Manuscript accepted on :25-03-2020
Published online on: 14-08-2020
Plagiarism Check: Yes
Reviewed by: Martin Helan
Second Review by: Pradipta Bhakta
Final Approval by: Dr. Beatrice O. Ondondo
Ayush Pal Bansal, Vivek Chakole, Amol Singam and Basant Singh Latwal
Department of Anesthesiology, Datta Meghe Institute of Medical Science, Sawangi (Meghe), Wardha- 442004, Maharashtra, India
Corresponding Author E-mail: drvivekchakole@rediffmail.com
DOI : https://dx.doi.org/10.13005/bpj/1999
Abstract
Background and objective: Caesarean section is most commonly performed under spinal anaesthesia these days. One of the most common complication of spinal anaesthesia is post spina shivering occurring at the rate of as high as 85% in caesarian section. The present study aims at studying the effect of intrathecal tramadol in prevention of post spinal shivering. Methods: Sixty patients of American Society of Anaesthesiologist Class I and II were randomly divided into two groups and were given either normal saline (Group C) as control group or Tramadol (group T) as study group intrathecally as adjuvant along with Bupivacaine (hyperbaric) for spinal anaesthesia. The patients were monitored for intensity and incidence of shivering. Result: Statistically significant difference was found in the incidence as well as intensity of shivering among the two groups. The tramadol requirement was significantly reduced in the study group and there was no significant difference between the adverse effects seen in both the groups. Conclusion: We found that when tramadol was given intrathecally along with hyperbaric bupivacaine it was found to be effective in countering the side effect of shivering in parturient after spinal anaesthesia. Also, there was no significant difference in side effects like nausea, vomiting and pruritis due to use of tramadol in both the groups.
Keywords
Anaesthesia; Bupivacaine; Caesarian Section; Spinal Anaesthesia; Tramadol
Download this article as:| Copy the following to cite this article: Bansal A. P, Chakole V, Singam A, Latwal B. S. Evaluation of Efficacy of Intra Thecal Tramadol for Prevention of Shivering Post Spinal Anaesthesia in Patients Undergoing Caesarian Section. Biomed Pharmacol J 2020;13(3). |
| Copy the following to cite this URL: Bansal A. P, Chakole V, Singam A, Latwal B. S. Evaluation of Efficacy of Intra Thecal Tramadol for Prevention of Shivering Post Spinal Anaesthesia in Patients Undergoing Caesarian Section. Biomed Pharmacol J 2020;13(3). Available from: https://bit.ly/3fXyez2 |
Introduction
The use of Spinal anaesthesia for caesarean section has revolutionized obstetric anaesthesia. Compared to general anaesthesia, spinal anaesthesia offers reduced maternal mortality, the ability to use fewer drugs, more direct experience of childbirth and the capability to decrease blood loss and provide excellent postoperative pain control.1 However, one of the most common complication of spinal anaesthesia is post spinal shivering which is known to occur at a rate of 56.7 % which increases to 85% in patients undergoing cesarean section under spinal anesthesia.2
Post spinal shivering has been defined as spontaneous, involuntary and oscillatory fasciculations or tremor like hyperactivity of skeletal muscles.3 It varies from a mild form of having skin eruptions to a severe form with generalized continuous skeletal muscle contractions. It is known to have both intra operative and post-operative complications. Intraoperatively it is known to increase the oxygen demand by 200-500 % along with an increase in the carbon dioxide production.4 Thus it may further compromise myocardial function in the pregnant females. Moreover, it is distressing for the patient and interferes with perioperative vital monitoring.4 Post operatively it may contribute to increased wound pain, delayed wound healing and hence a delayed in discharge from the hospital.4
Various non pharmacological and pharmacological therapies like preoperative warming, forced air warming, use of intravenous opioids, ketanserin, propofol, granisetron, doxaparem, physostigmine, clonidine and nefopam has been commonly used but intrathecal use of drugs reduce it’s dosage as well as side effects associated with it.5
Tramadol hydrochloride is a µ opioid receptor agonist which has shown to prevent shivering when given intravenously. Moreover, it’s analgesic property when given intrathecally has been widely studied and it is proven to be safe to mother as well as the fetus when given intrathecally.6
Therefore, the present study was designed to evaluate the efficacy of tramadol as an intrathecal adjuvant in prevention of shivering in caesarian sections when given in a low dose of 20mg.
