Manuscript accepted on :26-07-2021
Published online on: 02-08-2021
Plagiarism Check: Yes
Reviewed by: Dr. Sana Tanzil
Second Review by: Dr. Ankur Singh Bist
Final Approval by: Dr. Fai Poon
Lalita BT1 , Yuvaraj Maria Francis2*
, Yuvaraj Maria Francis2* , Balaji K2
, Balaji K2 , Gunapriya Raghunath2
, Gunapriya Raghunath2  and Kumaresan M2
and Kumaresan M2
1Saveetha Medical College and Hospital, Thandalam, Chennai, India- 602105.
2Department of Anatomy, Saveetha Medical College and Hospital, Thandalam, Chennai, India- 602105.
Corresponding Author E-mail: sujinalways@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2222
Abstract
The lower end of humerus has numerous fossae which play a significant role during extreme movements. Coronoid fossa and olecranon fossa are separated by a delicate supratrochlear septum; occasionally septum has perforation and form an aperture, named as Supratrochlear foramen (STF). The knowledge of this foramen will be beneficial for anatomists, anthropologists, orthopedic surgeons, and radiologists. The aim of the present study was to establish the prevalence and morphometry of STF of the humerus in South Indian population and to correlate with the previous studies. The present prospective study was carried out with 274 (146 left sided + 127 right sided) dried humeri of unknown sex and age. The distal humeri were examined for the presence of STF, morphometry such as diverse shapes, vertical and horizontal diameters, and distance from STF to medial, lateral epicondyle and also to the inferior margin of trochlea using digital vernier caliper. In the present study, out of 274 dried humeri, 69 showed presence of STF, 163 were translucent and 42 were opaque. The prevalence of STF was 25.18%. After keen observation, shapes of the STF were categorized accordingly. The oval (42%) showed higher percentage whereas the other shapes showed as follows: - irregular (12%), round (19%), rectangular (12%), reniform (9.7%), sieve (7.3%) and triangular (2%). The mean vertical and transverse diameters of STF on the right side were 3.12 ± 1.09 and 5.5 ± 1.83mm and on the left side, it was 3.47± 1.32 and 4.9± 1.5mm respectively. The mean distance from STF to medial and lateral epicondyle on the right side was 25.12± 3.1 and 28.09± 2.3mm and for the left side 24.97± 2.9mm and 27.16± 2.4mm respectively. The anatomical knowledge regarding the supratrochlear foramen is much promising for the orthopaedic surgeons during intramedullary nailing for supracondylar fracture of humerus. STF appears as a radiolucent area in radiographs, which may pose a difficulty for the radiologist in differentiating it from an osteolytic or cystic lesion. In addition, STF is predominantly found in the primates, it may act an evolutionary link between the humans and lower animals.
Keywords
Anatomist; Anthropologist; Humerus; Intramedullary nailing; Orthopaedicians; Radiologist; Supra-trochlear foramen; Supracondylar fractures
Download this article as:| Copy the following to cite this article: Lalita B. T, Francis Y. M. Balaji K, Raghunath G, Kumaresan M. A Comprehensive Study on Supratrochlear Foramen of Human Humerus and its Clinical Significance - A Review. Biomed Pharmacol J 2021;14(3). |
| Copy the following to cite this URL: Lalita B. T, Francis Y. M. Balaji K, Raghunath G, Kumaresan M. A Comprehensive Study on Supratrochlear Foramen of Human Humerus and its Clinical Significance - A Review. Biomed Pharmacol J 2021;14(3). Available from: https://bit.ly/3xk1mJJ |
Introduction
The supratrochlear foramen (STF) is a significant and relatively atypical anatomical variation noticed in the distal end of humerus and this variation has not been given due significance in standard textbooks of anatomy and orthopedics. Generally, foramen transmits blood vessels and nerves, in the case of STF, no significant structure is transmitted and in the rare case, there may be a probability of entry of the median nerve, which may produce symptoms such as pain and weakness in the hand 1. A delicate plate of compact bone known as supratrochlear septum (STS) varying from 0.7 mm to 1.2 cm in thickness, lined by a synovial membrane of the elbow joint, partitioned the ventrally placed coronoid fossae and dorsally placed olecranon fossae. This translucent or opaque septum may consist of enormous perforations and in extreme cases, it may be perforated to form a narrow orifice known as ‘supratrochlear orifice’ or ‘supratrochlear foramen’ [2, 3]. The first person to establish the STF was Mekel in 1825 and it was also frequently named as epitrochlear, intercondylar, coronoid, and olecranon foramen [4-6]. The STF is in various shapes and their morphometry varies in different gender and races. The delicate and translucent STS is not observed in newborn and begins to appear in the latter period of life, persists until the age of seven years and later due to various reasons, STS undergoes degeneration or absorption only in some individuals and may lead to the formation of STF [7, 8]. The presence of STF is not only observed in humans but also in lower animals such as apes, dogs, hyenas, and other primates. The presence of STF in individuals and primates results in hyperextension of the elbow joint during various activities in day to day life [9, 10]. The presence of STF in humans indicates that they are evolved from primates as proved by various theories [11]. The formation of STF could be due to changes that occur at the molecular level and the gene responsible is T-Box5 (TBX). The genes of these family regulate the genesis of proteins known as TBX proteins, plays a significant role in the genesis of various parts of the upper limb and pumping organ in the womb [12]. The STF is considered to be a negligible feature of the humerus in the early days due to unidentified reasons. The supratrochlear fracture is one of the frequently occurring fractures among children [13]. The orthopedic surgeons usually perform a reduction procedure to correct supracondylar fracture through intramedullary nailing, which may be compromised due to the existence of STF. The retrograde intramedullary nailing is done either through the medial and lateral epicondyles of the humerus or only through the lateral epicondyle. Therefore ruling out the presence of STF is of utmost importance before planning the intramedullary nailing of supracondylar fractures of the humerus [14]. During radiological evaluations of the distal end of humerus, the existence of STF may result in spurious interpretation as pathological lesions or cysts [15]. Therefore, this study aims to scrutinize the prevalence, incidence, morphology, and morphometry of supratrochlear foramen among the South Indian population. The comprehensive knowledge regarding STF will be worthwhile for anthropologists to trace the evolutionary changes between humans and primates, anatomists while teaching, orthopedic surgeons during pre-operative procedures and radiologists during interpretation.
