Manuscript accepted on :16-01-2021
Published online on: 11-02-2021
Plagiarism Check: Yes
Reviewed by: Dr. Donna Edwards
Second Review by: Dr. Vikrant Rai
Final Approval by: Dr. Ayush Dogra
Naisal Rassi1 , M J Sudha2*
, M J Sudha2* , S Viveka3
, S Viveka3 , Salih Sharafudeen1
, Salih Sharafudeen1
1Medical Undergraduate student, Azeezia Institute of Medical Sciences and Research, Kollam, Kerala, India.
2Department of Pharmacology, Azeezia Institute of Medical Sciences and Research, Kollam, Kerala, India.
3Department of Anatomy, Azeezia Institute of Medical Sciences and Research, Kollam, Kerala, India.
Corresponding Author E-mail: sudhasudhasudha@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2133
Abstract
Background and objectives: The important component of all antibiotic stewardship program is education of clinicians about the antimicrobial usage. The objective of the study was to evaluate the knowledge and attitudes regarding antibiotic resistance among medical doctors in a tertiary care hospital. The other objective was to evaluate the usefulness of the interactive educational intervention in improving the knowledge about antibiotic resistance
Methodology: This was a cross sectional questionnaire based study involving residents and postgraduates from various departments. Questionnaire had three categories of assessment, namely, knowledge about the development of antimicrobial resistance (fifteen questions), treatment of resistant microbial conditions (five questions) and prevention of antimicrobial resistance (five questions). Questionnaire was pre-tested and pilot run.
After the filling up of the questionnaire, each participant or a group of three or four participants were provided with interactive educational intervention. In each such session, three components were discussed using a custom designed course module using a learning management system. The modes of development of antimicrobial resistance, methods of rationale antimicrobial prescription and interventions to prevent development of antimicrobial resistance were the main components in the online module. After the online course, each participant filled post-test. The long-term retention of the concepts was tested with one-month follow-up post-test.
Results: 120 participants have taken up the pre-test and undergone the study. Pre-test average score was 11.1(± 3.44) out of 25. Of these participants 114, have taken immediate post-test and average score was 20.9 (± 2.67). The improvement of pre-test scores to post-test scores was statistically significant. 94 participants have answered the one-month post-test, the average score was 16 (± 4.79). The results were statistically significantly more than the pre-test score, however statistically lower than post-test score.
Conclusion: Use of the interactive online learning material has resulted in significant improvement in the knowledge and attitude regarding antibiotic resistance among post-graduates and interns in a tertiary care hospital.
Keywords
Antimicrobial Resistance; Interactive Learning; Online Modules
Download this article as:| Copy the following to cite this article: Rassi N, Sudha M. J, Viveka S, Sharafudeen S. The Impact of Educational Intervention on Knowledge and Attitude Regarding Antibiotic Resistance Among Medical Doctors in A Tertiary Care Hospital. Biomed Pharmacol J 2021;14(1) |
| Copy the following to cite this URL: Rassi N, Sudha M. J, Viveka S, Sharafudeen S. The Impact of Educational Intervention on Knowledge and Attitude Regarding Antibiotic Resistance Among Medical Doctors in A Tertiary Care Hospital. Biomed Pharmacol J 2021;14(1). Available from: https://bit.ly/3qcKpOt |
Introduction
Our time with antibiotics is running out.1 World Health Organization (WHO) is continuously emphasizing all health care stakeholders for responsible use of antibiotics to prevent rampant development of resistance. In this regard, WHO is organizing World Antibiotic Awareness Week aiming to increase awareness of development of antibiotic resistance.2 At the same time, it is also encouraging best practices among health care providers and policy makers to avoid further antibiotic resistance. Effective communication, education and training of health care providers are the important steps advocated by WHO.3Centre for disease control (CDC) is also promoting hospital antibiotic stewardship programs to encourage responsible antibiotic usage.4 Antibiotic stewardship programs are hospital based programs directed towards optimization of antibiotic use and reduce adverse events associated with antibiotic use.5
As the microbes are fast replicating, there is every possible chance that it develops some of the mechanisms to circumvent the detrimental effects of drugs used against them. Few microbes can alter the drug targets, inactivate the drug or can efflux the drug.6,7Micro-organisms are known to horizontally transfer the genes to other microbes.8 With the emergence of multidrug, extremely drug resistant and pan drug resistant superbugs, the antimicrobial resistance has become a major problem & has occupied a centre stage in all intensive care settings9 Methicillin resistant Staphylococcus aureus (MRSA), vancomycin resistant enterococci(VRE) and carbapenem resistant Enterobacteriaceae are the three most important microbes posing threats with severe systemic uncontrolled infections.10,11
For limiting development of resistance, the health care professionals need to strictly utilize the antimicrobial drugs, identify the causative organism wherever possible, select appropriate drug for correct duration at proper dosage.12 Indian Council of Medical Research (ICMR) has formulated guidelines for hospital infection control and Antimicrobial Stewardship Program addressing antimicrobial resistance.13National policy for containment of antimicrobial resistance, has been formulated to address the same,14 but development of individual policies at local level also plays a crucial role & takes us a long way in preventing development of antimicrobial resistance.
