Manuscript accepted on :27-05-2021
Published online on: 09-06-2021
Plagiarism Check: Yes
Reviewed by: Avtanski, Dimitar B
Second Review by: Dr. Ana Golez
Final Approval by: Dr Ayush Dogra
Yogesh Chhaparwal1 , Mathangi Kumar1*
, Mathangi Kumar1* and Shubha Chhaparwal2
and Shubha Chhaparwal2
1Department of Oral Medicine and Radiology, Manipal College of Dental Sciences, Manipal, Manipal Academy of Higher Education, Manipal 576104, Karnataka, India.
2Department of Conservative Dentistry and Endodontics, Manipal College of Dental Sciences, Manipal, Manipal Academy of Higher Education, Manipal 576104, Karnataka, India.
Corresponding Author Email: mathangi.kumar@manipal.edu
DOI : https://dx.doi.org/10.13005/bpj/2194
Abstract
Trigeminal neuralgia is the most common neuralgia affecting the orofacial region. The condition characterized by sudden, severe electric shock like pain on the face with pain free periods and is termed as refractory period.Management of this condition is achieved through various drug therapies and in some cases, surgical intervention may be required. Refractory trigeminal neuralgia is a condition that is non responsive to the traditional line of therapy. This poses a challenge to the clinicians to offer the patients alternate options for pain control in these patients. In this review, an attempt has been made to discuss the various drug therapies in the management of refractory trigeminal neuralgia.
Keywords
Facial pain; Neuralgia; Trigeminal Nerve; Therapeutics
Download this article as:| Copy the following to cite this article: Chhaparwal Y, Kumar M, Chhaparwal S. Drug Therapy for Refractory Trigeminal Neuralgia- A Review. Biomed Pharmacol J 2021;14(2). |
| Copy the following to cite this URL: Chhaparwal Y, Kumar M, Chhaparwal S. Drug Therapy for Refractory Trigeminal Neuralgia- A Review. Biomed Pharmacol J 2021;14(2). Available from: https://bit.ly/351WHjQ |
Introduction
Trigeminal neuralgia is defined by International association for the study of pain as “A sudden usually unilateral, severe, brief, stabbing, recurrent pain in the distribution of one or more branches of the fifth cranial nerve1. The area of distribution is mainly on face which is innervated by trigeminal nerve. The prevalence of this condition is 1 in 25,000 individuals. In 1756 the term “tic douloureux” (painful jerking) was coined by Nicolaus Andre. In 1773, Fothergill described this disease and hence called as “Fothergill’s disease”.
The exact cause of trigeminal neuralgia is unknown. However most widely accepted theory remains the atherosclerotic blood vessel (usually the superior cerebellar artery) pressing on and grooving the root of the trigeminal nerve. This pressure results in focal demyelinization and hyperexcitability of nerve fibers2,3, which will then fire in response to light touch (allodynia), resulting in brief episodes of intense pain. The International Headache society classifies trigeminal neuralgia into two types as primary or idiopathic with no known clinical neurological defect and secondary trigeminal neuralgia with a structural neurological lesion.
The pain in trigeminal neuralgia is characteristic with unilateral occurrence in most cases and confined to the distribution of trigeminal nerve. The pain is typically described as electric shock like, paroxysmal and lasts from a fraction of second to minutes. There are trigger zones which are an area of facial skin or oral mucosa where a light touch can trigger neuralgic pain in an individual. These trigger zones are pathognomic of trigeminal neuralgia.
These paraoxysmal pain episodes are variable and may differ from among patients affecting their quality of life. The management of trigeminal neuralgia includes both medical and surgical treatment options. However medical management is always considered first line and if patient doesnot respond to conventional drug therapy it is categorized as Refractory trigeminal neuralgia. Refractory trigeminal neuralgia is a trigeminal neuralgia which is non responsive tothe standard care of treatment4.
Conventional treatment of trigeminal neuralgia
The conventional standard treatment includes: First line drugs and second line drugs in the management of trigeminal neuralgia.
