Manuscript accepted on :04-03-2021
Published online on: 25-05-2021
Plagiarism Check: Yes
Reviewed by: Dr. Sadia Malik
Second Review by: Dr. Salma Rattani
Final Approval by: Dr Ricardo Lagoa
1Department of Nursing Science, College of Applied Medical Sciences in Wadi Add wasir, Prince Sattam Bin Abdulaziz University, Kingdom of Saudi Arabia.
2Pediatric Nursing Department, Faculty of Nursing, Assiut University, Egypt.
Corresponding Author E-mail: atyathassan@aun.edu.eg
DOI : https://dx.doi.org/10.13005/bpj/2175
Abstract
The aim was to assess the prevalence, associated factors, and outcome of neural tube defects (NTDs). A retrospective study design was applied at neonatal intensive care unit.Study subjects: A convenience sample of all (90) neonates who were admitted to the study setting during 12 months period and diagnosed as having NTDs were chosen retrospectively. Tool: One structured interview questionnaire was implemented. It included three sections: Personal and clinical data of neonates, characteristics and clinical data of neonates' mother, and associated factors of NTDs. Study results:It was indicated that 62.2% of neonates were males, 56.7% of NTDs were preterm neonates, 58.9% of neonates were delivered emergency cesarean section (CS). Concerning the discharge outcome from NICU; 46.7% of NTDs' neonates have died. The present study revealed that 55.6% of neonates having NTDs their mothers aged from 20-29 years and 44.4% had parents' consanguinity. Moreover, it was found that NTDs were more prevalent (40% and 37.8%)with mothers who were multigravida <4 and >4 and 76.7% were multipara <4.28% of congenital anomalies (CAs) neonates were having NTDs; 53.3% of NTDs were spina bifida followed by 40% were hydrocephalus and 4.4% were encephalocele. The study results found that recurrent abortions 30% and diabetes mellitus (DM) 4.4%among mothers of the studied neonates before current pregnancy. In addition; 15.6% were taking drugs, 7.8% had an infection, only 6.7% were taking folic acid, and 4.4% had gestational diabetes during current pregnancy.
Keywords
Associated Factors; Neural Tube Defects; Outcome; Prevalence; Retrospective Study
Download this article as:| Copy the following to cite this article: Hassan A. M. Prevalence, Associated Factors, and Outcome of Neural TubeDefects: A Retrospective Study. Biomed Pharmacol J 2021;14(2). |
| Copy the following to cite this URL: Hassan A. M. Prevalence, Associated Factors, and Outcome of Neural TubeDefects: A Retrospective Study. Biomed Pharmacol J 2021;14(2). Available from: https://bit.ly/3wu1LsY |
Introduction
Neural tube defects (NTDs) still a main problem in developing countries 1.Worldwide, the congenital anomalies’ (CAs)are affecting about 3-7% of all neonates. The incidence has been proved to differ from one geographical area to another. Many studies stated, NTDs seem to be the most widespread systemic CAs2, 3, 4 “NTDs are CAs emerging from developmental deformity of the central nervous system (CNS) during the embryonic period” 5. NTDs consist of disorders termed spina bifida, anencephaly, and encephalocele which are all present at birth 1.
NTDs are linked with many factors that could be either genetic or environmental 6. However folic acid deficiency existsas a contributing factor of NTDs 7. So, folic acid supplementation is predictable to decrease the occurrence of NTDs 8. Also, certain associated factors as diabetes mellitus (DM), preconception period fever (indicating infection), and therapeutic drugs have increased the occurrence of NTDs 9, 10, 11. Other associated factors such as parental consanguinity, maternal age, male sex, and prematurity 12.
Prenatal diagnosis of NTDs, its types, and detection of cases have increased its prognosis 13. Survived infants who were born with CAs; have affected their health physically, mentally, or socially. Also, they are more susceptible to morbidity 14.
Study Significance
CAs are one of primary causes of mortality and morbidity in developed and developing countries 15, 16. NTDs encompass a major public health problem.It is estimated that about 300,000 neonates are born each year with NTDs worldwide 17. The WHO in 2010, reported that 270,000 neonates died world wide because of CAs, with NTDs being one of the most serious and most common of these anomalies 18. Treatment and prognosis of infants and/or children with CAs are so difficult 19. So, early detection, diagnosis, and determine causes of CAs consider the base of prevention programs 20.
Study Aim
The aim was to assess the prevalence, associated factors, and outcome of neural tube defects.