Materials and methods
This study was carried out after obtaining proper Institutional ethical clearance (SMC/IEC/2020/03/135). A prospective study was carried out on 274 dried humeri from South Indian population including 146 left-sided and 127 right-sided of unknown age, sex and free from bony pathology, obtained from the Department of Anatomy, Saveetha Medical College and Hospital, Thandalam Chennai, India. The study was carried out for 6 months from January to June 2020. The following parameters were observed such as the presence and morphometry of STF. The various morphometric parameters were measured using a digital vernier caliper and the data obtained were analyzed statistically.
Results
The results of this study were narrated in a stepwise manner of various parameters observed in the study.
Presence of STF
Out of 274 dried humeri, STF was observed in 69 bones, among which 32 were noticed on the right side and 37 were on the left side. 42 showed opaque, among which 19 were
on right and 23 were on left side and the remaining 163 were translucent septa, in which 65 were on right and 98 were on left side.
Shapes of STF
The shapes of STF are categorized into irregular, oval, round, rectangular, reniform, sieve, and triangular. In the present study almost all shapes were observed. Among all, oval was predominantly observed with 42% and the least was triangular 2%, remaining shapes were 19% round, 9.7% reniform, 8% rectangular, 12% irregular and 7.3% were a sieve. The diverse shapes observed in the study were expressed in figure: 1.
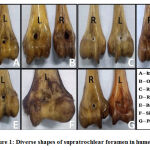 |
Figure 1: Diverse shapes of supratrochlear foramen in humerus. |
Vertical diameter of STF
The mean and standard deviation of vertical diameter of STF on the right side was 3.12 ± 1.09 and 3.47 ± 1.32mm on the left side were observed. Nominal variations were observed when we compare with various shapes.
The transverse diameter of STF
The mean and standard deviation of transverse diameter of STF on the right side was 5.45 ± 1.83 and 4.9 ± 1.51 mm on the left side were observed. Nominal variations were observed when we compare with various shapes.
Distance from Medial epicondyle to STF
The distance was measured from the center of STF to the medial margin of the medial epicondyle. The mean distance from the medial epicondyle to the center of STF on the right side was 25. 12 ± 3.1mm and on the left side was 24.97 ± 2.9 mm.
Distance from Lateral epicondyle to STF
The distance was measured from the center of STF to the lateral margin of the lateral epicondyle. The mean distance from the lateral epicondyle to the center of STF on the right side was 28. 09 ± 2.3 mm and on the left side were 27.16 ± 2.4 mm.
Distance from Trochlea to STF
The distance was measured from the center of STF to the inferior margin of the trochlea. The mean distance from the inferior margin of the trochlea to the center of STF on the right side was 15.07 ± 1.78 mm and on the left side was 14.97 ± 1.62mm. The various morphometry analyzed in the study were expressed in figure: 2.
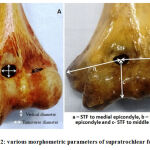 |
Figure 2: various morphometric parameters of supratrochlear foramen. |
Discussion
The distal end of the humerus has medial and lateral epicondyles for the origin of flexor and extensor groups of muscles of the forearm. They have three fossae namely the radial fossa, olecranon fossa, and coronoid fossa, and articulate with the radius and ulna to form elbow-joint16. The lower end of the humerus plays a crucial role in orthopedic treatment during pre-operative planning for supracondylar fracture and also in anthropologists to identify the evolution of humans from the primates17, 18. The bones of humans and lower animals have various foramina for the transmission of neurovascular structures but in case of STF no such significant structure is passing, hence it does not qualify to be one by definition. The STF in lower animals transmitted the brachial artery and median nerve and in a study conducted by Erdogmus S explained that passage of the median nerve produces pain and weakness in the hand.
Theories in the Formation of STF
There are various theories recommended regarding the development of STF both in humans and lower animals.
According to Glanville EV, the STF is formed as a result of articulations between the humerus and ulna during extremes of flexion and extension and mainly comes under mechanical theory. The presence of STF, therefore, can be attributed to the physiological genesis of the elbow joint and its diverse shapes to the morphometry of the articulating surfaces19.
According to Koyun N, the genesis of STF is mainly due to an inherited trait 20
According to Sunday.OO the prehistoric ancestors were used to undergo cumbersome activities such as cultivation and carrying heavy tools for their basic needs. The intermittent pressure of processes of the ulna gradually results in the absorption of the STS between them and results in the genesis of STF 21.
