Manuscript accepted on :7-Dec-2020
Published online on: --
Plagiarism Check: Yes
Reviewed by: Dr. B.Surendiran
Second Review by: Dr. Mohamed Ali
Final Approval by: Dr. Francesca Gorini
Husam Jihad Imran1* , Samer Abdulameer Dhaher2
, Samer Abdulameer Dhaher2  and Abbas Ali Mansour3
and Abbas Ali Mansour3
1Department of Adult Endocrinologist. Faiha Specialized Diabetes, Endocrine, and Metabolism Center (FDEMC), University of Basrah, Basrah,Iraq.
2Depardment of dermatology, University of Basrah, Basrah, Iraq.
3Department of Medicine, Consultant Endocrinologist.Faiha Specialized Diabetes, Endocrine, and Metabolism Center (FDEMC), University of Basrah, Basrah, Iraq.
Corresponding Author Email: husam_imran@yahoo.com
DOI : https://dx.doi.org/10.13005/bpj/2056
Abstract
Background:Hirsutism is a distressing medical problem for women. Most of hirsutism in women is associated with excess androgen, and most cases have PCOS as an underlying cause.Which androgen to be used to evaluate clinical or biochemical hyperandrogenism in women with PCOS is still debated.There are a small number of studies that evaluated androgens in women with PCOS having hirsutism with conflicting results. The Objective of this study was to determine which androgen predict hirsutism in women with polycystic ovary syndrome (PCOS). Patients and Methods:A case-control study was done in Faiha Specialized Diabetes, Endocrine, and Metabolism Center (FDEMC), Basrah, Iraq. A total of 130 women with PCOS (based on Rotterdam criteria) and 70 healthy controls of comparable age (16-40 years) were investigated for androgens (total testosterone, free testosterone, DHEA-S) using Electrochemiluminescence technology assay; excess hair was examined according to the modified Ferriman-Gallwey (mFG) score and a cut-off value of 8 defined hirsutism. Results: In the three groups of women, the first (n=100) included PCOS with hirsutism, the second (n=30) PCOS without hirsutism, and the third (n=70) women without PCOS or hirsutism as healthy control, hirsutism was seen in about 77 % of PCOS women mostly of moderate severity; High TT, FT, DHEA-S, and overall androgens were seen in 69%, 76%, 37%, and 99% respectively of our PCOS women with hirsutism. No correlation was found between TT, FT, and DHEA-S and the mFG score. Conclusions: This study provides evidence that presence of hirsutism in women with PCOS was associated with a higher level of biochemical hyperandrogenism than seen in PCOS without hirsutism; however, there was no correlation between the studied androgens and mFG score.
Keywords
Biochemical Hyperandrogenism; DHEA-S; Hirsutism; Polycystic Ovary Syndrome; Testosterone
Download this article as:| Copy the following to cite this article: Imran H. J, Dhaher S. A, Mansour M. A. A. Testosterone or Dehydroepiandrosterone Sulfate as A Biomarker for Hirsutism in Women with Polycystic Ovary Syndrome. Biomed Pharmacol J 2020;13(4). |
| Copy the following to cite this URL: Imran H. J, Dhaher S. A, Mansour M. A. A. Testosterone or Dehydroepiandrosterone Sulfate as A Biomarker for Hirsutism in Women with Polycystic Ovary Syndrome. Biomed Pharmacol J 2020;13(4). Available from: https://bit.ly/2KiTRQK |
Introduction
Hirsutism is adistressing medical problem for women.Overall, it affects about 5-15% of women(1), it is usually associated with cosmetic concern, emotional distress, and depression(2), and is typically a feature of an underlying condition mostly of hormonal disturbance origin(3).Hirsutism can be described as terminal (thick and dark) hair in the face and /or body of women in areas usually having little or no hair (1).In 1981, Hatch, Rosenfield, Kim, and Tredway revised the initialvisual score thatintroducedin 1961 by Ferriman and Gallwey, where nine body areas used, each is graded from nil (no substantial terminal hair growth) to four (considerableterminal hair growth) and then added up to a totalscoreof themodified Ferriman-Gallwey(mFG), which is the standard scoring scale for hirsutism currently in use.(4).