Antibiotic stewardship is defined as the optimal selection, dosage and duration of the antimicrobial treatment resulting in best clinical outcomes with minimal impact on the subsequent development of resistance.15The major goal of antimicrobial stewardship is to encourage health care professionals to prescribe the most appropriate antimicrobial for a given clinical condition with correct dose and duration. This practice follows 4Ds of antimicrobial therapy, namely, right Drug, right Dose, De-escalation to pathogen directed therapy and right Duration of the therapy.16With such an approach – the overall treatment cost is set to come down as fewer doses are used and less expensive drugs are chosen.17It also emphasizes to prevent antimicrobial overuse, misuse, and abuse. Minimize the development of resistance by use of antibiotics for common illnesses is associated with emergence of resistance strains as shown by many meta-analysis.18The most important antimicrobial resistance leading to increased morbidity and mortality are Carbapenem-resistant K pneumonia16and Methicillin-resistant S aureus.19
Pre-prescription restrictive approach enforces limited use or complete restriction of certain antimicrobials by clinicians. Use of such restricted antibiotics requires prior permission with sound evidence from the concerned authorities. This approach has resulted in decrease in overall expenditure of antimicrobials. Also, this has led to over usage of the antibiotics that are not restricted.20The other form of antibiotic stewardship program uses effective prospective review and feedback after the entire treatment. Such post-prescription surveys and audits recommend individual clinicians to adjust, change or use appropriate dose, de-escalate the antibiotics based on microbiology results of the hospital and clinical status of the patient.21 The institutions not having sufficient resources for the regular pre-prescription restrictive approach for the antibiotic stewardship program are encouraged to follow post-prescription review with feedback to work towards prevention of antibiotic resistance.
The fundamental component of all antibiotic stewardship program is education of clinicians about the antimicrobial usage. Usually clinicians get such information about the antimicrobial usage, dosage, duration and de-escalation while reading the treatment algorithms of a particular infectious condition. Continued medical education and clinical meets about the routine cases can supplement or update the information of antibiotic usage. Regular conversation with the antibiotic stewardship program co-ordinators who are deeply involved can substantially alter the dosage, drug and duration. Post-prescription review and feedback also effectively influences the prescription habits of the clinicians. Formal didactic sessions or grand rounds–type lectures can also influence the overall outcomes.17
The orientation of clinicians towards better antibiotic stewardship programstarts with understanding their perception about the antibiotic resistance. Many researchers have reported heighted awareness of infection control measures are essential specially during institutional antibiotic therapy.22 Overall, most agree that the provision of up-to-date antibiotic prescription guidelines clubbed with physician sensitization shall lead to reduction of unnecessary antibiotic prescription. In addition, health warning on the antibiotic prescription bags to emphasize the importance of hygiene during treatment must be emphasised. In this regard, many studies have evaluated the knowledge, attitude and practices of the clinicians (especially house surgeons and postgraduates) regarding the antibiotic resistance. The following paragraphs mentions few such studies conducted in India.