Research Question
What is the prevalence, associated factors, and outcome of NTDs among neonates?
Materials and Method
Study design
A retrospective study design was applied in this study.
Study setting
The study conducted at the Neonatal Intensive Care Unit (NICU) in Assiut University Children Hospital.
Study subjects
A convenience sample of all (90) newborn infants(from a total of 1400 neonates). They were admitted to the NICU during 12 months period from January to December 2016 and diagnosed as having NTDs were chosen retrospectively based on medical records of the hospital. NTDs were diagnosed by neonatologists based on the clinical evaluation of neonates.
Data collection tool
One structured interview questionnaire was implemented through three sections as follow
Section I: Personal and clinical data of neonates as;
gestational age, sex, method of delivery, type of gestation, and discharge outcome from NICU.
Section II: Characteristics and clinical data of neonates’ mothers as;
age, job, residence, parents’ consanguinity. Also, number of mothers’ gravidities, parities, abortions, stillbirths, and neonatal deaths.
Section III: Associated factors of neural tube defects containing:
Related to neonates as; male gender, multiple gestations, and preterm neonates.
Related to neonates’ mothers as; age and parents’ consanguinity. And obstetrical history (i.e. multigravida, multipara, and recurrent abortions). History of diseases, complications before current pregnancy (i.e. medical illness as DM and hypertension, and previous congenital anomalies). Complications during current pregnancy (i.e. anemia, gestational diabetes or pregnancy induced hypertension, infection, deficiency of folic acid intake, and taking drugs during pregnancy).
Method
Official permission for conducting the study was obtained from the head of NICU. The aim of the study was clarifying.
The tool’s content validity index (CVI) was done by five experts in the field of pediatric nursing and pediatrics (CVI = 0.9). While Cronbach’s alpha coefficient was used to test the tool’s internal consistency r=0.81.
Nine newborn infants (10%) of the study sample were included in the pilot study. It was applied to test the applicability of the study tool. No changes were performed.It was included in the study sample.
The study data was collected by the researcher. It was performed during four months. From April to August 2017, in the morning and afternoon shift, two days/week.
A written approval was taken from the head of NICU. The researchers confirmed that the collected data used only to fulfill the study aim.
Statistical analysis:
The statistical package for social science software (SPSS) version 16.0was used to enter and analyze the study data. Frequencies and percentages (i.e. qualitative variables) and Means and standard deviations (i.e. quantitative variables) were used to describe the statistics.
Results and Discussion
The study found that 62.2% of neonates were males. It was in the same with 21, 13 who found that anomalies of the CNS were more prevalent (61.1%) among males to females with a ratio of 1.6:1. Disagree with 22 who indicated that sex was not associated with CAs. This result attributed that male gender had lethal, sex, and genetic predisposing factors which affect their health. Regarding gestational age; a higher incidence (56.7%) of NTDs was found among preterm neonates. The result is in accordance with 15 who indicated that a significantly higher incidence of CAs was in preterm neonates when compared with the full term neonates. This could be explained that the presence of CAs made the neonates more complicated and high risk to be delivered before the normal birth time.
Furthermore, 58.9% of neonates were delivered emergency CS this could be due to that most of the NTDs in the studied sample were hydrocephalus and needed urgent CS. Concerning the discharge outcome from NICU; 46.7% of NTDs’ neonates have died. This was in agreement with 22 who reported that the relation between CA and neonatal deaths less frequent than other acute conditions, with no statistically significant difference.
The present study revealed that 55.6% of neonates having NTDs their mothers aged from 20-29 years. Theresult was concurrent with 13 who revealed that 73.6% of mothers aged less than 35 years, their delivered infants had CNS anomaly.23, 24 indicated that the median mother’s age at CAs’ diagnosis was between 20 -< 30 years old. Furthermore, 44.4% had parents’ consanguinity. The finding was strengthened by 25, 26. This could be attributed that consanguinity is considered one of the most common contributing factors in transferring CAs’ genetic traits.
Moreover, it was found that NTDs were more prevalent among multigravida mothers <4 and more than 4 (40% and 37.8% respectively) and multipara <4 were 76.7%. These were in the same line with 27, 25 who highlighted that multiparty was one of the obstetrical risk factors for congenital malformation in Egypt.
