Manuscript accepted on :08-04-2020
Published online on: 10-06-2020
Plagiarism Check: Yes
Reviewed by: Akshat Pandey
Second Review by: Cherry Bansal
Final Approval by: Dr Pallav Sengupta
Shivani Dixit , Sunil B.Vasudevarao*
, Sunil B.Vasudevarao* and Shaila Kamath
and Shaila Kamath
Department of Anaesthesiology, KMC Mangalore Manipal Academy of Higher Education, Mangalore, Karnataka, India -575001
Corresponding Author E-mail : drsunilbv@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/1937
Abstract
Venepuncture is a painful but necessary prerequisite for safe administration of anaesthesia. Various pharmacological and non pharmacological methods have been attempted to decrease venepuncture pain. EMLA (eutectic mixture of 2.5% lidocaine and 2.5% prilocaine) cream facilitates the local absorption of both constituent drugs without organic solvents, resulting in high concentrations of lidocaine/prilocaine in the skin. Valsalva maneuver reduces the severity of pain associated with venepuncture, via stimulation of the vagus nerve. We conducted an observational study to evaluate the efficacy of Valsalva maneuver and EMLA cream in decreasing venepuncture pain. After obtaining approval from the Indian Ethics Committee, 129 American society of anesthesiology Class 1 & 2 patients who were posted for various surgeries, aged 18-60 years were chosen after obtaining consent. They were randomly allocated into two groups using computerized tables (Group E – 65, Group V – 64), with application of EMLA cream (Group E) and valsalva maneuver (Group V) being performed prior to venepuncture. Post venepuncture, VAS, pain score (to assess subjective and objective pain) and changes in hemodynamic parameters were assessed. Data was analysed using student unpaired ‘t’ test, student paired t test and X2 test. Average Pain score and VAS score for Group E was 1, 0.94 and in Group V was 2 and 2.24 respectively (p <0.0001). Average change in HR and MAP was 3 bpm and MBP 1 mm Hg in Group E, and 6 bpm and MBP 3 mm Hg in Group V, comparing prior and post venepuncture parameters . Average increase in HR and MBP was seen to be significantly more in Group V than in Group E.(p <0.0001). Pain on venepuncture after EMLA cream application was significantly lesser than pain on venepuncture after valsalva maneuver.
Keywords
EMLA; Nociception; Pain; Valsalva; Visual Analogue Score
Download this article as:| Copy the following to cite this article: Dixit S, Vasudevarao S. B, Kamath S. A Comparison between Valsalva Maneuver and Eutectic Mixture of Local Anaesthetic to Relieve Venepuncture Pain. Biomed Pharmacol J 2020;13(2). |
| Copy the following to cite this URL: Dixit S, Vasudevarao S. B, Kamath S. A Comparison between Valsalva Maneuver and Eutectic Mixture of Local Anaesthetic to Relieve Venepuncture Pain. Biomed Pharmacol J 2020;13(2). Available from: https://bit.ly/2zof1Yi |
Introduction
Venous cannulation is considered a stressful and painful procedure. It is essential for safe practice of any type of anaesthesia. Physical, emotional and psychological factors play a major role in perception and the characteristics of pain [1]. Patients feel anxiety arising from the anticipation of pain due to injections. [2,3] Anxiety and irrational fear of needles affects an estimated 10% of the population. and it can result in delaying essential medical services and care . Various techniques have been tried to alleviate pain on venepuncture, both non-pharmacological and pharmacological. Non-pharmacological methods address the psychological aspect of pain. Distraction tactics such as diversion of attention, cough maneuver and acupuncture have been tried in the past [4-7]
Pharmacological measures include use of ethyl chloride, ice, and local anaesthetic preparations [8,9]. Several different local anaesthetic topical preparations have been used including Liposomal lidocaine preparation, Lidocaine/Prilocaine cream, tetracaine/lidocaine patch, and lignocaine iontophoresis [10-13]. In current medical practice, use of these techniques is relatively infrequent due to inconvenience, slow onset of activity, and side effects such as vasoconstriction.
EMLA is a eutectic mixture of two different local anaesthetics, namely 2.5% lidocaine and 2.5% prilocaine cream [14]. In combination, both drugs are absorbed better locally and hence organic solvents are not required. EMLA cream on absorption, leads to an increased concentration of lidocaine/prilocaine at the level of skin, making it an effective surface anaesthetic agent. EMLA has successfully been used as a local anaesthetic in the past for various procedures, such as vaccinations and placement of invasive lines .
