_Mortalidad_SE43_MX.pdf
- Suárez V, Suarez-Quezada M, Oros- Ruiz S, Ronquillo De Jesús E. Epidemiología de COVID-19 en México: del 27 de febrero al 30 de abril de 2020. Revista Clínica Española. 2020; 220(8): 463-471. https://doi.org/10.1016/j.rce.2020.05.007
CrossRef - PanAmerican Health Organization. Módulo de Principios de Epidemiología para el Control de Enfermedades (MOPECE). 2ª ed, Washington, USA; Organización Panamericana de la Salud; 2011. Available in: https://www.paho.org/col/dmdocuments/MOPECE1.pdf
- PanAmerican Health Organization. Codificación del COVID-19 con la CIE-10. 2020. Available: https://www.paho.org/arg/dmdocuments/2019-ncov-1/documentos/COVID-19-CIE-codigos-2020-03-25-spa.pdf
- Ioannidis JPA. Infection fatality rate of COVID-19 inferred from seroprevalence data. Bull World Health Organ. 2021;99:19–33F. doi: http://dx.doi.org/10.2471/BLT.20.265892
CrossRef - Acosta LD. (2020). Response capacity to the COVID-19 pandemic in Latin America and the Caribbean. Rev Panam Salud Pública. 2020; 44:E109. doi: https://doi.org/10.26633/RPSP.2020.109
CrossRef - Souris M, Gonzalez JP. (2020). COVID-19: Spatial analysis of hospital case-fatality rate in France. PLoS ONE. 2020; 15(12): e0243606. doi: https://doi.org/10.1371/journal.pone.0243606
CrossRef - Bellan M, Patti G, Hayden E, Azzolina D, Pirisi M, Acquaviva A, et al. Fatality rate and predictors of mortality in an Italian cohort of hospitalized COVID-19 patients. Sci Rep. 2020; 10(1): 20731. doi: https://doi.org/10.1038/s41598-020-77698-4
CrossRef - Ñamendys-Silva SA. Case fatality ratio of COVID-19 patients requiring invasive mechanical ventilation in Mexico: an analysis of nationwide data. Crit Care. 2021: 25(1):68. doi: https://doi.org/10.1186/s13054-021-03485-w
CrossRef - Sistema Nacional de Información Básica en Materia de Salud. Secretaría de Salud. Egresos hospitalario s 2020. Available in: http://sinba08.salud.gob.mx/cubos/cubosaeh2020_plataforma.htm
- Mohamed SM, Moulin TC, Schiöth HB. Sex differences in COVID-19: the role of androgens in disease severity and progression. Endocrine. 2021;71(1):3-8. doi: https://doi.org/10.1007/s12020-020-02536-6
CrossRef - Takahashi T, Ellingson MK, Wong P, Israelow B, Lucas C, Klein J, et al. Sex differences in immune responses that underlie COVID-19 disease outcomes. Nature. 2020; 588(7837):315-320. doi: https://doi.org/10.1038/s41586-020-2700-3
CrossRef - Gallo Marin B, Aghagoli G, Lavine K, Yang L, Siff EJ, Chiang SS, et al. Predictors of COVID-19 severity: A literature review. Rev Med Virol. 2021;31(1):1-10. doi: https://doi.org/10.1002/rmv.2146
CrossRef - 28 Levin AT, Hanage WP, Owusu-Boaitey N, Cochran KB, Walsh SP, Meyerowitz-Katz G. Assessing the age specificity of infection fatality rates for COVID-19: systematic review, meta-analysis, and public policy implications. Eur J Epidemiol. 2020;35(12):1123-1138. doi: https://doi.org/10.1007/s10654-020-00698-1
CrossRef