Method
A prospective randomized double-blind study was conducted in the department of anesthesiology, acharya vinoba bhave hospital sawangi meghe wardha after approval from the institutional ethics committee. We performed this study in patients undergoing elective caesarean section falling in american society anesthesiology class I-II. We excluded patients who didn’t give consent for SAB, any contra indication of Sub Arachnoid Block (SAB), significant cardio respiratory, renal or hepatic impairment, uncontrolled hypertension or diabetes mellitus or on chronic analgesics or vasodilator therapy.
The patients were randomly divided into two groups of 30 each with the help of computer-generated random number table and were allotted the same group through sealed enveloped technique. Group C received 10 mg (2 ml) of Hyperbaric Bupivacaine along with 0.4 ml of injection of NS For SAB. Group T received 10 mg (2 ml) of injection Bupivacaine heavy along with 0.4 ml (20 mg) of tramadol for SAB.
A detailed pre anaesthetic checkup (PAC) was done for every patient. An NBM period of 6 hours was ensured and every patient was given standard aspiration prophylaxis. They were explained about the Visual Analogue scoring (VAS) system at the time of PAC.
After entering the operation theatre monitors were attached to the patient to record baseline parameters like Heart Rate, oxygen saturation and Blood pressure and was continuously monitored by an anaesthesiologist. An 18-gauge IV canula was secured, preloading was intentionally avoided to prevent shivering from excessive fluid. They were maintained at 2 ml/kg/hour which was adjusted according to the hemodynamics of the patient. The OT temperature of 22-24 degree Celsius was maintained and I.V. fluids were maintained at the same temperature. All the patients were covered with a single layer of surgical drapes over chest, arm and abdomen intraoperatively. The IT injectate was prepared aseptically in 2.5 ml syringe outside the operation theatre by an anaesthesiologist who took no further part in the study. The SAB was performed in lateral position in L3- L4 spinal space after confirming free flow of the CSF. The patients were immediately made supine after the SAB and were given a left lateral tilt of 15-20 degree. Patients requiring general anaesthesia due to incomplete or partial block were excluded from the study.
The patients were monitored intraoperatively for the signs of shivering and intensity of shivering was graded using a five-point intensity scale: Grade 0: no shivering, Grade 1: one or more of the following: piloerection, peripheral vasoconstriction and peripheral cyanosis but without visible muscle activity. Grade 3: visible muscle activity in more than one muscle group, Grade 4: gross muscle activity involving the whole body. Injection Tramadol 1 mg/kg i.v. was given if shivering score was ≥2.7 Any hypotension which was defined as mean arterial pressure below 60 mmhg or fall in blood pressure more than 20 % pf the base line value was treated by inj. Mephentermine 6 mg boluses. Bradycardia was defined as heart rate below 60 or fall in H.R. by 20 % of the baseline value and was treated by Inj. Glycopyrrolate 0.2 mg bolus. The time at which the SAB was given was taken as time 0 min and the time at which the final skin suture was taken marked the end of surgery. The patients were continuously monitored for any side effects of the drugs like hypotension, bradycardia, nausea, vomiting, pruritis and respiratory depression. Inj. Ondansetron 4mg iv was given as rescue anti emetic in case of nausea and vomiting.
Statistical Analysis
The mean and standard deviation of the parameters studied during the observation period were calculated for the 2 groups and compared by use of analysis of variance tests. Quantitative data was analysed by student t-test and qualitative data was analysed by Chi-square test. Intragroup comparison was performed with the paired t test. P<0.05 was taken as significant.