Valsalva maneuver is known to reduce the extent of pain perceived while undergoing venepuncture. Performing valsalva maneuver causes an increase in the intrathoracic pressure. Baroreceptors are then activated, and the vagus nerve is stimulated [14,15]. Sensory fibres from various sites, mainly the upper GI tract, the oropharynx, thoracic and abdominal cavities relay information to the nucleus of tractus solitarius through vagal fibres, including fibres that relay nociception [16,17]. Hence, valsalva can cause an antinociceptive effect in humans.
Our study has compared EMLA cream and valsalva maneuver, in terms of pain response, and changes in hemodynamic parameters on performing venepuncture.
Methods
An observational study was conducted after obtaining approval from the Institutional Ethics committee (IEC KMC MLR 11-16/315) in a tertiary care centre from December 2016 to June 2018. 129 ASA Class 1 & 2 patients aged 18-60 years, posted for elective surgeries were divided into 2 groups named Group E and Group V. The sample size was calculated using the formula
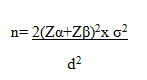
Where Zα = 1.96 (with 95% confidence interval)
Zβ = 1.28 (with 90% power)
σ= SD
d= Mean difference
Data was analysed using student paired ‘t’ test, student unpaired ‘t’ test, chi-square test, Fischer’s exact test. IBM SPSS Statistics version 17 software was used. The study protocol was explained and written informed consent was taken. Any history of allergies or sensitivity to local anaesthetics was obtained.
The primary outcome of the study was the pain felt during Venepuncture. Secondary outcome included the changes in the haemodynamic parameters measured before and 2 min after securing the cannula.
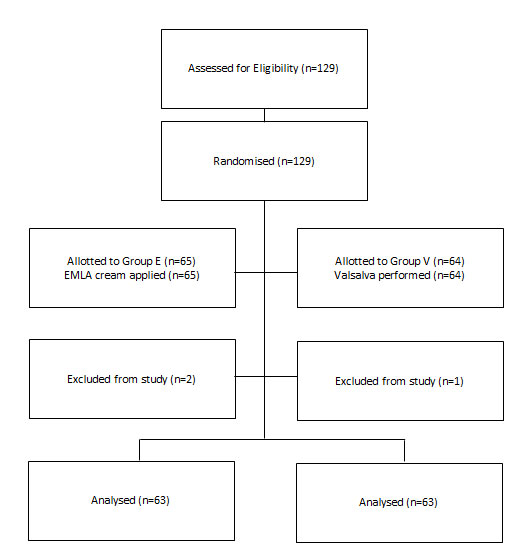
The patients were assigned into two groups after computerized randomization [Figure 1/Table 1]:
GROUP E
The patients receiving EMLA cream application 30 minutes prior to venepuncture
GROUP V
The patients performing Valsalva Maneuver prior to venepuncture.
In Group E, the dorsum of hand was covered with a thick layer of EMLA cream for 30 mins. before venous cannulation. In the operating room, once patients were in supine position, a vein on dorsum of the non-dominant hand was chosen and patients were told to turn their head to the opposite direction. Sterile spirit swab was used to clean the dorsum of the hand. A venous tourniquet was applied and peripheral venous cannulation was performed. If the selected vein was not prominent enough, it was tapped upon and time taken was noted. Venepuncture was performed by the anaesthetists using a 18G venous cannula.
In group V, the patients were educated on how to perform VM by the anesthetist. Patients were asked to blow into rubber tubing connected to a sphygmomanometer and raise the mercury column up to 30 mm Hg for a period of at least 20 seconds. In the operating room, patients were placed in the supine position. A vein on the dorsum of the non-dominant hand was identified. Venous tourniquet was applied and a sterile spirit swab was used to clean the dorsum of the hand. The patients were asked to perform valsalva maneuver, and hold their breath for a period of 20 seconds. If the proposed vein was still not prominent enough, it was tapped upon and the time taken was recorded. VP was then performed by anaesthetists using an 18G venous cannula.
During the process of venous cannulation, an independent anesthesiologist observed and questioned the patients.
Pain was Graded Using a 4-Point Scale
0 – No apparent pain,
1- Mild pain (reported only in response to questioning, and without any behavioral signs such as arm withdrawal, facial grimacing or tears),
2 – Moderate pain (reported in response to questioning, and accompanied by a behavioral sign or pain reported without questioning), and
3 – Severe pain, i.e., strong vocal response or response which was accompanied with behavioral signs
After venous cannulation, pain during the process was assessed on a Visual analogue scale of 0 –10 where 0 stands for “no pain” and 10 stands for “worst imaginable pain” by the same anesthetist.