First line drugs
Carbamazepine is the initial drug of choice for the management of trigeminal neuralgia. Carbamazepine is given in doses in the range of 200-1200mg/day depending on the severity of pain episodes5. The mechanism of action of this drug is its ability to block voltage gated sodium channels and thereby neutralizing hyperexcitable neural membranes. Common side effects include drowsiness, ataxia and hyponatremia. Some serious side effects include myelosuppression, Steven Johnson syndrome and aplastic anemia. It is imperative to monitor complete blood count, serum sodium and liver function test in patients who are under carbamazepine.
Oxcarbamazepine is a ketoanalogue which has lesser side effects. It is better safety profile and is considered in patients who are not able to tolerate carbamazepine6.
Second line drugs
The various management options for refractory trigeminal neuralgia is described in Figure 1.
Patients who do not respond to first line therapy of carbamazepine and oxcarbamazepine are often considered for second line of drugs which include:
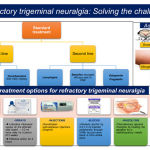 |
Figure 1: Figure depicting various management options for refractory trigeminal neuralgia. |
Baclofen
The main clinical use of baclofen is in treatment of spastic disorders. It has shown promise to relieve symptoms of trigeminal neuralgia in the dose between 10-60mg/day. This drug has reported high efficacy second most to carbamazepine. In a study conducted on 30 patients where one group was treated with carbamazepine, second group with baclofen and third group with combination of both. Their result showed that baclofen was more efficacious in relieving the symptoms of neuralgia7,8.
Lamotrigine
Lamotrigine is an antiepileptic drug used to treat partial and generalized tonic clonic seizures. It acts as neural membrane stabilizer by acting against voltage gated sodium channels. It is usually given in gradually increasing dose to 200-400mg/day in two dose schedule. It is an adjuvant drug to carbamazepine and has shown promising results.In a randomized controlled trial conducted on 14 patients with refractory trigeminal neuralgia, it showed that more patients were benefited by adding lamotrigine as an adjuvant drug compared to placebo9. However adverse effects of skin reactions in form of rash has been reported and doses should be increased gradually with monitoring of skin reactions as dose increases.
Gabapentin
Gabapentin is primarily an epileptic drug and has shown great promise in patients who were not responding to first line of therapy. In a study where 194 cases of trigeminal neuralgia not responding to first line drugs were treated with gabapentin and 43 patients reported partial to complete pain relief in first two weeks of therapy. During the follow up time of eight months pain relief was continued in majority of patients10. It can be given in a dose range of 100-2400 mg/day in divided doses. Hyperlipidemia is the most common side effect noted among patients treated with this drug.
Newer drugs for patients not responding to first and second line drugs
Topiramate
Newer epileptic drug tried in patients not responding to conventional drug therapy. Various studies where patients are tried with low initial dose of 50 to 100 mg a day have shown moderate to complete resolution in some patients11. However cognitive impairment is reported in patients treated with topiramate and hence this drug must be used with caution.
Levitiracetam
This drug is mainly used as an adjuvant drug to conventional drug therapy. In one observational trial 23 patients showed reduction of pain attacks with levitiracetam as the adjuvant drug12. However large randomized clinical trial is warranted before its use in clinical practice.
Tizanidine
It is a central muscle relaxant which is tried in patients with trigeminal neuralgia. However small sample size in clinical trials limits its use. In a study carried out with 12 patients where comparison of efficacy between tizanidine and carbamazepine were done and their result no difference in their efficacy13.
Sodium valproate
In patients with refractory trigeminal neuralgia, sodium valproate at a dose of 800 to 1600 mg/day, has reported 50 to 75% improvement in reducing the pain symptoms and severity of attacks14. The safety profile of the drug was proven to be satisfactory with no renal and hepatic side effects.
Botulinum Toxin
Recently botulinum toxin has gained popularity in the treatment of migraine and neuralgia of occipital origin. A study conducted to evaluate the role of botulinum toxin in patients with refractory trigeminal neuralgia showed significant improvement in number and severity of pain attacks after six months of injection15.