According to Chapman DL, the pressure from the olecranon process may act as a strengthening factor but in the later period of life, the inadequate blood flow to STS results in deterioration and leads to the genesis of STF foramen formation and literature proved that the STS was not present in the embryonic life, but develops after seven years of postnatal life due to reduced blood flow22.
Prevalence of STF
The prevalence of STF varies in different population mainly due to genetic factor and day to day activities they undergo. The formation of STF is predominantly observed in females compared with males [23]. Similarly, the STF observation was predominant in the non-dominant left side when compared to the right side. The reason is right side bones are robust and gracile in nature [24-28]. The prevalence of STF in the present study is about 25.18%. The STF prevalence in the human population varies from 0.3% to almost 60% worldwide and is drafted in Table 1.
According to Macalister, a study conducted among Libyans showed a STF prevalence of 57% [29]. Prevalence of STS is high among Arkans Indians 52% and low in the Greek population 1% [30]. There is no obvious cause, the communication noticed between the olecranon and coronoid fossa seems to be an unusual congenital irregularity. Congenital anomalies of bilateral occurrence might reflect the presence of a particular, though very rare genetic defect, since an Online Mendelian Inheritance in Man (OMIM) database search did not divulge any disorder with a clinical evaluation corresponding to lower part of upper extremity communication. Such a congenital anomaly could be due to an enormous growth of olecranon or coronoid process, or it could be pertinent to collagen fibers elasticity leading to flail joints. Flail joints generally hyperextend and may produce erosion of the delicate STS between the fossae.
Lamb et al observed that the prevalence of STF is predominantly observed in the left side comparated to the right side especially in ancient people and adolescents [31]. Similarly, in the present study, the prevalence of STS was recognized high on the left side than the right side. These results were compared with the previous studies and were documented in (Table: 1) many studies.
Table 1: Prevalence of Supratrochlear foramen in various populations.
| Author | Population | Prevalence % |
| Agarwal et al, (2018) [31] | North Indians | 22.96 |
| Akabori et al, (1934) [32] | Koreans | 11 |
| Akabori et al, (1934) [32] | Ainus | 8.8 |
| Akabori et al, (1934) [32] | Japenese | 18.1 |
| Arunkumar et al, (2015) [33] | South Indian | 21.4 |
| Abo Sablan et al, (2020) [34] | Kurdish | 25.81 |
| Ananthi et al, (2011) [35] | South Indians | 31.3 |
| Benfer et al, (1968) [10] | American | 6.9 |
| Bashi et al, (2019) [36] | Turkey | 20.37 |
| Bradshaw et al, (2019) [37] | Portuguese | 16.18 |
| Bokhari et al, (2018) [38] | Lahore | 17 |
| Bhanu and Sankar, (2012) [3] | South Indians | 30.58 |
| Chatterjee, (1968) [39] | Eastern Indians | 27.4 |
| Chagas et al, (2016) [40] | Brazil | 22.5 |
| Çimen et al, (2003) [41] | Turks | 12 |
| Dang et al, (2016) [42] | North Indian | 30 |
| Deshmukh et al (2018) [43] | South Indian | 16.3 |
| Diwan et al (2013) [25] | North Indian | 24.1 |
| Erdogmus et al (2014) [17] | Turkish | 10.8 |
| Glanville et al, (1967) [19] | Africans | 47 |
| Glanville et al, (1967) [19] | Europeans | 6 |
| Hirsh et al, (1927) ) [7] | White Americans | 4.2 |
| Hirsh et al, (1927) [7] | African Americans | 21.7 |
| Hirsh et al, (1927) ) [7] | Native Americans (Arkansas) | 58 |
| Hrdlicka et al, (1932) [44] | Australians | 46.5 |
| Hrdlicka et al, (1932) [44] | Italians | 9.4 |
| Hrdlicka et al, (1932) [44] | Germans | 8.8 |
| Jadhav et al, (2015) [45] | North Indians | 34.68 |
| Jagdish et al, (2017) [46] | North Indians | 27.3 |
| Joshi et al, (2016) [47] | Western Indian | 35.88 |
| Kate and Dubey et al, (1970) [48] | Central Indians | 32 |
| Krishnamurthy et al, (2011) [49] | Indians (Telangana ) | 23 |
| Krishnamurthy et al, (2011) [49] | Mexicans | 38.7 |
| Krishnamurthy et al, (2011) [49] | Eskimos | 18.4 |
| Kumar et al, (2015) [5] | South Indian | 26 |
| Koyun et al, (2011) [20] | Turkish | 8.6 |
| Li et al, (2015) [50] | Jining | 10.3 |
| Macalister et al, (1990) [29] | Libyans | 57 |
| Mathew et al, (2016) [27] | Indians (Kerala) | 24.59 |
| Ming-Tzu, (1935) [51] | Chinese | 17.5 |
| Mayuri et al, (2013) [52] | North Indians | 40.78 |
| Mallikarjun et al, (2020) [53] | South Indians | 32 |
| Nayak et al, (2009) [54] | Indians | 34.4 |
| Naqshi et al, (2014) [55] | North Indians | 27.5 |
| Nodu et al, (2012) [6] | South Africans | 32.5 |
| Ozturk et al, (2000) [56] | Egyptians | 7.9 |
| Patel et al, (2013) [57] | South Indians | 23.5 |
| Papaloucas et al, (2011) [58] | Greeks | 0.304 |
| Paraskevas et al, (2010) [23] | Greeks | 11.7 |
| Raghavendra et al, (2014) [59] | South Indians | 19.2 |
| Ramamurthi (2016) [60] | South Indians | 23.7 |
| Rao et al, (2018) [11] | South Indian | 11.7 |
| Singh (1972) [24] | North Indians | 27.5 |
| Singhal and Rao et al, (2007) [11] | South Indians | 28 |
| Sathish and suresh (2019) [61] | South Indians | 19.2 |
| Shivaleela et al, (2016) [28] | South Indians | 26.7 |
| Sangeetha et al, (2017) [62] | North Indians | 30.5 |
| Sunday et al, (2014) [21] | Nigerian | 27.7 |
| Veerapan et al, (2013) [63] | South Indians | 19.17 |
| Present study | South Indians | 25.18 |
Morphometry of STF
Shape of STS
The shapes of STF are classified into an irregular, oval, round, rectangular, reniform, sieve, and triangular [52, 63]. The formation of the diverse shape of STF may depend upon the level of degradation, mechanical activity, and differences in race. As per the literature report, the commonest shape is oval and the least common is a sieve. The remaining shape varies according to different races and depending on the level of absorption. Inconsistent with the previous studies, our studies also showed a higher incidence of oval shape with 52 %, triangular 2 %, round 19% , reniform 9.7%, irregular 10% and 7.3% were a sieve. These results obtained in this study were compared with the previous literature and they were expressed in (Table: 2).