Most of hirsutism in women is associated with excess androgen (up to 85%), and most cases (around 70 – 80%) have PCOSas an underlying cause.Other causes of hirsutism constitute about 10 – 15 % and include idiopathic hirsutism, thyroid dysfunction, hyperprolactinemia, congenital adrenal hyperplasia, Cushing disease, acromegaly, ovarian and adrenal tumors(5).
PCOS is an endocrine condition observed during the fertile life of females, with a 6 – 15 % prevalence that varies accordingto the diagnostic criteria used (6). Hyperandrogenism, chronic anovulation, and polycystic ovarian morphology(PCOM)are characteristic of PCOS(7).
The European Society for Human Reproduction and Embryology (ESHRE) and the American Society for Reproductive Medicine (ASRM) have proposedthe PCOS diagnosis needs two out of the following three features- theRotterdam criteria(8)
Ovulatory dysfunction refers to oligomenorrhea (cycles approximately 35 days apart or nine cycles or less peryear) or amenorrhea (absence of menstruation 6 to 12 months after a cycle). Clinical or biochemical hyperandrogenemia.
Polycystic ovaries (as described on ultrasonography): 12 or more follicles in at least one ovary with a diameter of 2-9 mm and/ora total volume of an ovary greater than 10 mL.
Before diagnosing PCOS, disorders can lead to ovulatory dysfunction such as hyperprolactinemia and thyroid dysfunction, and those withandrogen excess,including non-classic congenital adrenal hyperplasia (NC-CAH), should be omitted.In women, theovaries release androstenedione,T, anddehydroepiandrosterone(DHEA)under the influence of pituitary luteinizing hormone (LH); the adrenal glands produce androstenedione, T, DHEA, and dehydroepiandrosterone sulfate (DHEA-S) under the control of pituitary adrenocorticotropic hormone (ACTH).In peripheral tissues (liver, skin, and adipose tissue), the androstenedione and DHEA(ovaries and adrenals), and DHEA-S (adrenals) can be converted into T.Approximately 98 – 99 % of circulating T is bound to sex hormone-binding globulin (SHBG) and albumin; the remainder1-2 % is the free testosterone (FT), which is bioactive androgenthat will be converted into DHT by the 5alpha-reductase enzymes in the target tissue. This DHT has a higher affinity for androgen receptors found in the dermal papilla cells and the hair follicle’s outer root sheath to produce longer thick hair(9).
The suggested fundamental physiological abnormality in women with PCOS is the increased intensity and frequency of the LH pulse caused by increased pulsatile gonadotropin-releasing hormone (GnRH) secretion, resulting indirect stimulation of ovarian theca cells to generate androgens (7).In 2008, the Endocrine Society proposed testing women with abnormally high mFG score for elevated androgen levels(10).In 2012, the Androgen Excess and Polycystic Ovary Syndrome Society (AE-PCOS) also recommended hormonal analysis for women with a highhirsutism score (1).There are a small number of studies that evaluated androgens in women with PCOS having hirsutism with conflicting results(11-13).The study aims to investigate TT, FT, and DHEA-S as biochemical markers for hirsutism in women with PCOS.
Patients and method
Design and participants
A case-control study was conducted on 200 women of reproductive age (16-40 years) at Faiha Specialized Diabetes, Endocrine, and Metabolism Center (FDEMC) in Basrah, Iraq from September 2019 to September 2020. It was composed of three groups: the first group (n=100) included women with PCOS and hirsutism, the second group (n=30) women with PCOS but no hirsutism, and the third group (n=70) women without PCOS or hirsutism as healthy control (Figure1).
Basrah College of Medicine Ethics Committee had approved the study protocol, and participants gave written informed consent.
Pregnant and lactating women were excluded as patients with liver and kidney diseases.