Conclusion
Trigeminal neuralgia is not an uncommon disorder affecting many patients. Refractory trigeminal neuralgia is when the disorder is non-responsive to conventional management options. Medical management of this condition remains the first line of choice and hence a thorough knowledge about the various treatment options will aid us in achieving pain control for these patients.
Acknowledgments
None
Conflict of interest
The authors do not have any conflict of interest.
References
- The International Classification of Headache Disorders: 2nd edition. Cephalalgia24:9-160 (2004).
- Devor M, Amir R, Rappaport ZH. Pathophysiology of trigeminal neuralgia: the ignition hypothesis. The Clinical journal of pain18(1):4-13 (2002).
CrossRef - Siqueira SR, Alves B, Malpartida HM, Teixeira MJ, Siqueira JT. Abnormal expression of voltage-gated sodium channels Nav1. 7, Nav1. 3 and Nav1. 8 in trigeminal neuralgia. Neuroscience 164(2):573-575 (2009).
CrossRef - Cruccu G, Gronseth G, Alksne J, Argoff C, Brainin M, Burchiel K, Nurmikko T, Zakrzewska JM. AAN‐EFNS guidelines on trigeminal neuralgia management. European journal of neurology15(10):1013-1028 (2008)
CrossRef - Killian JM, Fromm GH. Carbamazepine in the treatment of neuralgia: use and side effects. Archives of neurology19(2):129-136 (1968).
CrossRef - Nasreddine W, Beydoun A. Oxcarbazepine in neuropathic pain. Expert opinion on investigational drugs16(10):1615-1625 (2007).
CrossRef - Fromm GH, Terrence CF, Chattha AS. Baclofen in the treatment of trigeminal neuralgia: double‐blind study and long‐term follow‐up. Annals of Neurology: Official Journal of the American Neurological Association and the Child Neurology Society15(3):240-244 (1984).
CrossRef - Gronseth G, Cruccu G, Alksne J, Argoff C, Brainin M, Burchiel K, Nurmikko T, Zakrzewska JM. Practice parameter: the diagnostic evaluation and treatment of trigeminal neuralgia (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology and the European Federation of Neurological Societies. Neurology71(15):1183-1190 (2008).
CrossRef - Zakrzewska JM, Chaudhry Z, Nurmikko TJ, Patton DW, Mullens EL. Lamotrigine (lamictal) in refractory trigeminal neuralgia: results from a double-blind placebo controlled crossover trial. Pain73(2):223-230 (1997).
CrossRef - Cheshire Jr WP. Defining the role for gabapentin in the treatment of trigeminal neuralgia: a retrospective study. The Journal of Pain3(2):137-142 (2002).
CrossRef - Domingues RB, Kuster GW, Aquino CC. Treatment of trigeminal neuralgia with low doses of topiramate. Arquivos de neuro-psiquiatria65(3B):792-794 (2007).
CrossRef - Mitsikostas DD, Pantes GV, Avramidis TG, Karageorgiou KE, Gatzonis SD, Stathis PG, Fili VA, Siatouni AD, Vikelis M. An observational trial to investigate the efficacy and tolerability of levetiracetam in trigeminal neuralgia. Headache: The Journal of Head and Face Pain50(8):1371-1377 (2010).
CrossRef - Vilming ST, Lyberg T, Lataste X. Tizanidine in the management of trigeminal neuralgia. Cephalalgia6(3):181-182 (1986).
CrossRef - Spina E, Perugi G. Antiepileptic drugs: indications other than epilepsy. Epileptic disorders 6(2):57-75(2004).
- Bohluli B, Motamedi MH, Bagheri SC, Bayat M, Lassemi E, Navi F, Moharamnejad N. Use of botulinum toxin A for drug-refractory trigeminal neuralgia: preliminary report. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology111:47-50 (2011).
CrossRef