Table 2: Evaluation of various shapes of supratrochlear foramen in correlation with previous literature.
| Author | Prevalence of various shape of supratrochlear foramen in percentage | ||||||
| Irregular | Oval | Round | Reniform | Rectangular | Sieve | Triangular | |
| Arunkumar et al, (2015) [33] | 93.42 | 2.63 | 3.94 | ||||
| Agrawal et al, (2018) [31] | 61.29 | 32.25 | |||||
| Bahsi (2019) [36] | 32.36 | 61.93 | 5.36 | ||||
| Bokhari et al (2018) [38] | 14.7 | 54.88 | 14.7 | 11.76 | 2.94 | ||
| Bhanu and Sankar (2012) [3] | 70.27 | 29.72 | |||||
| Burute et al. (2016) [64] | 56.68 | 16.66 | 26.66 | ||||
| Diwan et al. (2013) [25] | 82.47 | 10.51 | 2.33 | ||||
| Deshmukh et al, (2018) [43] | 45 | 50 | 5 | ||||
| Dang et al. (2016) [42] | 40 | 60 | |||||
| Erdogmus et al, (2014) [17] | 72.22 | 11.11 | 6.5 | 11.11 | |||
| Joshi et al. (2016) [47] | 65.57 | 21.31 | 9.83 | 3.27 | |||
| Jadhav and Zambare (2015) [45] | 7.79 | 67.53 | 16.88 | ||||
| Jagdish et al, (2017) [46] | 36.66 | 63.33 | |||||
| Kumar et al. (2015) [2] | 78.94 | 8.77 | 3.5 | 3.5 | |||
| Kumarasamy et al. (2011) [15] | 82 | 18 | |||||
| Li et al (2015) [50] | 70.37 | 14.81 | 7.40 | 7.40 | |||
| Mayuri et al. (2013) [52] | 48.38 | 41.93 | 3.22 | 6.45 | |||
| Mallikarjun et al, (2020) [53] | 43.75 | 7.81 | 4.68 | 18.75 | 9.35 | 12.5 | |
| Mathew et al. (2016) [27] | 51.6 | 21.6 | 11.6 | 1.6 | 8.3 | 5 | |
| Naqshi et al. (2014) [55] | 90.9 | 9.09 | |||||
| Nayak et al. (2009) [54] | 91.79 | 5.22 | 1.49 | ||||
| Öztürk et al. (2000) [56] | |||||||
| Patel et al. (2013) [57] | 93.98 | 4.51 | 1.5 | ||||
| Rao et al, (2018) [11] | 5.88 | 76.47 | 11.76 | 5.88 | |||
| Raghavendra et al, (2014) [59] | 85.71 | 14.28 | |||||
| Sathish and suresh (2019) [61] | 46.70 | 33.30 | 20 | ||||
| Singhal and Rao (2007) [11] | |||||||
| Sunday et al, (2014) [21] | 55.55 | 22.22 | 11.11 | 11.11 | |||
| Shivaleela et al. (2016) [28] | 10.53 | 42.11 | 47.37 | ||||
| Savitha and Dakshayani (2016) [14] | 28 | 35.71 | 21.42 | 7.14 | |||
| Veerapan et al, (2013) [63] | 42.85 | 35.71 | 7.14 | 14.28 | |||
| Present study | 12 | 42 | 19 | 9.7 | 8 | 7.3 | 2 |
Vertical and transverse diameter of STF
In this study, the mean transverse diameter of the STF was 5.45mm on right side and 4.9 mm, on the left side. Similarly, the mean vertical diameter of STS on the right side was 3.12mm and on the left side, it was 3.47mm. The results obtained in the study were consistent with a study conducted by Vishwajit et al[43], Mathew et al[27], Nayak et al [54], Krishnamurthy et al [49], and Veerappan et al[63]. The results of the present study were compared with the previous literature and they were expressed in the (Table: 3). The vertical and transverse diameters of the STF varies according to the shape, absorption, and vascular insufficiency of the distal end of the humerus. The perception of these dimensions of STF in the lower end of the humerus may help to reduce the misinterpretation of radiological images.