Clinical evaluation
Participants medical history focused onage at menarche,childbearing history, menstrual cycle length, and regularity, presence ofgalactorrhea,the appearance of excess hair in the face and body, and the use of medications that may affect hormone parameters during the lastthree months prior entering the study like oral contraceptive pillsand glucocorticoids. Bodyweight(kg) and height(cm) were measured, andbody mass index (BMI) was calculated by the Quetelet’s Index formula. Physical examination included assessing the amount and distribution of terminal hair according to the mFG score by the same trainednurse(14).Women who had removed the excess hair were informed to come later for a more reliable hair score assessment (12 weeks after laser therapy, four weeks after depilation or waxing, and five days after shaving)(15).PCOS diagnosis was proposed by the Rotterdam criteria(8).Ovulatory dysfunction was labeled as oligomenorrhea (cycles ≥ 35 days apart or ≤9 cycles per year) or amenorrhea (absence of menses for 6 -12 monthsafter an established cycle) (16).The study definedhyperandrogenism clinically bythe presence of hirsutism with the mFG score equal to or more than 8(5).PCOM was determined by transabdominal pelvic ultrasonography.The diagnosis of PCOS was only made after excluding hyperprolactinemia, thyroid dysfunction, Cushing’s syndrome, andNC-CAH by relevant clinical and laboratory analysis, including prolactin (PRL), thyroid-stimulating hormone (TSH), cortisol, ACTH, and 17-hydroxyprogesterone(17-OHP).
Laboratory tests
Basal Hormone Measurement
On the second to the seventh day of menses (for women with regular menstrual cycles or at any day for those with irregular ones), fasting venous blood samples (4 mL in clot-activator gel tube and 3 mL in EDTA tube) were collected at 8:00-10:00 am. After separation by NUVE-NF 800 at 4100 RPM, TT, DHEA-S, PRL, SHBG, TSH, cortisol, ACTH, and albumin were tested by Electrochemiluminescence (ECL) technology assay (Cobas e 411analyzer-Roche, Germany), 17-OHP was measured by Enzyme-linked immunosorbent assay (ELISA) method (BioTek-USA).Our study normal androgens level were 15-46 ng/dL for TT(≤ 6% CV), 0.13-0.56 ng/dL for calculated FT(<6% CV), and 18-86 nmol/L for SHBG(< 4% CV)(17).FT was calculated from TT, SHBG, and albumin, according to the Vermeulen equation(18).Reference ranges for other hormonal parameters used were thoseof the FDEMC laboratory;DHEA-S 145-395 µg/dL(<5%CV) for women age 18-19, 65-380 µg/dL for women ages 20-29,45-270 µg/dL for women ages 30-40,PRL 4-30ng/mL(≤5%CV), TSH 0.27-4.2µIU/mL(<5%CV), cortisol 5-25 µg/dL (<6%CV), ACTH 10-60 pg/ mL(<5%CV),and 17OHP ≤495ng/dL (<10%CV).
Ovarian Ultrasonography
The sameradiologist examined the participants for PCOMusing a 4.0 MHz trans-abdominal transducer.The presence of PCOM was based on visualization of ≥12 follicles in one ovary measuring 2-9 mm in diameter over the peripheral stroma, and/or increased an ovarian volume of 10 mLor more at day two-seven of mensuration in women with regular menstrual cycles or at any day for those with irregular menses(19).In our study, the ultrasonic exanimation of the pelvis wastransabdominal, not the trans-vaginal one.
Statistical Analyses
Statistical analysis was done by Statistical package for social science software (SPSS Inc. Chicago, IL, USA) version 25.Using the Kolmogorov – Smirnov method, we tested the distribution of all continuous variables. Since the data were normally distributed, continuous variables were presented as mean ± standard deviations.Different study group’s means were compared using the ANOVA with post hoc. Categorical variables were summarized in number and percentage.A Chi-square test and Fishier Exact test were used to compare categorical groups.Correlations between continuous variables were analyzed with Pearson’s correlation. P-value <0.05 was considered statistically significant.