The total number of neonatal admission was 1400 neonates; 90 (6.4%) of themhave NTDs. 28% were having NTDs, while 72% were having other congenital anomalies. These results were consistent with 13, 28 who found that NTDs were the most frequent types of CAs (32.5%). Also,1 indicated that 63.3/10 000 children in Ethiopia have NTDs. As well, the study findings revealed that 53.3% of NTDs were spina bifida followed by 40% were hydrocephalus and 4.4% were encephalocele. It came in agreement with 29, 13 who reported that spina bifida was the most prevalent NTDs (68.1%).Also,1, 21 declared that spina bifida, anencephaly, and encephalocele were the mostprevalent. This could be explained by the prevalence and type of NTDs may differ with time and/or geographical setting.
The study results found that recurrent abortions 30% and diabetes mellitus 4.4% were the most associated factors as regards NSTDs before current pregnancy among mothers of the studied neonates. 30, 27, 31 support this study result. As they declared that occurrence of illness during pregnancy especially in the first trimester, recurrent abortions, and DM were risk factors that increase prevalence of CAs in neonates.
In addition; the most associated factors as regards NSTDs during current pregnancy among mothers of the studied neonates were 15.6% taking drugs, 7.8% had infection, only 6.7% taking folic acid, and 4.4% had gestational diabetes. These results were supported by 21, 28, 13 demonstrated that lack of folic acid supplementation, and history of febrile illness in the first trimester, and DMin pregnancy were associated factors for NTDs. Moreover, 24 emphasized that maternal infection with toxoplasmosis represented an important role in having neonate with CAs as pregnancy outcome.
Likewise, Egyptian studies done by 32, 33 revealed that taking drugs during pregnancy, and having infections considered risk factors that increase the incidence of CAs. Similarly, other studies implemented in Egypt by 25, 34 demonstrated that maternal disease as DM, the presence of fever due to infections, and medications misuse during pregnancy were maternal risk factors for CAs in Egypt.
Results
Table 1: Personal and clinical data of the studied neonates (N=90):
| Data of neonates | No | % |
| Sex | ||
| · Male | 56 | 62.2 |
| Female | 34 | 37.8 |
| Type of neonates’ gestation | ||
| · Single | 81 | 90.0 |
| · One of twins | 9 | 10.0 |
| Gestational age | ||
| Preterm | 51 | 56.7 |
| Full term | 39 | 43.3 |
| Mean ± SD(Min-max) | 36.9 ± 2.2 (28-40) | |
| Method of delivery | ||
| Normal vaginal delivery | 16 | 17.8 |
| Elective CS | 21 | 23.3 |
| Emergency CS | 53 | 58.9 |
| Discharge outcome from NICU | ||
| Improvement | 48 | 53.3 |
| Death | 42 | 46.7 |
Table 2: Characteristics of the studied neonates’ mothers (N=90):
| Characteristics of mothers | No | % |
| Age/years | ||
| <20 | 10 | 11.1 |
| 20-29 | 50 | 55.6 |
| 30-39 | 26 | 28.9 |
| 40 and more | 4 | 4.4 |
| Mean ± SD(Min-max) | 26.8 ± 6.5 (16-43) | |
| Occupation | ||
| Housewife | 78 | 80 |
| Working | 18 | 20 |
| Residence | ||
| Rural | 64 | 71.1 |
| Urban | 26 | 28.9 |
| Parents’ consanguinity | ||
| Present | 40 | 44.4 |
| Not present | 50 | 55.6 |
Table 3: Obstetric history of mothers of the studied neonates (N=90):
| Obstetric history | No | % |
| Number of gravidities | ||
| · Primigravida | 20 | 22.2 |
| · <4 | 36 | 40.0 |
| · 4 and more | 34 | 37.8 |
| Mean ± SD (Min-max) | 3.2 ±2.0 (1-9) | |
| Number of parities | ||
| · <4 | 69 | 76.7 |
| · 4 and more | 21 | 23.3 |
| Mean ± SD (Min-max) | 2.9 ± 1.6 (1-7) | |
| Number of abortions | ||
| · No | 63 | 70.0 |
| · <3 | 22 | 24.4 |
| · 3 and more | 5 | 5.6 |
| Number of still births | ||
| · No | 89 | 98.9 |
| · 1-2 | 1 | 1.1 |
| Number of neonatal deaths | ||
| · No | 82 | 91.1 |
| · Yes | 8 | 8.9 |
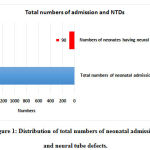 |
Figure 1: Distribution of total numbers of neonatal admission and neural tube defects. |
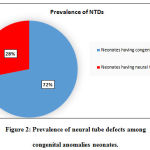 |
Figure 2: Prevalence of neural tube defects among congenital anomalies neonates. |
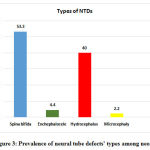 |
Figure 3: Prevalence of neural tube defects‘ types among neonates. |
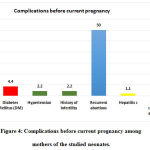 |
Figure 4: Complications before current pregnancy among mothers of the studied neonates. |
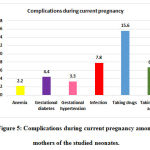 |
Figure 5: Complications during current pregnancy among mothers of the studied neonates. |
Conclusion
NTDs were more prevalent among the studied neonates; 28% of CAs neonates were having NTDs, spina bifida and hydrocephalus were the most frequent types. 46.7% of NTDs’ neonates have died on discharge from NICU. Male sex, preterm birth,mothers’ age, parents’ consanguinity, multigravida, and multipara were associated factors for NTDs. Likewise, complications before current pregnancy as;recurrent abortions and presence of medical illness e.g. DM, and complications during current pregnancy as;taking drugs, catching an infection, folic acid deficiency, and gestational diabetes were associated factors for NTDs. So, the study recommended that early detection and diagnosis of NTDs are important for planning care and knowing the etiology and are the base of prevention programs.