Table 3: Evaluation of vertical and transverse diameters of supratrochlear foramen in correlation with previous literature.
| Author | Vertical diameter of STF | Transverse diameter of STF | ||
| Right | Left | Right | Left | |
| Arunkumar et al (2015) [33] | 3.9 ± 1.32 | 3.84 ± 1.20 | 5.67 ± 1.71 | 5.39 ± 1.57 |
| Agarwal et al, (2018) [31] | 4.88 ± 0.69 | 4.16 ± 0.67 | 6.35 ± 1.57 | 6.49 ± 1.37 |
| Bahsi (2019) [36] | 4.81±1.38 | 4.82±1.33 | 6.55±2.84 | 5.64±1.96 |
| Bokhari (2018) [38] | 3.8 ± 1.24 | 3.2 ± 1.19 | 5.2 ± 2.69 | 4.9 ± 2.75 |
| Bhanu and Sankar, (2012) [3] | 5.75±1.5 | 4.86±1.2 | 6.68±0.8 | 6.92±2.0 |
| Chagas et al (2016) [40] | 2.778±2.197 | 2.779±2.050 | 2.365±1.396 | 2.332±1.23 |
| Dang et al (2016) [42] | 3.79 ±0.68 | 3.94 ±1.40 | 5.14 ±1.165 | 5.21 ±2.13 |
| Deshmukh et al (2018) [43] | 4.2 ± 3.1 | 4.3±1.7 | 5.3±2.7 | 6.7±2.3 |
| Erdogmus et al (2014) [17] | 2.72 ± 0.0 | 4.26 ± 0.0 | 6.52 ± 0.0 | 6.7 ± 2.2 |
| Joshi et al (2016) ) [47] | 3.75 ±1.48 | 4.68 ±1.43 | 5.5 ±2.89 | 6.48 ±2.47 |
| Jagdish et al (2017) [46] | 3.77±0.62 | 3.87±1.40 | 5.16±1.169 | 5.20±2.14 |
| Krishnamurthy et al (2011) [49] | 4.7 ± 1.69 | 4 ± 1.52 | 5.26 ± 2.47 | 6.5 ± 2.59 |
| Kumar et al (2015) [5] | 4.64 ±2.45 | 4.76 ± 2.64 | 5.76 ±2.22 | 6.36 ± 2.88 |
| Mathew et al (2016) [27] | 3.82 ± 1.07 | 3.37 ± 1.25 | 5.24 ± 1.76 | 4.88 ± 1.63 |
| Mahitha et al (2016) [65] | 3.4 ± 1.24 | 4.2 ± 0.75 | 4.6 ± 1.76 | 6.2 ± 2.12 |
| Nayak et al. (2009) [54] | 3.81 ± 0.97 | 4.85 ± 1.64 | 5.99 ± 1.47 | 6.55 ± 2.47 |
| Naqshi et al (2015) [55] | 3.9 ± 1.32 | 4.6 ± 1.63 | 5.3 ± 2.37 | 6.6 ± 2.53 |
| Patel et al (2013) [57] | 4.77 ± 1.15 | 4.90 ± 1.68 | 7.31 ± 1.77 | 7.03 ± 1.49 |
| Raghavendra et al (2014) [59] | 3.9±1.4 | 4.7±1.6 | 5.1± 2.4 | 6.5±2.5 |
| Rao et al (2018) [11] | 5.4 ± 1.52 | 5.3 ± 2.00 | 8.1 ± 1.88 | 7.25 ± 2.78 |
| Ramamurthi KS (2016) [60] | 4.3 ±1.6 | 4.9 ±1.5 | 5.3± 2.2 | 6.8 ±2.3 |
| Sathish and Suresh (2019) [61] | 3.94 ± 1.3 | 3.82 ± 1.03 | 5.82 ± 1.52 | 5.46 ± 2.5 |
| Shivaleela C et al (2016) [28] | 3.88±2.39 | 3.68±3.53 | 4.50±3.18 | 3.32±3.22 |
| Sunday et al, (2014) [21] | (3.33 ± 1.04 | 5.00 ± 2.40 | 4.95 ± 1.02 | 6.82 ± 2.92 |
| Veerappan et al (2013) [63] | 4.09±1.13 | 5.35±1.60 | 8.30 ± 1.07 | 7.53±1.28 |
| Present study | 3.12 ±1.09 | 3.47±1.32 | 5.45±1.83 | 4.9±1.51 |
Distance from center of STS to Medial epicondyle, Lateral epicondyle, and Trochlea
In the present study, the average distance from the center of STF to the medial epicondyle on the right side was 25. 12 ± 3.1mm and on the left side was 24.97 ± 2.9 mm. Similarly, the distance measured from the center of STF to the lateral epicondyle was on the right side 28. 09 ± 2.3 mm and on the left side was 27.16 ± 2.4 mm. These results were correlated with previous studies conducted by Li et al [50], Zahra et al [38], Sathish et al [61], Mathew et al[27]. The data were compared with the previous reports and revealed in (Table: 4).