Results
The features of the 200 participants included in the study are presented in Table1. The mean age (±SD) for the first group (women with PCOS and hirsutism) was 24 (±6), for the second group (women with PCOS without hirsutism) was 26 (±8), and for the third group (women without PCOS or hirsutism) was 26(±7)with no significant difference among the groups (p=0.17), so the three groups of participants were age-matched.BMI for the first group was 32(±5.9), for the second group was 27.4 (±3.5), and for the third group was 26.9 (±5.7), with a significant statistical difference of the first group from the second and third (<0.001), and between the first and third groups(<0.001), but there was no significant difference between the second and third groups (p=0.6). Hirsutism score for the first group was 19 (± 5), for the second group was 5 (± 2) and for the third group was 3 (± 2), with a significant statistical difference of the first group from the second and third (<0.001), and between the first and third groups(<0.001), and there was a significant difference (< 0.01) between the second and third groups.
Table 1: Age,BMI and hirsutism score ofstudy groups n=200.
| Variables
|
PCOS with hirsutism
n=100 |
PCOS with no hirsutism
n=30 |
no PCOS, no hirsutism
n=70 |
p-value |
| Mean± SD | Mean± SD | Mean± SD | ||
| Age (years) | 24±6 | 26±8 | 26±7 | 0.17 |
| BMI (kg/m2) | 32±5.9 | 27.4±3.5 | 26.9±5.7 | <0.001 |
| mFG score | 19 ± 5 | 5 ± 2 | 3 ± 2 | <0.001 |
| PCOS, polycystic ovary syndrome; SD, standard deviation; BMI, body mass index; mFG, modified Ferriman-Galloway. | ||||
The mean TT (±SD), for the first group, was 50.2ng/dL (±10), for the second group was 39.3ng/dL (±6.3) and for the third group was 23.7ng/dL (±7.6).The mean FT(±SD), for the first group, was 1.04ng/dL (±0.29), for the second group was 0.43ng/dL (±0.07) and for third one was 0.33ng/dL (±0.10).The mean DHEA-S (± SD), for the first group, was 323.3µg/dL (±99.5), for the second group 209µg/dL (± 68), and the third group was 200.6µg/dL (±63.3), as shown in Table2.
Table 2: The mean of androgens in study groups n=200.
| Androgen | PCOS with hirsutism
n=100 |
PCOS with no hirsutism
n=30 |
no PCOS, no hirsutism
n=70 |
p-value |
| Mean± SD | Mean± SD | Mean± SD | ||
| TT (ng/dL) | 50.2±10 | 39.3±6.3 | 23.7±7.6 | <0.001 |
| FT (ng/dL) | 1.04±0.29 | 0.43±0.07 | 0.33±0.1 | <0.001 |
| DHEA-S (µg/dL) | 323.3±99.5 | 209.8±68 | 200.6±63.3 | <0.001 |
| PCOS, polycystic ovary syndrome; SD, standard deviation; TT, total testosterone; FT, free testosterone; DHEA-S, dehydroepiandrosterone sulfate. | ||||
The post hoc tests of mean androgen comparison of the study groups revealed the following: for TT, there was a significant difference between the first group and the second group (<.001), and between the first group and the third one (<0.001). Also, there was a significant difference between the second group and the third one (<.001).
Regarding FT, again, there was a significant difference between the first group and second group (<0.001), and between the first group and the third one (<0.001), but there was no significant difference between the second and third groups (p=0.52).
In the case of DHEA-S, there was a significant difference between the first group and second group (<0.001) and between the first group and the third one (<0.001). But, no significant difference between the second and third groups (p=0.6).
The number of participants witha high androgen level is shown in Table3.In the group of women with PCOS and hirsutism, there were69patients(69%) with high TT, 76patients (76%) with high FT, and 37(37%) patients with high DHEA-S.In women with PCOS and no hirsutism, threepatients (10%) had high TT,and tenpatients(33.3%) had high FT,while none of them had high DHEA-S level.In the group of women without PCOS or hirsutism, none of the participants had an abnormally high TT or FT or DHEA-S.High overall androgens was seen in 84.61 % of women with PCOS (n=130), in99 % of the women with hirsutism, and 36.7% of women with PCOS but no hirsutism enrolled in the study.