Mohit Nair et al, evaluated the use of antibiotic usage among doctors, nurses, informal providers, and pharmacy shopkeepers.23 They found, doctors, even though scored higher in questions assessing knowledge and attitudes, scored poorer in practices assessment. They recommend to address the ‘nexus’ between the doctors, pharmaceutical representatives and informal health care providers to tackle the drug resistance problem. VandanaBadar et al, evaluated the knowledge and attitude of medical teachers and clinicians in a tertiary care hospital; opined that all medical faculty are fairly oriented to principles of clinical practices leading to prevention of development of antimicrobial resistance.24 They suggest computer assisted programs for effective antimicrobial stewardship program. Manali Mahajan et al, studied knowledge and attitude of undergraduate students in a medical college and recommended that antimicrobial resistance should be a part of pharmacology curriculum.25 Further, Anita Kotwani et al, studied such knowledge and attitude among high school students and their teachers through focus group discussions. They found that students had poor knowledge regarding antibiotic resistance and only few teachers had basic orientation.26 They recommended to utilise the keen interest of high school students to orient them regarding antibiotic usage and prevention of antimicrobial resistance. Bharani Krishna et al, noted more than 96% of the students have knowledge and good attitudinal orientation for antimicrobial resistance prevention.27KanikaKhajuria et al also noted similar results among second year medical undergraduate students.28
All these recent studies variably mention the knowledge, attitude and practice gaps in the antimicrobial resistance prevention in the health care sector. As mentioned earlier, for effective antimicrobial stewardship program, overt knowledge and attitude of the doctors regarding the development of resistance, pharmacological basis of antimicrobial selection, dosing pattern, microbiological supporting data, de-escalation end point definitions are of immense importance. These aspects of infectious condition management, even though dealt in detail during formative undergraduate training, if reinforced during internship and during post-graduation course, may serve as effective tools in stronger antimicrobial stewardship program.
With these things in background, a short education module highlighting the development of antimicrobial resistance, treatment of resistant microbial conditions and prevention of antimicrobial resistance was used in the present study. Didactic lectures and interactive lectures to large extent do not necessarily bring about attitudinal and transformative changes. Content delivery on a mobile platform with appropriate instructional design can not only bring about effective interactive learning but also the desired outcomes. World Health Organisation (WHO) and Centre for Disease Control (CDC) have initiatives to acquire antimicrobial stewardship competency through online courses.
There are no such short course available in India for willing stakeholders to revise, revisit and fine tune concepts of antimicrobial resistance that play a pivotal role in antimicrobial stewardship program. Through this study, an attempt was made to develop and deploy an online short module for improving knowledge and attitude about the antibiotic resistance among busy doctors.
Objectives
The main objective of the study was to evaluate the knowledge and attitudes regarding antibiotic resistance among medical doctors in a tertiary care hospital. The other objective was to evaluate the usefulness of the interactive educational intervention in improving the knowledge about antibiotic resistance.
Methodology
Study Design
Cross sectional questionnaire based studyinvolving residents and postgraduates from various departments in our medical college.
Inclusion criteria
All interns and postgraduates of all clinical departments who consented to take part in the study.
Exclusion criteria
All other medical students, teaching faculty of pre, para and clinical departments were excluded. Those who fail to take the post-test were also excluded from the final analysis.
Study instrument
Questionnaire
After obtaining ethics committee approval, a structured, pilot tested, validated questionnaire was distributed to all medical doctors in a tertiary care hospital. The baseline knowledge about the modes of development of antimicrobial resistance, methods of treatments and modes of prevention were assessed initially.
Questionnaire components
Questionnaire had three categories of assessment, namely, knowledge about the development of antimicrobial resistance (fifteen questions), treatment of resistant microbial conditions (five questions) and prevention of antimicrobial resistance (five questions). Several questions were adopted from similar studies in the past with considerable changes.24,29The questionnaire components were tested by two subject experts in the department of Pharmacology, other than the guide of the study. Later, the questionnaire was pilot tested among total five senior residents belonging to Department of General Medicine and General Surgery. The doctors’pilot testing the questionnaire were not included in the final list of participants for the study. A Cronbach’s alpha score of more than 0.8 indicated an internal consistency during validation.