Table 4: Evaluation of distance from supratrochlear foramen to medial and lateral epicondyles in correlation with previous literature.
| Author | STF to Medial epicondyle | STF to Lateral epicondyle | ||
| Right | Left | Right | Left | |
| Bahsi (2019) ) [36] | 25.00±3.07 | 24.73±3.04 | 26.19±2.64 | 26.91±1.97 |
| Bokhari et al (2018) [38] | 21.7+ 0.45 | 25.3+ 0.24 | 27.4+ 3.0 | 26.2+ 2.8 |
| Deshmukh et al (2018) [43] | 24.1 ±2.2 | 23.7± 2.4 | 16.9 ±5.5 | 24.3± 2.2 |
| Erdogmus et al (2014) [17] | 24.70±1.95 | 23.93±2.65 | 26.65±0.68 | 26.92±1.28 |
| Joshi et al (2016) [47] | 24.7±3.3 | 25.2±3.2 | 24.7±1.9 | 25.7±2.7 |
| Mathew et al (2016) [27] | 24.91±2.93 | 24.39±3.15 | 27.2±2.95 | 26.92±2.46 |
| Satish and Suresh (2019) [61] | 23.84±2.73 | 24.06±2.93 | ||
| Sunday et al, (2014) [21] | 26.30 ± 2.07 | 25.82 ± 2.75 | ||
| Present study | 25.12±3.1 | 24.97±2.9 | 28.09±2.3 | 27.16±2.4 |
The distance from the center of STF to the inferior margin of the trochlea was measured in this study and the mean was 15.07 ± 1.78 mm on right side and on the left side 14.97 ± 1.62mm. The present study was consistently correlated with Mathew et al [27]. The knowledge regarding such distances will be very much useful for the surgeons who perform retrograde intramedullary nailing for fractures that occur in the lower end of the humerus and also it will be useful for the radiologist to prevent the misinterpretation of the lower end of the humerus. According to De Wilde et al STF is a relatively radiolucent area, frequently named “Pseudo lesion” in a radiograph of the upper extremity, and can be erroneous as an osteolytic or cystic lesion66.
Conclusion
The STF is a skeletal variation observed in the distal end of humerus, knowledge regarding this variation will be significant to the anatomists in academics, forensic experts in medicolegal investigations, and anthropologists can use it as a reliable tool to establish a relationship between humans and primates. The presence of STF is important for the orthopedic surgeon for preoperative planning in supracondylar fractures and to choose an ideal intramedullary nail. The radiologist will also find it beneficial during the interpretation of radiographs and CT scans of the lower end of the humerus as it helps in differentiating from an osteolytic or cystic lesion.
Acknowledgement
I like thank the Professor and head of Department of Anatomy to carry out the research.
Conflicts of Interest
The authors don’t have any conflict of interest.
Funding Source
There are no funding source for this artical.
References
- Roaf R. Foramen in the humerus is caused by the median nerve. The Journal of Bone and Joint Surgery. 1957; 39B (4): 748–4.
CrossRef - Kumar U, Sukumar C, Sirisha V, Rajesh V, Murali Krishna S, Kalpana T. Morphologic and Morphometric Study of Supra Trochlear Foramen of Dried Human Humeri Of Telangana Region. Int J Cur Res Rev 2015; 7: 95-8.
- Bhanu PS, Sankar KD: Anatomical note of supratrochlear foramen of the humerus in the south coastal population of Andhra Pradesh. Narayana Medical Journal, 2012; 1(2): 28–34.
- Meckel JH (1825), Cited by Kate BR, Dubey PN. A note on the septal apertures in the humerus of Central Indians. Eastern Anthropologist.1970; 33:105-10.
- Das S: Supratrochlear foramen of the humerus. Anat Sci Int, 2008; 83(2): 120.
CrossRef - Ndou R, Smith P, Gemmell R, et al: The supratrochlear foramen of the humerus in a South African dry bone sample. Clin Anat, 2013; 26(7): 870–74.
CrossRef - Hirsh IS. The supratrochlear foramen: clinical and anthropological considerations. Am J Surg 1927; 2: 500-5.
- Morton HS, Crysler WE. Osteochondritis dissecans of the supratrochlear septum. J Bone Joint Surg Am 1945; 27:12-24.
- Haziroglu RM, Ozer M. A supratrochlear foramen in the humerus of cattle. Anat Histol Embryol 1990; 19:106-8.
CrossRef - Benfer RA, Tappen NC. The occurrence of the septal perforation of the humerus in three non-human primate species. Am J Phys Anthropol 1968; 29:19-28.
CrossRef - Singhal S, Rao V. Supratrochlear foramen of the humerus. Anat Sci Int 2007; 82:105-7.
CrossRef - Chapman DL, Garvey N, Hancock S, Alexiou M, Agulnik SI, Gibson-Brown JJ, Cebra-Thomas J, Bollag RJ, Silver LM, Papaioannou VE. Expression of the T-box family genes, Tbx1-Tbx5, during early mouse development. Dev Dyn 1996; 206:379-90.
CrossRef - Nick Pilla, John Rinaldi, Mark Hatch, and William Hennrikus, Epidemiological Analysis of Displaced Supracondylar Fractures. Cureus. 2020 Apr; 12(4): e7734.
CrossRef - Savitha V, Dakshayani K. Study of the supratrochlear foramen of the humerus. Int J Anat Res 2016; 4: 2979-83.
CrossRef - Kumarasamy SA, Subramanian M, Gnanasundaram V, Subramanian A, Ramalingam R. Study of intercondyloid foramen of humerus. Rev Arg de Anat Clin 2011; 3: 32-6.