Table 3: High Androgens in Participants n=200.
| Androgens level | PCOS with hirsutism
n=100 |
PCOS with no hirsutism
n=30 |
no PCOS, no hirsutism
n=70 |
p-value | |||
| n | % | n | % | n | % | ||
| High TT | 69 | 69 | 3 | 10 | 0 | 0 | <0.001a |
| High FT | 76 | 76 | 10 | 33.3 | 0 | 0 | <0.001b |
| High DHEA-S | 37 | 37 | 0 | 0 | 0 | 0 | <0.001c |
| High overall androgens | 99 | 99 | 11 | 36.7 | 0 | 0 | <0.001d |
| PCOS, polycystic ovary syndrome; TT, total testosterone; FT, free testosterone; DHEA-S, dehydroepiandrosterone sulfate.
a for high TT levels, there was a significant difference between first and second groups (p <0.001). Thesignificance between other groups was not applicable. b for high FT levels, there was a significant difference between first and second groups (p <0.001). The significance between other groups was not applicable. c for high DHEA-S levels, statistical deference calculation was not applicable. dfor any biochemical hyperandrogenism, there was a significant difference between first and second groups (p <0.001). The significance between other groups was not applicable. |
|||||||
For women with PCOS who had hirsutism in the study group, the severity of hirsutism was mild in 29 patients (29%),moderate in 59 patients (59%), and severe in 12 patients (12%).
Figure1. shows the receiver operating characteristic (ROC) curves for androgen marker; the cut-off values determined from the ROC curve together with diagnostic sensitivity and specificity.
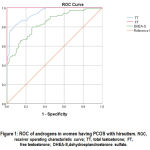 |
Figure 1: ROC of androgens in women having PCOS with hirsutism. ROC, receiver operating characteristic curve; TT, total testosterone; FT, free testosterone; DHEA-S,dehydroepiandrosterone sulfate. |
In our patients, TT showed a ROC curve of a good accuracy (area under the curve AUC = 0.944, SE = 0.013, 95%CI (0.918 – 0.970)and,p<0.001. A TT of 44.3 ng/dL or more had 78% sensitivity and 90% specificity for hirsutism in women with PCOS.
The FT showed a ROC curve with excellent accuracy (area under the curve AUC =1.000, SE=0.0001, 95%CI (1.000-1.000) and p<0.001. An FT of 0.54ng/dL or more had 100% sensitivity and 85% specificity for hirsutism in women with PCOS in the study sample.
While, DHEA-S showed a ROC curve of a good accuracy (area under the curve AUS= 0.839, SE=0.026, 95%CI (0.788-0.891) and p<0.001. A DHEA-S of229 µg/dL or more had 81% sensitivity and 70% specificity for hirsutism in women with PCOS in the study sample. A negligible correlation was noted betweenthe hirsutism score and measured androgens (TT, FT, and DHEA-S).
The correlation between biochemical markers and hirsutism is illustrated in table4.
Table 4: Pearson correlation between androgen parameters (TT, FT, and DHEA-S).
| Variable
|
r statistics
|
p-value
|
| TT | 0.099 | 0.32 |
| FT | 0.072 | 0.47 |
| DHEA-S | 0.202 | 0.053 |
|
Pearson correlation coefficient; TT, total testosterone; FT, free testosterone;DHEA-S, dehydroepiandrosterone sulfate. |
||
Discussion
Hirsutism is usually a sign of different medical conditions, and PCOS accounts for about 80% of them(1),where it is considered a usefulmarker of biochemical hyperandrogenism(5).In this study, we investigated biochemical markers in women with PCOS to predicthirsutism.The mean age of the enrolled women with PCOS and hirsutism was 24±6 years, which coincided with the finding ofa previous study fromthe same center on womenin Basrah in 2017(20).There was a significant difference in BMI between the group of women with PCOS and hirsutism and other groups (women with PCOS without hirsutism and women in the control group).Asimilar finding of asignificantly higher BMI in 409 women with PCOS than 7057 women in the non-PCOS group was seenin a population-based observational studyin 2013(21).The high prevalence of obesity in our data amongwomen with PCOS may represent an overall obesity trend in our localitypopulation(22).
The mean mFG score for enrolled women in different study groups was comparable to that seen by an Italian study in 2006(23); the difference in means of hirsutism score between the groups of women with no hirsutism in the study although it was statistically significant, but clinically was not significant as the scores were below the cut-off that defined hirsutism used during enrollment.