Administration of questionnaire
Each participant was explained the objective of the study and a written informed consent was obtained before administering the questionnaire as pre-test. The pre-test defined the baseline knowledge and attitude of doctors regarding antibiotic resistance.
Interactive educational intervention
After filling up of the questionnaire, each participant or a group of three or four participants were provided with interactive educational intervention. In each such session, three components were discussed using a custom designed course module using a learning management system (Moodle). The course design was such that it followed the Knowles’s six principles of adult learning. The student investigator & the guide participated in each session. Emphasized components were.
The modes of development of antimicrobial resistance
Methods of rationale antimicrobial prescription
Interventions to prevent development of antimicrobial resistance
Such interactive educational intervention differs from regular awareness programs as it concentrates on examples from individual practices and also specific strategies towards antibiotic stewardship. The instructional design of the online learning module was set up in a way that the participant can complete all the built-in tasks in less than 90 minutes. Immediately after the completion of the course, participants filled a post-test questionnaire (same questions as of pre-test). Feedback was collected about the intervention.
Description of Educational Intervention
The online contents had two modules to understand antimicrobial resistance and emphasis measures to prevent the antimicrobial resistance. The first module, concentrated on mechanisms of antimicrobial resistance and their pharmacological basis. The second module, concentrated on measures to be taken to prevent antimicrobial resistance.
The learning objectives of the first module were:
To define appropriate empiric antimicrobial prescribing
To highlight mechanisms by which microorganisms develop antimicrobial resistance
To understand the influence of pharmacodynamic& pharmacokinetic factors in development of drug resistant strains of microbes
To understand the principles of antimicrobial selection for a specific infectious condition.
Module one subsections were – definition of AMR, mechanisms of AMR, spread of AMR, multidrug resistant, pan drug resistant, extremely drug resistant organisms with examples. In this section short introduction to anti-fungal resistance, anti-viral resistance and anti-malarial resistance was also attempted. The content in each of these subsections had equal weightage of text and images. Extensive and lengthy videos were avoided.
The learning objectives of the second module was:
To enumerate basic steps of prevention of antimicrobial resistance
Module two subsections were – prescription writing, antimicrobial selection, prevention of AMR, antimicrobial stewardship program. After the section on selection of antimicrobial, a short section of interactive recollection of these drugs was attempted to evaluate the user engagement. The results of this interactive quiz was not analysed, however, instant feedback to the users provided instant assessment of their learning.
Follow up
The inter ventional educational impact was studied after one month of the initial intervention by a post-test. The same questionnaire was used during the post-test. Those who failed to participate in the post-test were excluded from final analysis.
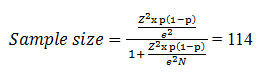
Sample size calculation
There are 160 interns and postgraduates in our tertiary care hospital. With a 95% confidence interval (z score of 1.96) and 5% margin of error, the sample size was calculated as
Statistical Analysis
The data was tabulated and analysed using MS Excel. All continuous data were expressed as mean with standard deviation.The pre-test and post-intervention scores regarding knowledge of antimicrobial resistance were checked by Fisher exact test. The overall effect of interactive educational intervention among interns and postgraduates were compared by Mann–Whitney U-test and values <0.05 were considered significant.
Results
Out of 125 interns and postgraduates who consented to take part in the study, 120 doctors completed the pre-test questionnaire. The pre-test score observations are tabulated in Table 1. The average score was 11.65 ± 3.6 marks out of 25.