Acknowledgement
Thanks to Dr. Amal Hussian who assisted in data collection.
Conflict of Interest
No conflict of interest.
Funding Source
None
References
- Bitew Z, Worku T, Alebel A, and Alemu A. Magnitude and Associated Factors of Neural Tube Defects in Ethiopia: A Systematic Review and Meta-Analysis. Global Pediatric Health, 2020; 7:1-14
CrossRef - Mashuda F, Zuechner A, Chalya P, Kidenya B, Manyama M. Pattern and factors associated with congenital anomalies among young infants admitted at Bugando medical centre, Mwanza. Tanzania. BMC Res Notes, 2014; 7:195.
CrossRef - Obu H, Chinawa J, Uleanya N, Adimora G, Obi I. Congenital malformations among newborns admitted in the neonatal unit of a tertiary hospital in Enugu. South‑East Nigeria – A retrospective study. BMC Res Notes,2012; 5:177.
CrossRef - Saiyad S and Jadav H. Study of congenital malformations in central nervous system and gastrointestinal tract. Natl J Med Res,2012; 2:121‑
- Botto L, Moore C, Khoury M and Erickson J. Neural tube defects. N Engl J Med,1999; 341:1509-1519.
CrossRef - Padmanabhan R. Etiology, pathogenesis and prevention of neural tube defects. CongenitAnom (Kyoto),2006; 46:55-67.
CrossRef - Dolin C, Deierlein A, Evans M. Folic acid supplementation to prevent recurrent neural tube defects: 4 milligrams is too much. Fetal DiagnTher, 2018; 44:161-165.
CrossRef - Greene N, Leung K and Copp A. Inositol, neural tube closure and the prevention of neural tube defects. BirthDefects Res,2017; 109:68-80.
CrossRef - Welderufael A, Berihu B and Berhe Y. Nutritional status among women whose pregnancy outcome was afflicted with neural tube defects in Tigray region of Ethiopia. Brain Dev, 2019; 41:406-412.
CrossRef - Liu S, Evans J and MacFarlane A. Association of maternal risk factors with the recent rise of neural tube defects in Canada. PaediatrPerinatEpidemiol, 2019; 33:145-153.
CrossRef - Kerr S, Parker S, Mitchell A, Tinker S and Werler M. Periconceptional maternal fever, folic acid intake, and the risk for neural tube defects. Ann Epidemiol, 2017; 27(12): 777–782.
CrossRef - Taksande A, Vilhekar K, Chaturvedi P and Jain M. Congenital malformations at birth in Central India: A rural medical college hospital based data. Indian J Hum Genet,2010; 16:159‑
CrossRef - Eke C, Uche E, Chinawa J, Obi I, Obu H, Ibekwe R. Epidemiology of congenital anomalies of the central nervous system in children in Enugu, Nigeria: A retrospective study. Ann Afr Med, 2016; 15:126-32.
CrossRef - World Health Organization. Primary healthcare approaches for prevention and control of congenital and genetic disorders (WHO/HGN/WG/001). Geneva: World Health Organization; 2000.