We observed higher mean values for TT, FT, and DHEA-S in PCOS groups than non-PCOS, which was also seenin Turkish and Italian studies in 2011 and 2016(24, 25).
Women with hirsutism had significantly higherandrogens mean valuesthan women without hirsutism, a finding similar to a studyfromthe Aristotle University of Thessaloniki, Greece,in2013 (26).
The high androgen levels seen in women with PCOS were comparable to a study by Chang and colleagues in 2005,where TT, FT, and DHEA-S were high in about 50%, 88%, and 34% of women with PCOS, respectively(11), and to Ibanez and associates study in2017, whereabout 70% of women with PCOS have elevated FT, and 20 – 30% have high DHEA-S(27).
Women with hirsutism in our data had higherTT, FT, and DHEA-S levels,which were higher than those seen by some authors(28, 29); the different biochemical assay methods used for androgen estimation and different cut-off values used in the studycan explain the diversity in androgens levels.
In a systematic review published in 2006, biochemical hyperandrogenism was found in approximately 60-80% of women with PCOS,which was comparable toour result(30).
The documented strong association between hirsutism and biochemical hyperandrogenism (5) was also seen in our study, where overall high androgens noted in almost all women included with hirsutism.
Hirsutism was identified in aboutthree-quarters of women with PCOS in our study, and this was consistent with similar studies from Saudi Arabia and Turkey(12, 31).Hirsutism was mild in one-third of patients, moderate in about two-third, and severein less than one-fifth of patients, which was also seen by Chhabra and co-workers in2012who founded mild hirsutism in 32.5%, moderate scores in 52.5%, and a severe degree in 15% (32).
Although the DHEA-S role in PCOS is not yet well clarified,several studies have documented high DHEA-S in about 20-30 percent of patients with PCOS, which was consistent with our findings. However, this does not necessarily reflect an excess adrenal function; it may result from DHEA conversionor represent an inherited genetic abnormality, so interpretation needs caution(33).
An Italian cross-sectional study in 2016 showed thatthe percentages of women with PCOS and hirsutism who had elevatedDHEA-S were higherthan women with PCOSand no hirsutismwith even increasedserum mean values as established in our study(24).
The currentstudycut-off values for TT, FT, and DHEA-S weredifferent from those proposed by the University of Duisburg-Essen in 2007 and a Chinese cross-sectional in 2012 (34, 35).This difference in cut-off values can be explained by eitherdifferent assay methods for androgens measurementorvarious PCOSphenotypes.
No significant correlation was reportedin this study betweenthe androgens (TT, FT, and DHEA-S) and hirsutism score, as was seen in several other studies (13, 23, 24),and this can be explained by the fact that the local androgens level, the sensitivity of the pilosebaceous units, and the activity of androgen receptor are the principaldetermining factorsfor hirsutism severity rather than the level of circulatingandrogens(36).
The study limitations were recruitment of women was from a tertiary referral center and thus may not sufficiently represent the general population, and TT was measured by ECL rather than the liquid chromatography with tandem mass spectrometry method.
Conclusion
Since it demonstrated the highest sensitivity and specificity in the study, we recommend FTas a valuable marker for hirsutism in women with PCOS, even though we couldn’t find a correlation between any of the studied androgens with hirsutism severity.
Aknowlegement
Many thanks for laboratory medical and paramedical staff in Faiha Specialized Diabetes, Endocrine, and Metabolism Center and radiological medical staff in Faiha Teaching Hospital.
Conflict of Interest
Authors do not have any conflict of interest to disclose
Funding Source
A self-funded study done under the authors own expense
References
- Escobar-Morreale HF, Carmina E, Dewailly D, Gambineri A, Kelestimur F, Moghetti P, et al. Epidemiology, diagnosis and management of hirsutism: a consensus statement by the Androgen Excess and Polycystic Ovary Syndrome Society. Hum Reprod Update. 2012;18(2):146-70.
CrossRef - Ekbäck MP, Lindberg M, Benzein E, Årestedt K. Health-related quality of life, depression and anxiety correlate with the degree of hirsutism. Dermatology. 2013;227(3):278-84.