Table 1: Parameters of pre-test and post-test outcomes of the study questionnaire.
|
Parameter |
Pre-test |
Post-test |
| Number of participants | 120 | 114 |
| Average score | 11.1 | 20.9 |
| Standard deviation | 3.44 | 2.67 |
| Average score in percentages | 44.65% | 83.24% |
| Standard deviation (%) | 14.4% | 11.13% |
| Score distribution skewness | 0.4662 | -0.7442 |
| Score distribution kurtosis | 0.1954 | -0.2814 |
| Coefficient of internal consistency | 72.37% | 75.40% |
| Error ratio | 41.34% | 48.83% |
| Standard error | 7.8% | 6.55% |
All participants were encouraged to take post-test. However, out of 120 interns and postgraduates who have taken pre-test and course, only 114 could take the immediate post-test. The outcome of the post-test is tabulated in table 1, figure 3 and 4. There is statistically significant increase in the post-test scores in comparison to the pre-test. Maximum scores (n=39) were in higher band of 21.15 to 23.08 in post-test as compared to pre-test, where maximum scores (n=29) was observed between 11.54 to 13.46 (figure ).
 |
Figure 1: Scattered plot graph showing pre-test and post-test values with trendline denoting the mean value. |
The immediate feedback about the course material and instructional design was collected. Only 34 participants have given the feedback. 27 participants agreed that the discussion of the module is related to antimicrobial resistance. Overall rating of the online module was 4.2 ± 0.8 out of 5 for improvement of understanding of antimicrobial resistance.
A few repeated comments are as follows:
Enjoyed doing it
Wonderful effort Keep it up
Need more sessions
It helps me understand more about antimicrobial resistance.
A follow up must be implemented.
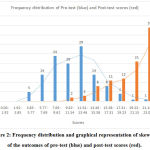 |
Figure 2: Frequency distribution and graphical representation of skewness of the outcomes of pre-test (blue) and post-test scores (red). |
Questionnaire had three categories of assessment, namely, knowledge about the development of antimicrobial resistance (fifteen questions), treatment of resistant microbial conditions (five questions) and prevention of antimicrobial resistance (five questions). The gain of knowledge after the educational intervention as assessed by outcomes during post-test was maximum (statistically significant, p<0.001) for the part one, i.e., knowledge about the development of resistance. Here, the pre-test average score was 6.63 (±0.15) and post-test score was 13.18 (±0.1). Similar improvement was also observed in the selection of antimicrobials and prevention of resistance categories (table 2). Overall, the educational intervention has resulted in the significant improvement in the knowledge regarding development of resistance, selection of the drugs and preventive methods to be followed.
Table 2: Category wise scores pre-test and post-test score of the study questionnaire.
|
Categories in questionnaire |
Part A: Knowledge | Part B: Selection |
Part C: Prevention |
| Pre-test | 6.63 (±0.15) | 1.97 (±0.17) | 2.54 (±0.12) |
| Post-test | 13.18 (±0.1) | 3.83 (±0.08) | 3.91 (±0.05) |
All participants were contacted through the features of learning management system and also through the email IDs. Despite repeated communicative efforts,only 94 participants completed the one-month post-test. One-month post-test was administered through Google forms converted quiz. The average score of the participants in this one-month post-test was 16 out of 25 with standard deviation on 4.79. The results were statistically significantly more than the pre-test score, however statistically lower than immediate post-test score.
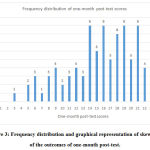 |
Figure 3: Frequency distribution and graphical representation of skewness of the outcomes of one-month post-test. |
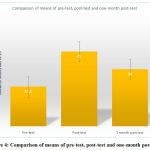 |
Figure 4: Comparison of means of pre-test, post-test and one-month post-test. |
Discussion
Many researchers have identified the gap in knowledge, attitude and practices among doctors and other health care providers with regard to antimicrobial resistance prevention. To address this gap and to strengthen individual hospital or institutional antibiotic stewardship program, effective educational interventionis needed. To promote competency development in clinicians with respect to antimicrobial stewardship program and to adhere to guidelines during management of common clinical scenarios, WHO has developed a 8 hour self-paced learning module comprising of 14 subsections.30 However, with the busy schedule of the doctors, the longer duration and self-paced courses meet larger attrition rates. Similar, paid and free course are being offered by Stanford centre for continued medical education,31 University of Dundee32 and Centre for Disease Control.