CrossRef - Susan Stranding, Gray’s Anatomy: The Anatomical basis of clinical practice, Elsevier, London, UK, 40 the edition.
- Erdogmus S, Guler M, Eroglu S, Duran N. The importance of the supratrochlear foramen of the humerus in humans: an anatomical study. Med Sci Monit 2014; 20: 2643.
CrossRef - Brauer CA, Lee BM, Bae DS, Waters PM, Kocher MS. A systematic review of medial and lateral entry pinning versus lateral entry pinning for supracondylar fractures of the humerus. J Pediatr Orthop. 2007; 27:1816.
CrossRef - Glanville EV. Perforation of the coronoid-olecranon septum humeroulnar relationships in the Netherlands and African populations. Am J Phys Anthropol.1967; 26:85-92.
CrossRef - Koyun N, Aydinlioglu A, Gumrukcuoglu FN. Aperture in coronoid-olecranon septum: A radiological evaluation. Indian J Orthop. 2011; 45:392-95.
CrossRef - Sunday OO, Olusegun OS, Oluwabunmi BM. The Supratrochlear Foramen of the Humerus: Implications for Intramedullary nailing in the distal humerus. Journal of Biology, Agriculture, and Healthcare. 2014; 4(7): 2224-32.
- Chapman DL, Garvey N, Hancock S, Alexiou M, Agulnik SI, Gibson-Brown JJ, Cebra-Thomas J, Bollag RJ, Silver LM, Papaioannou VE. Expression of the T-box family genes, Tbx1-Tbx5, during early mouse development. Dev Dyn 1996; 206: 379-90.
CrossRef - George K. Paraskevas, Basileios Papaziogas, Alexandros Tzaveas, George GiaglisC, Panagiotis Kitsoulis, Konstantino, Natsis. The supratrochlear foramen of the humerus and its relation to the medullary canal: A potential surgical application. Med Sci Monit, 2010; 16(4): BR119-123.
- Singh S, Singh SP. A study of the supratrochlear foramen in the humerus of North Indians. J Anat Soc India. 1972; 21:52-56.
- Diwan RK, Rani A, Chopra J, Srivastava AK, Sharma PK, Verma RK, et al. Incidence of Supratrochlear foramen of Humerus in North Indian Population. Biomedical Research. 2013; 24(1):142-45.
- Mays S. Septal aperture of the humerus in a medieval human skeletal population. Am J Phys Anthropol 2008; 136:432-40.
- Asha Joselet Mathew, Geetha Sulochana Gopidas, Tintu Thottiyil Sukumaran. A Study of the Supratrochlear Foramen of the Humerus: Anatomical and Clinical Perspective. Journal of Clinical and Diagnostic Research. 2016 Feb, Vol-10(2): AC05-AC08.
- Shivaleela C., Khizer Hussain Afroze, Lakshmiprabha S. An osteological study of the supratrochlear foramen of the humerus of south Indian population with reference to anatomical and clinical implications. Anat Cell Biol 2016; 49:249-253.
CrossRef - Macalister A. Anatomical notes and queries. Series II. 1. Perforate humeri in ancient Egyptian skeletons. J Anat Phys 1990; 35: 121-2.
- Baskar S, Kumar S. Variations in carrying angle between two sexes on the complete extension. J Pharm Sci Res 2013; 5:269.
- Agrawal D, Sujatha GB, Rani VS, Chinara PK. A Study of Supratrochlear Foramen and Their Members. 2018 Mar;7(2):154.
CrossRef - Akabori E. Septal apertures in the humerus in Japanese, Ainu and Koreans. Am J Phys Anthropol 1934; 18: 395-400.
CrossRef - Arunkumar K, Manoranjitham R, Raviraj K, Dhanalakshmi V. Morphological study of supratrochlear foramen of humerus and its clinical implications. Int J Anat Res 2015; 3: 1321-5.
CrossRef - Ali Husham Abo Sablan, Melina Calmon. Supratrochlear foramen frequency In three Iraqi populations. FSIR 2 (2020) 100107.
CrossRef - Ananthi K, Manickam S, Vaithianathan G, Aruna S, Ramalingam. Study of intercondyloid foramen of humerus. Rev Arg de Anat Clin. 2011;3(1):32-36.
- Ilhan Bahsi. An Anatomic Study of the Supratrochlear Foramen of the Humerus and Review of the Literature. Eur J Ther 2019; 25(4): 295-303.
CrossRef - Bradshaw R, Constantine Eliopoulos , Matteo Borrini. Septal Aperture of the Humerus: Etiology and Frequency Rates in Two European Populations. The anatomical record. 2019. 303(7) 1821-1830.
CrossRef - Bokhari, Nida Qasim Hayat , Qamar Ashfaq Ahmad , Maria Noman , Mahjabeen Muneera , Raafea Tafweez Kuraishi. The Supratrochlear Foramen of Humerus: A Human Anatomic Study. P J M H S. 2018, 12(3), 980-82.
- Chatterjee KP. The incidence of perforation of olecranon fossa in the humerus among Indians. Eastern Anthropol 1968;21:279-84.
- Chagas Carlos AA, Gabriel gutfiten-Schlesinger, Túlio FO Leite, Lucas AS Pires, Julio G. Silva. Anatomical and Radiological Aspects of the Supratrochlear Foramen in Brazilians. Journal of Clinical and Diagnostic Research. 2016 Sep, Vol-10(9): AC10-AC13.