CrossRef - Blume-Peytavi U, Atkin S, Gieler U, Grimalt R. Skin academy: hair, skin, hormones and menopause–current status/knowledge on the management of hair disorders in menopausal women. European Journal of Dermatology. 2012;22(3):310-8.
CrossRef - Blume-Peytavi U. How to diagnose and treat medically women with excessive hair. Dermatologic clinics. 2013;31(1):57-65.
CrossRef - Dennedy MC, Smith D, O’Shea D, McKenna TJ. Investigation of patients with atypical or severe hyperandrogenaemia including androgen-secreting ovarian teratoma. Eur J Endocrinol. 2010;162(2):213-20.
CrossRef - Lauritsen MP, Bentzen J, Pinborg A, Loft A, Forman JL, Thuesen L, et al. The prevalence of polycystic ovary syndrome in a normal population according to the Rotterdam criteria versus revised criteria including anti-Müllerian hormone. Human reproduction. 2014;29(4):791-801.
CrossRef - Rosenfield RL, Ehrmann DA. The pathogenesis of polycystic ovary syndrome (PCOS): the hypothesis of PCOS as functional ovarian hyperandrogenism revisited. Endocrine reviews. 2016;37(5):467-520.
CrossRef - ESHRE TR, Fertility A-SPCWGJ, sterility. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. 2004;81(1):19-25.
CrossRef - Bienenfeld A, Azarchi S, Lo Sicco K, Marchbein S, Shapiro J, Nagler AR. Androgens in women: Androgen-mediated skin disease and patient evaluation. J Am Acad Dermatol. 2019;80(6):1497-506.
CrossRef - Martin KA, Anderson RR, Chang RJ, Ehrmann DA, Lobo RA, Murad MH, et al. Evaluation and treatment of hirsutism in premenopausal women: an Endocrine Society clinical practice guideline. 2018;103(4):1233-57.
CrossRef - Chang WY, Knochenhauer ES, Bartolucci AA, Azziz R. Phenotypic spectrum of polycystic ovary syndrome: clinical and biochemical characterization of the three major clinical subgroups. Fertil Steril. 2005;83(6):1717-23.
CrossRef - Guzel AI, Kuyumcuoglu U, Celik Y. Factors affecting the degree of hirsutism in patients with polycystic ovary syndrome. Arch Gynecol Obstet. 2012;285(3):767-70.
CrossRef - Landay M, Huang A, Azziz RJF, sterility. Degree of hyperinsulinemia, independent of androgen levels, is an important determinant of the severity of hirsutism in PCOS. 2009;92(2):643-7.
CrossRef - Yildiz BO, Bolour S, Woods K, Moore A, Azziz R. Visually scoring hirsutism. Hum Reprod Update. 2010;16(1):51-64.
CrossRef - Ilagan M, Paz-Pacheco E, Totesora DZ, Clemente-Chua LR, Jalique JRKJE, Metabolism. The Modified Ferriman-Gallwey Score and Hirsutism among Filipino Women. 2019;34(4):374-81.
CrossRef - Fraser IS, Critchley HO, Broder M, Munro MG, editors. The FIGO recommendations on terminologies and definitions for normal and abnormal uterine bleeding. Seminars in reproductive medicine; 2011: © Thieme Medical Publishers.
CrossRef - Braunstein GD, Reitz RE, Buch A, Schnell D, Caulfield MP. Testosterone reference ranges in normally cycling healthy premenopausal women. J Sex Med. 2011;8(10):2924-34.
CrossRef - Vermeulen A, Verdonck L, Kaufman JM. A critical evaluation of simple methods for the estimation of free testosterone in serum. J Clin Endocrinol Metab. 1999;84(10):3666-72.
CrossRef - Dewailly D, Lujan ME, Carmina E, Cedars MI, Laven J, Norman RJ, et al. Definition and significance of polycystic ovarian morphology: a task force report from the Androgen Excess and Polycystic Ovary Syndrome Society. Hum Reprod Update. 2014;20(3):334-52.