Indian Council of Medical Research (ICMR) has formulated Antimicrobial Stewardship Program Guidelines. However, there are no specific online learning materials specifically addressing our doctors. Courses and modules designed according to the local needs and limitations of Indian health care system is the need of the hour. Linking such online modules to general continued medical education program specially designed one each for primary, secondary and tertiary health care physicians shall lead to improved training and orientation of all the doctors. In turn better antimicrobial stewardship program implementation in each hospital set-up and reduced antibiotic costs. In this regard, the present study design where an online module that is much shorter and more specific to the local needs caters much-required gaps in the busy clinicians’ antimicrobial therapy.
In the present study, there is significant improvement in the learning outcomes after exposure to the online learning module. Every guideline about the antimicrobial stewardship program recommends that the physician and pharmacist be fully trained in the infectious diseases with complete support from the microbiology team. Between two approaches for effective stewardship program, even though post-prescription audit and feedback appears an easy approach (especially in resource constrained environment), here as well the knowledge about the antimicrobial selection, susceptibility pattern, dose and duration with de-escalation end points are quiet important.The present study mainly concentrating on the development of the online material for training the clinicians in better implementation of the antibiotic stewardship program. In addition, the material used in the present study even though it is self-admissible and self-paced, presence of the principal investigator in every session along with the guide made learning not only assisted but also partially supervised.
In the present study, the average pre-test score are significantly lower. The pharmacological basis of the antimicrobial resistance is included along with the curriculum of second year of undergraduate training. Through the pre-test scores of this study, it is evident that the interns and post-graduates considerably unable to summon up the original concepts of development of antimicrobial resistance over years. The authors of this study urge that the concepts of antimicrobial selection and preventive methods must be continuously reinforced along the third and final year of undergraduate training.
At the end of the study, the knowledge and attitudes of medical doctors regarding the antibiotics resistance especially modes of development of resistance, methods to reduce the emergence of further resistance were evident. At the same time, the effectiveness of interactive educational intervention using infographics and individual interactions werealso evaluated at the end of 1 month. It is expected that the knowledge gained by such educative intervention will be translated into a responsible and judicial usage of antibiotic and lead to lesser emergence of resistance. Such awareness evaluations, leads to effective and efficient and formulation of hospital based antibiotic stewardship programs aiming at better antibiotic usage.
During the study, the difficulties encountered were related to busy schedule of the post-graduates and interns. Even though the entire course could have been administered in less than 90 minutes, many participants did not show inclination even for mobile content design. The modules used in the study, generally addresses the visual learners. The learning methodology choices and impact of teaching-learning aid varies with different modes of learners. All the participants cannot be uniformly addressed with a single type of learning module. This impacts of the retention of the concepts. Such disparity is apparent with lesser mean scores of the one-month post-test.
The learning management system deployed to host the course content used login ID and passwords for each participants to safely, securely and individually go through the course content and store individual grades in pre-test and post-test. After one-month, with fading enthusiasm and interest in the online learning module, many participants demanded new IDs and passwords to login to access the one-month retention test. To overcome this login problem, the same questions were distributed in the same order with the changes in order of the choices through Google forms. These Google forms analysed overall score of the participants.
Though this study has effectively showed that there is intrinsic lacunae in the understanding of the concepts of antimicrobial resistance, selection of the antibiotics and resistance preventive methods, it may not be generalized as it is a single institution based study. Moreover, the questionnaire components and concepts addressed in the study do not comprehensively represent the all the components of anti-microbial resistance stewardship.
Conclusions
Use of the interactive online learning material has result in significant improvement in the knowledge and attitude regarding antibiotic resistance among post-graduates and interns in a tertiary care hospital.
Acknowledgements
Authors thank all the participants who have undertaken this survey. Authors also thank Management and Principal of Azeezia Institute of Medical Sciences and Research for allowing us to conduct the survey. We thank the interns and postgraduates who have actively participated in this study.
Conflict of Interest
Authors declare no conflict of interest.
Funding source
Authors have not received any funding for this study.