Result
60 cases were divided into 2 groups of 30 each. Both the groups were comparable in terms of demographic characteristics like age and sex, ASA grading and duration of surgery. The baseline characteristics like heart rate, mean arterial pressure and SpO2 were also comparable among two groups. [ Table 1]
Table 1: Demographic Data
| GROUP C | GROUP T | P VALUE | |
| AGE | 24.78±3.12 | 25.32±3.26 | 0.514 |
| WEIGHT | 51.32±4.28 | 50.46±5.12 | 0.483 |
| ASA GRADE I
II |
24 (80%)
6 |
21 (70%)
9 |
0.375
0.375 |
| DURATION OF SURGERY(IN MIN.) | 42±6.32 | 44±5.44 | 0.194 |
We found shivering in 17 cases in group C as compared to only 6 in Group T. This shows that incidence of shivering was significantly lower in Group T as compared to Group C [20 % in group T vs 56.66 % in Group C] P value = 0.0038 .[ table 2] Moreover, shivering requiring I.V. tramadol (grade ≥ 2) was significantly lower in Group T as compared to Group C ( 6.66 % in group T vs 30 % in group c p value = 0.0205). [ figure 1]
Table 2: Baseline Parameters
| PARAMETER | GROUP C | GROUP T | P VALUE |
| HEART RATE | 82.40±8.76 | 81.30±9.18 | 0.636 |
| MEAN ARTERIAL PRESSURE | 88.46±10.64 | 86.24±9.28 | 0.392 |
| SpO2 | 99.1±1.2 | 99.4±1.6 | 0.415 |
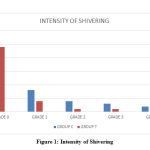 |
Figure 1: Intensity of Shivering |
There was a significant increase in heart rate in Group C as well as group T at 15 minutes after block (Figure 2). This coincided with the peak incidence of shivering in both the groups. [figure 3]
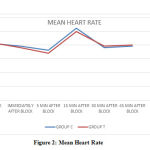 |
Figure 2: Mean Heart Rate |
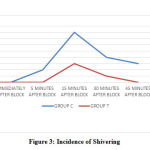 |
Figure 3: Incidence of Shivering |
The incidence of side effects like nausea, vomiting and pruritis were comparable among two groups and were non-significant. [Table 4]
No incidence of respiratory depression was found in any if the group.
Table 3: Tramadol requirement
| GROUP C | GROUP T | P VALUE | |
| TRAMADOL REQUIREMENT ( % OF PATIENT) | 9(30%) | 2 (6.66%) | 0.021 |
Table 4: Side Effects
| SIDE EFFECT | GROUP C | GROUP T | P VALUE |
| NAUSEA | 5 (16.66%) | 8 (26.66%) | 0.351 |
| VOMITING | 2 (6.66%) | 5 (16.66%) | 0.234 |
| PRURITIS | 0 (0 %) | 1 (0.33%) | 0.754 |
Discussion
The cause of shivering post spinal anaesthesia is a common complication and is attributed to peripheral vasodilatation, which results in a core to peripheral distribution of the body heat.9 This causes a decrease in core body temperature. This decrease is sensed by the hypothalamic thermoreceptors which tries to increase the heat production primarily by shivering. Other intra operative causes of shivering may include disinhibited spinal reflex, respiratory alkalosis, decreased sympathetic activity or pain.10
Tramadol not only has a weak opioid activity it also inhibits the reuptake of serotonin and nor epinephrine at the spinal cord level. This inhibition increases the release of 5-hydroxytryptamine which influences the thermoregulatory center.
Our study showed a more than four time decrease in the incidence of shivering in the tramadol group as compared to NS group. This is consistent with the study of Subedi et al6 where the incidence of shivering in patients receiving tramadol [5%] was significantly lower than patients who received fentanyl [32%] intrathecally.
There was an increased incidence of shivering seen at 15 minutes after the block in both the groups. This increased incidence was associated with an increased heart rate. In a study conducted by Ghaffar et al11 to prevent post spinal shivering also showed that there was increased incidence of shivering at 15 minutes post spinal anaesthesia. There findings also concluded an adjacent increase in heart rate and mean arterial pressure.
This hemodynamic variation can be explained by the fact that shivering is associated with increased adrenergic and sympathetic hyperactivity.12 Moreover, there is an increased oxygen consumption and peripheral ischemia causing a further increase in the heart rate.13
The side effects were comparable in both the groups and were not statistically significant. Even though in a study conducted by prasad et al.14 there was increased incidence of nausea [ 58%] and vomiting [40%] in parturient who were given intrathecal tramadol. This decreased incidence in our study can be attributed to the standard aspiration prophylaxis which was given to every patient in our study.
The incidence of nausea and vomiting is known to occur in parturient at a higher rate.15 This is probably due to use of uretrogenic drugs, excessive handling of uterus, abdominal viscera and peritoneum. Tramadol, due to it’s ability to increase 5-HT levels, has the potential to potentiate the emetic effect in parturient.15 Hence, addition of aspiration prophylaxis can be helpful in these patients.