CrossRef - Cimen M, Kosar Y, Sonmez M. Humerus ta apertura septalis ile ilgili bir arastırma. Antropoloji 2003; 14:20-3.
- Dang Bhumica , Vivek S. Malik , Priyanka Parmar. Supratrochlear Foramen: Incidence, Importance and Clinical Implications in North-Indian Population. Int J Intg Med Sci 2016, Vol 3(4):265-69.
CrossRef - Deshmukh Vishwajit Ravindra, Rohini Arathala, Suryakanta Seth. THE SUPRATROCHLEAR FORAMEN OF THE HUMERUS: FORMATION AND CLINICAL IMPLICATIONS. INTERNATIONAL JOURNAL OF SCIENTIFIC RESEARCH. 2018, 7 (2).763-65.
- Hrdlicka A. The humerus: septal apertures. Anthropology 1932; 10:31-96.
- Jadhav SD, Zambare BR. Supratrochlear foramen and its clinical significance. Asian J Biomed Pharmaceut Sci 2015; 5: 13-5.
CrossRef - Jagdish P, Sumit Kumar. A morphometric study of supratrochlear foramen of humerus in north indian population. global journal for research analysis.2017, 6(9),90-91.
- Joshi MM, Kishve PS, Wabale RN. A morphometric study of supratrochlear foramen of the humerus in western indian dry bone sample. Int J Anat Res 2016; 4: 2609-13.
CrossRef - Kate BR, Dubey PN. A note on the septal apertures in the humerus of Central Indians. East Anthropol 1970; 33:105-10.
- Krishnamurthy A, Yelicharla AR, Takkalapalli A, Munishamappa V, Bovinndala B, Chandramohan M. Supratrochlear foramen of humerus: a morphometric study. Int J Biol Med Res 2011; 2:829- 31.
- Li J, Mao Q, Li W, Li X. An anatomical study of the supratrochlear foramen of the Jining population. Turk Journal Med Sci 2015; 45: 1369-73.
CrossRef - Ming-Tzu P. Septal apertures in the humerus in the Chinese. Am J Phys Anthropol 1935; 20:165-70.
CrossRef - Mayuri J, Aparna T, Pradeep P, Smita M. Anatomical study of supratrochlear foramen of humerus. J Res Med Dent Sci 2017; 1: 33-5.
- Mallikarjun M , Raveendra Patil GT , Solomon Krupanidhi U. Morphological study of supratrochlear foramen in adult dry humerus bones. Int J Anat Res 2020, Vol 8(3.1):7604-08.
CrossRef - Nayak SR, Das S, Krishnamurthy A, Prabhu LV, Potu BK. Supratrochlear foramen of the humerus: An anatomico-radiological study with clinical implications. Ups J Med Sci 2009; 114: 90-4.
CrossRef - Naqshi BF, Shah AB, Gupta S, Raina S, Khan HA, Gupta N, et al. Supratrochlear foramen: an anatomic and clinico-radiological assessment. Int J Health Sci Res 2015; 5: 146-50.
- Ozturk A, Kutlu C, Bayraktar B, Ari Z, Sahinoglu K. The supratrochlear foramen in the humerus: anatomical study. Ist Tip Fak Mecmuasi 2000; 63: 72-6.
- Patel SV, Sutaria LK, Nayak TV, Kanjiya DP, Patel BM, Aterkar SH. Morphometric study of supratrochlear foramen of humerus. Int J Biomed Adv Res 2013; 4: 89-92.
CrossRef - Papaloucas C, Papaloucas M, Stergioulas A. Rare cases of humerus septal apertures in Greeks. Trends Med Res 2011; 6: 178-83.
CrossRef - Raghavendra V. P , Benjamin W, Study of Supratrochlear Foramen of Humerus in South Indian Population. International Journal of Science and Research. 2014, 3 (10), 2244-46.
- Ramamurthi K. Morphometric analysis of supratrochlear foramen of humerus in south indian population. Sch Acad J Biosci 2016; 4: 908-10.
- Satish Kumar S, Suresh Kumar. Supratrochlear foramen-anatomical variations and its clinical implications. Int J Anat Res 2019, Vol 7(3.2):6807-10.
CrossRef - V, Premchand.S.A. Morphology Of Humeral Septal Aperture: An Osteological Study. National Journal of Basic Medical Sciences.2017, 8 (2).83-86.
- Veerappan V, Thotakura B, Aruna S, Kannan G, Narayanan GKB. Study of intercondylar foramen of humerus – clinical and radiological aspect. IOSR-JNHS 2013; 2: 24-7.
CrossRef - Burute P, Singhal S, Priyadarshini S. Supratrochlear Foramen; morphological correlation and clinical significance in western maharashtrian population. IJA 2016; 5: 275-9.
CrossRef - Mahitha B, Jitendra R, Janaki V, Navakalyani T. Supratrochlear foramen of humerus in telangana state: a morphometric study. Int J Anat Res 2016; 4: 2450-3.
CrossRef - De Wilde V, De Maeseneer M, Lenchik L, Van Roy P, Beeckman P, Osteaux M. Normal Osseous variants presenting as cystic or lucent areas on radiography and CT imaging: A pictorial overview. Eur j. Radiol.2004; 51:77-84.
CrossRef