References
- World Health Organization. World Antibiotic Awareness Week 2018: “Change can’t wait. Our time with antibiotics is running out” [Internet]. https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance. 2018 [cited 2019 Jan 10]. Available from: https://www.who.int/campaigns/world-antibiotic-awareness-week/2017/posters/time-running-out.pdf
- World Health Organization. ‘Super’ Gonorrhoea: Q&A with Dr. TeodoraWi [Internet]. https://www.who.int. [cited 2019 Jan 10]. Available from: https://www.who.int/who-campaigns/world-antibiotic-awareness-week/world-antibiotic-awareness-week-2018/features-from-around-the-world/super-gonorrhoea-q-a-with-dr.-teodora-wi
- World Health Organization.Advocacy material [Internet]. https://www.who.int. 2018 [cited 2019 Jan 10]. Available from: https://www.who.int/who-campaigns/world-antibiotic-awareness-week/world-antibiotic-awareness-week-2018/advocacy-material
- Center for Disease Control and Prevention.Core Elements of Hospital Antibiotic Stewardship Programs | Antibiotic Use | CDC [Internet]. https://www.cdc.gov/antibiotic-use/healthcare/index.html. 2017 [cited 2019 Jan 9]. Available from: https://www.cdc.gov/antibiotic-use/healthcare/implementation/core-elements.html
- Barlam TF, Cosgrove SE, Abbo LM, MacDougall C, Schuetz AN, Septimus EJ, et al. Implementing an Antibiotic Stewardship Program: Guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis Off Publ Infect Dis Soc Am. 2016 May 15;62(10):e51–77.
CrossRef - Kapoor G, Saigal S, Elongavan A. Action and resistance mechanisms of antibiotics: A guide for clinicians.J AnaesthesiolClinPharmacol. 2017 Jul 1;33(3):300.
CrossRef - Munita JM, Arias CA. Mechanisms of Antibiotic Resistance. MicrobiolSpectr. 2016;4(2).
CrossRef - Lerminiaux NA, Cameron ADS.Horizontal transfer of antibiotic resistance genes in clinical environments. Can J Microbiol. 2019 Jan;65(1):34–44.
CrossRef - Mathur P, Singh S. Multidrug Resistance in Bacteria: A Serious Patient Safety Challenge for India. J Lab Physicians. 2013;5(1):5–10.
CrossRef - Hawkey PM, Warren RE, Livermore DM, McNulty CAM, Enoch DA, Otter JA, et al. Treatment of infections caused by multidrug-resistant Gram-negative bacteria: report of the British Society for Antimicrobial Chemotherapy/Healthcare Infection Society/British Infection Association Joint Working Party.J AntimicrobChemother. 2018 Mar 1;73(suppl_3):iii2–78.
CrossRef - Calfee DP. Methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci, and other Gram-positives in healthcare.CurrOpin Infect Dis. 2012 Aug;25(4):385–94.
CrossRef - Fair RJ, Tor Y. Antibiotics and Bacterial Resistance in the 21st Century. Perspect Med Chem. 2014 Aug 28;6:25–64.
CrossRef - V. Balaji, Priscilla Rupali, KaminiWalia, V C Ohri. Antimicrobial Stewardship Program Guideline [Internet].Indian Council of Medical Research; 2018. Available from: https://www.icmr.nic.in/sites/default/files/guidelines/AMSP.pdf
- R. K. Srivastava. National Policy for containment of antimicrobial resistance, India 2011.[Internet]. Directorate General of Health Services, Ministry of Health and Family Welfare.; 2011. Available from: https://mohfw.gov.in/sites/default/files/3203490350abpolicy%20%281%29.pdf
- Gerding DN. The search for good antimicrobial stewardship.JtComm J QualImprov. 2001 Aug;27(8):403–4.
CrossRef - Joseph J, Rodvold KA.The role of carbapenems in the treatment of severe nosocomial respiratory tract infections.Expert OpinPharmacother. 2008 Mar;9(4):561–75.
CrossRef - Doron S, Davidson LE. Antimicrobial Stewardship. Mayo Clin Proc. 2011 Nov;86(11):1113–23.
CrossRef - Costelloe C, Metcalfe C, Lovering A, Mant D, Hay AD. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis.BMJ. 2010 May 18;340:c2096.