Pregnant females are also more prone to side effects of pruritis after intrathecal administration of opioids with incidence as high as 60%.16 pain and pruritus are transmitted by the same population of sensory neurons, namely small un-myelinated nerve fibers (C-fibers) and the release of prostaglandins (PGE1 and PGE2) enhance C-fiber transmission to the central nervous system, which potentiates pruritus17 A study conducted shah et al.16 concluded that when a local anaesthetic is added to opioid there is a significant reduction in the incidence of pruritis. Moreover, almost negligible incidence of pruritis can be attributed to a very low dose of tramadol used.
Conclusion
Based on our study we can conclude that intrathecal tramadol is effective in countering the anaesthesia induced shivering in parturient. The incidence of nausea and are not significant when a standard aspiration prophylaxis is given to patients. Also, it is not associated with side effects like pruritis and respiratory depression.
Conflict of Interest
There is no conflict of interest.
References
- Spielman FJ, Corke BC Advantages and disadvantages of regional anesthesia for cesarean section. A review. J Reprod Med. 1985 Nov;30(11):832-40
- Crossley AW. Peri-operative shivering. Anesthesia 1992;47:193-5.
CrossRef - Ozaki M, Kurz A, Sessler DI, Lenhardt R, Schroeder M, Moayeri A, et al. Thermoregulatory thresholds during spinal and epidural anesthesia. Anesthesiology 2004;81:282-8.
CrossRef - Buggy DJ, Crossley AWA. Thermoregulation, mild perioperative hypothermia, and post-anaesthetic shivering. Br J Anaesth. 2000;84: 615–628.
CrossRef - Bamigbade T, Langford R. The clinical use of tramadol hydrochloride. Pain Rev 1998;5:155-82.
CrossRef - Subedi A, Biswas BK, Tripathi M, Bhattarai BK, Pokharel K. Analgesic effects of intrathecal tramadol in patients undergoing caesarean section: A randomized, double-blind study. Int J Obstet Anesth 2013;22:316-21
CrossRef - Wrench IJ, Singh P, Dennis AR, Mahajan RP, Crossley AW. The minimum effective doses of pethidine and doxapram in the treatment of post‑anaesthetic shivering. Anaesthesia 1997;52:32‑6.
CrossRef - Visual analogue scales (VAS): Measuring instruments for the documentation of symptoms and therapy monitoring in cases of allergic rhinitis in everyday health care. Ludger Klimek, Karl-Christian Bergmann, […], and Oliver Pfaar.
- Hynson JM, Sessler DI, Glosten B, McGuire J. Thermal balance and tremor patterns during epidural anesthesia. Anesthesiology 1991;74:680-90.
CrossRef - Sessler DI. Temperature monitoring. In: Millar RD, editor. Textbook of Anaesthesia. 5th New York: Churchill Livingstone Inc; 1994. p. 1367-89
- Hala S. Abdel‐Ghaffar Seham M. Moeen Prophylactic granisetron for post‐spinal anesthesia shivering in cesarean section: A randomized controlled clinical study https://doi.org/10.1111/aas.13084
CrossRef - Physiologic responses to mild perianesthetic hypothermia in humans.Sessler DI1, Rubinstein EH, Moayeri A. DOI:1097/00000542-199110000-00009
- Lopez MB. Postanaesthetic shivering – from pathophysiology to prevention. Rom J Anaesth Intensive Care. 2018;25(1):73–81. doi:10.21454/rjaic.7518.251.xum
CrossRef - Prasad RB, Joel CJ, Zachariah VK. Effectiveness of addition of intrathecal tramadol with hyperbaric bupivacaine in prevention of shivering in parturients undergoing cesarean section under spinal anesthesia: A randomized Placebo-controlled study. Karnataka Anaesth J [serial online] 2015 [cited 2019 Aug 12];1:123-7
CrossRef - Lussos SA, Bader AM, Thornhill ML, Datta S. The antiemetic efficacy and safety of prophylactic metoclopramide for elective cesarean section delivery during spinal anesthesia. Reg Anesth 1992;17:126-30.
- Shah MK, Sia AT, Chong JL. The effect of the addition of ropivacaine or bupivacaine upon pruritus induced by intrathecal fentanyl in labour. 2000;55:1008–13.
CrossRef - Gulhas N, Erdil FA, Sagir O, Gedik E, Togal T, Begec Z, et al. Lornoxicam and ondansetron for the prevention of intrathecal fentanyl-induced pruritus. J Anesth. 2007;21:159–63.
CrossRef
(Visited 630 times, 1 visits today)