CrossRef - Hussein RN, Hamdi KIA, Mansour AAJD. The Contribution of New Areas to the Total Hirsutism Scores in Basrah Hirsute Women. 2017;5(4):32.
CrossRef - Moran LJ, Ranasinha S, Zoungas S, McNaughton SA, Brown WJ, Teede HJJHr. The contribution of diet, physical activity and sedentary behaviour to body mass index in women with and without polycystic ovary syndrome. 2013;28(8):2276-83.
CrossRef - Mansour A, Habib OS, Basrah Uo. Overweight and obesity among adults attending medical department. Single center experience in Basrah.
- Amato MC, Galluzzo A, Merlino S, Mattina A, Richiusa P, Criscimanna A, et al. Lower insulin sensitivity differentiates hirsute from non-hirsute Sicilian women with polycystic ovary syndrome. Eur J Endocrinol. 2006;155(6):859-65.
CrossRef - Pasquali R, Zanotti L, Fanelli F, Mezzullo M, Fazzini A, Morselli Labate AM, et al. Defining Hyperandrogenism in Women With Polycystic Ovary Syndrome: A Challenging Perspective. J Clin Endocrinol Metab. 2016;101(5):2013-22.
CrossRef - Coskun A, Ercan O, Arikan DC, Özer A, Kilinc M, Kiran G, et al. Modified Ferriman–Gallwey hirsutism score and androgen levels in Turkish women. 2011;154(2):167-71.
CrossRef - Panidis D, Tziomalos K, Papadakis E, Chatzis P, Kandaraki EA, Tsourdi EA, et al. The clinical significance and primary determinants of hirsutism in patients with polycystic ovary syndrome. 2013;168(6):871-7.
CrossRef - Ibáñez L, Oberfield SE, Witchel S, Auchus RJ, Chang RJ, Codner E, et al. An international consortium update: pathophysiology, diagnosis, and treatment of polycystic ovarian syndrome in adolescence. 2017;88:371-95.
CrossRef - Orio Jr F, Matarese G, Di Biase S, Palomba S, Labella D, Sanna V, et al. Exon 6 and 2 peroxisome proliferator-activated receptor-γ polymorphisms in polycystic ovary syndrome. 2003;88(12):5887-92.
CrossRef - Carmina E, Rosato F, Janni A, Rizzo M, Longo RJTJoCE, Metabolism. Relative prevalence of different androgen excess disorders in 950 women referred because of clinical hyperandrogenism. 2006;91(1):2-6.
CrossRef - Azziz R, Carmina E, Dewailly D, Diamanti-Kandarakis E, Escobar-Morreale HF, Futterweit W, et al. Criteria for defining polycystic ovary syndrome as a predominantly hyperandrogenic syndrome: an androgen excess society guideline. 2006;91(11):4237-45.
CrossRef - Al-Ruhaily AD, Malabu UH, Sulimani RA. Hirsutism in Saudi females of reproductive age: a hospital-based study. Ann Saudi Med. 2008;28(1):28-32.
CrossRef - Chhabra S, Gautam RK, Kulshreshtha B, Prasad A, Sharma N. Hirsutism: A Clinico-investigative Study. Int J Trichology. 2012;4(4):246-50.
CrossRef - Goodarzi MO, Carmina E, Azziz R. DHEA, DHEAS and PCOS. J Steroid Biochem Mol Biol. 2015;145:213-25.
CrossRef - Hahn S, Kuehnel W, Tan S, Kramer K, Schmidt M, Roesler S, et al. Diagnostic value of calculated testosterone indices in the assessment of polycystic ovary syndrome. Clin Chem Lab Med. 2007;45(2):202-7.
CrossRef - Zhou Z, Ni R, Hong Y, Li Y, Wang Y, Zhao X, et al. Defining hyperandrogenaemia according to the free androgen index in C hinese women: a cross‐sectional study. 2012;77(3):446-52.
CrossRef - Chen WC, Zouboulis CC. Hormones and the pilosebaceous unit. Dermatoendocrinol. 2009;1(2):81-6.
CrossRef
(Visited 1,440 times, 1 visits today)