CrossRef - Cosgrove SE, Sakoulas G, Perencevich EN, Schwaber MJ, Karchmer AW, Carmeli Y. Comparison of mortality associated with methicillin-resistant and methicillin-susceptible Staphylococcus aureus bacteremia: a meta-analysis. Clin Infect Dis Off Publ Infect Dis Soc Am. 2003 Jan 1;36(1):53–9.
CrossRef - Tiwari SA, Ghongane BB, Daswani BR, Dabhade SS. Restricted Parenteral Antibiotics Usage Policy in a Tertiary Care Teaching Hospital in India. J ClinDiagn Res JCDR. 2017 May;11(5):FC06–9.
CrossRef - Tamma PD, Avdic E, Keenan JF, Zhao Y, Anand G, Cooper J, et al. What Is the More Effective Antibiotic Stewardship Intervention: Preprescription Authorization or Postprescription Review With Feedback? Clin Infect Dis Off Publ Infect Dis Soc Am. 2017 01;64(5):537–43.
- Cheng VC, Wong SC, Ho P-L, Yuen K-Y. Strategic measures for the control of surging antimicrobial resistance in Hong Kong and mainland of China. Emerg Microbes Infect. 2015 Jan 1;4(1):1–13.
CrossRef - Nair M, Tripathi S, Mazumdar S, Mahajan R, Harshana A, Pereira A, et al. Knowledge, attitudes, and practices related to antibiotic use in PaschimBardhaman District: A survey of healthcare providers in West Bengal, India. PLOS ONE. 2019 May 31;14(5):e0217818.
CrossRef - Badar V, Parulekar VV, Garate P. Study of knowledge, attitude and practice amongst medical professionals about antimicrobial stewardship in tertiary care teaching hospital in India: a questionnaire based study. Int J Basic ClinPharmacol. 2018 Feb 22;7(3):511–7.
CrossRef - Mahajan DMM, Dudhgaonkar DS, Deshmukh DSN. A Questionnaire based Survey on the Knowledge, Attitude and Practises about Antimicrobial Resistance and Usage among the Second year MBBS Students of a Teaching tertiary care Hospital in Central India. Int J Pharmacol Res. 2014 Dec 30;4(4):175–9.
- Kotwani A, Wattal C, Joshi PC, Holloway K. Knowledge and perceptions on antibiotic use and resistance among high school students and teachers in New Delhi, India: A qualitative study. Indian J Pharmacol. 2016 Jul 1;48(4):365.
CrossRef - Bharanikrishna Y, SasiSekhar TVD, Hanumanth N, LalithaPalaparthi. A KAP Study Regarding Anti Microbial Resistance Among Medical Students In South India. IOSR J Dent Med Sci IOSR-JDMS. 2015;14(4):110–3.
- Khajuria K, Kaur S, Sadiq S, Khajuria V. KAP on antibiotic usage and resistance among second professional medical students. Int J Basic ClinPharmacol. 2018 Dec 24;8(1):68–73.
CrossRef - Jayabalan N, Selvaraj N, Ganesan S, Rajamohammad MA, Anandan I. A questionnaire based survey on knowledge, attitude and behaviour of antibiotic usage and resistance among undergraduates in South Indian teaching hospital. Int J Basic ClinPharmacol. 2018 Sep 24;7(10):1991–7.
CrossRef - Marisa Holubar, Stan Deresinski, Elizabeth Robilotti, TjallingLeenstra, Muna Abu Sin, HrachuhiGhazaryan, et al. Antimicrobial Stewardship: A competency-based approach [Internet].OpenWHO. [cited 2019 Oct 25]. Available from: https://openwho.org/courses/AMR-competency
- Stanford Antimicrobial Safety and Sustainability Online CME Courses [Internet].Stanford Center for <br>Continuing Medical Education. [cited 2019 Oct 25]. Available from: https://med.stanford.edu/cme/learning-opportunities/antimicrobialstewardship.html
- DilipNathwani. Antimicrobial Stewardship – Online Course [Internet].FutureLearn. [cited 2019 Oct 25]. Available from: https://www.futurelearn.com/courses/antimicrobial-stewardship