- Seba B, Shubhankar M, and Sambedana P. Congenital Anomalies in Neonates and Associated Risk Factors in a Tertiary Care Hospital: A Single Center Study from India. Indian Journal of Applied Research, Pediatrics, 2017; 7(11): 174-176.
- Amar T., Krishna V., Pushpa C., and Manish J. Congenital Malformations at Birth in Central India: A Rural Medical College Hospital Based Data. Indian J Hum Genet, 2010; 16:159–63.
CrossRef - Christianson A, Howson C, and Modell B. Global report on birth defects: the hidden toll of dying and disabled children, White Plains (NY): March of Dimes Birth Defects Foundation 2006.
- World Health Organization, “Fact sheet No 370. October 2012,” http://www.who.int/mediacentre/factsheets/fs370/en/index.html.
- Isa A, Masomeh K and Hamid-Reza F. The Prevalence at Birth of Overt Congenital Anomalies in Urmia, Northwestern Iran .Archives of Iranian Medicine, 2008; 11: 148 –51.
- Singh A, Ravinder K and Jammu S. Pattern of Congenital Anomalies in Newborn: A Hospital Based Prospective, Jammu (J&K)-India, 2009; 11:34-36.
- Gedefaw A, Teklu S, and Tadesse B. Magnitude of Neural Tube Defects and Associated Risk Factors at Three Teaching Hospitals in Addis Ababa, Ethiopia. HindawiBioMed Research International, 2018; 2018: 4829023
CrossRef - Ajao A and Adeoye Adeoye1Prevalence, risk factors and outcome of congenital anomalies among neonatal admissions in OGBOMOSO, Nigeria. BMC Pediatrics, 2019; 19:88
CrossRef - Aloui M, Nasri K, Ben Jemaa N, Ben Hamida A, Masmoudi A, Gaıgi S and Marrakchi R. Congenital Anomalies in Tunisia: Frequency and Risk Factors. J GynecolObstet Hum Reprod, 2017; 46: 651–655.
CrossRef - Sunitha T, Prasoona K, Kumari T, Srinadh B, Deepika M, Aruna R and Jyothy A. Risk Factors for Congenital Anomalies in High Risk Pregnant Women: A Large Study from South India. The Egyptian Journal of Medical Human Genetics. HOSTED BY Ain Shams University, 2017; 18: 79–85.
CrossRef - Mohammed A, Mohammed S and AbdulFatah A. Congenital Anomalies among Children: Knowledge and Attitude of Egyptian and Saudi Mothers. Journal of Biology, Agriculture and Healthcare, 2013; 3(20): 18-32.
- Tayebi N, Yazdani K and Naghshin N. The Prevalence of Congenital Malformations and its Correlation with Consanguineous. OMJ, 2010; 25: 37-40.
CrossRef - Căpățînă D and Camelia C. Risk Factors Associated with Congenital Anomalies in Children ARS MedicaTomitana, 2015; 2(21): 105 -111.
CrossRef - Adane F and Seyoum G. Prevalence and associated factors of birth defects among newborns at referral hospitals in Northwest Ethiopia. Ethiop. J. Health Dev. Ethiop. J. Health Dev. 2018; 32(3):1-7
- Holmbeck G, Zebracki K, Papadakis J, Driscoll C. Spina bifida. In: Roberts MC, Steele RG, eds. Handbook of Pediatric Psychology. 5th ed. Guilford; 2017:312-322.
- Rani S and Lakshmi V. Study of Congenital Malformations in a Tertiary Hospital, Government General Hospital, Guntur. IOSR Journal of Dental and Medical Sciences, 2015; 14(4):16-20.
- Pal A, Mukhopadhyay D, Deoghuria D, Mandol S, Patra A, and Murmu S. Prevalence of Congenital Malformations in Newborns Delivered in a Rural Medical College Hospital, West Bengal. IOSR Journal of Dental and Medical Sciences, 2015; 14(12):26-32.
- Aly E and Abd-Manaf M. Prevalence and Risk Factors for Major Congenital Anomalies among Egyptian Women: A Four-Year Study. Med. J. Cairo Univ, September, 2013; 81(1): 757-762.
- Ahmed A, Abd el Kader S, Abd El Hamid A and Gaafar M. Assessment of Risk Factors for Fetal Congenital Anomalies among Pregnant Women at Cairo University Hospitals. Journal of American Science, 2011;7-(12)
- Shawky R and Sadik D. Congenital Malformations Prevalent among Egyptian Children and Associated Risk Factors. Egypt JMed Hum Genet, 2011; 12:69–78.
CrossRef