Patients with failed cannulation in the first attempt were not included in the study. Hemodynamic parameters including heart rate and Mean blood pressure were recorded before and 2 mins after venous cannulation to detect sympathetic response to pain. Complications to procedure, such as allergic or skin reactions,or syncope, were recorded.
Consort Chart
Results
Age,(P;0.980/X2 .433) Sex,(P;0.719/X2 .130) and ASA Grading(P;0.471/X2 .519) were comparable in Group E and Group V(P>0.05) as seen in table 1 and 2.
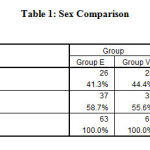 |
Table 1: Sex Comparison |
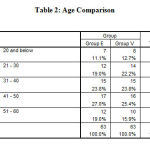 |
Table 2: Age Comparison |
The median pain score in patients in Group E [0.94±0.504] was 1, and in Group V [2.24±0.615] was 2. The difference in pain score between the two was found to be statistically significant (p=0.0001)as seen in table 3.
The median values of VAS score in Group E [1.83±0.583] was 4 for post venipuncture, whereas Group V [3.48±0.592] had a VAS score of 2. The difference in VAS score between the 2 groups was statistically significant (p=0.0001) as seen in table 3.
Table 3:
| Group | ||||||
| Group E | Group V | Chi square/Fishers exact test | ||||
| Count | Column N % | Count | Column N % | |||
| PAIN RESP | 0 | 10 | 15.9% | 0 | .0% | p=0.000, HS |
| 1 | 47 | 74.6% | 6 | 9.5% | ||
| 2 | 6 | 9.5% | 36 | 57.1% | ||
| 3 | 0 | .0% | 21 | 33.3% | ||
| Total | 63 | 100.0% | 63 | 100.0% | ||
| VAS | 1 | 17 | 27.0% | 0 | .0% | p=0.000, HS |
| 2 | 40 | 63.5% | 3 | 4.8% | ||
| 3 | 6 | 9.5% | 27 | 42.9% | ||
| 4 | 0 | .0% | 33 | 52.4% | ||
| Total | 63 | 100.0% | 63 | 100.0% | ||
Change in heart rate for group E was from 71.38±10.69 to 74.57±11.27.For group V, change in heart rate was from 76.35±10.48 to 88.06±9.07. Average increase in HR was significantly more in Group V when compared to Group E.(p <0.0001) .(figure 1)
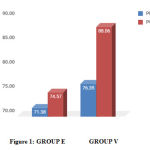 |
Figure 1: GROUP E GROUP V |
Changes in MBP for group E, was from 72.9±5.06 to 73.7±5.27 For Group V, Change in MBP was from 71.83±4.36 to 74.32±4.33. (figure 2). Average increase MBP was significantly more in Group V when compared to Group E.(p <0.0001) .
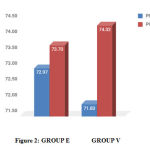 |
Figure 2: GROUP E GROUP V |
Side effects were significantly high in Group E. We noticed redness in 6 patients and pallor in 2 patients which is statistically significant (table 2) P <0.0001.(table 4)
Discussion
In this study, we have attempted to compare a simple technique, performing Valsalva maneuver, with EMLA cream application, and we found EMLA cream was significantly more efficacious in lowering pain on venepuncture when compared to Valsalva Maneuver.
Previous reports [15-17] have shown that the vagus stimulation results in antinociception, which decreases the intensity of pain perception by humans. The proposed mechanism is antinociception occurring due to central inhibition by vagus nerve, along with added contributions from noradrenergic, opioid and serotonergic pathways, rather than solely the primary afferents. Central relay stations, mainly the nucleus of tractus solitarius (NTS) and locus coereleus and subcoereleus have been identified. During Valsalva maneuver, the vagus nerve is stimulated via baroreceptors, which ultimately results in decreased pain perception [16,17].
Lal et all [18] performed studies in children comparing EMLA cream and distraction techniques, and found no difference in pain scores in the two groups. Hence, the Valsalva maneuver can also be a technique of distraction of attention from the actual skin prick. Although it has been postulated that syncope and dizziness may occur in patients due to valsalva, this problem was not encountered in our study.
Shivashankar et al [7] proved in their study on venepuncture in children, that among various non-pharmacological methods, distraction using a flash of light was more effective than valsalva maneuver in attenuating pain on cannulation.
EMLA cream is constituted from oil, water and eutectic mixture in equal parts of lignocaine and prilocaine (2.5%). The local anaesthetic molecules bind to free nerve endings in subcutaneous tissue, leading to local anaesthetic effect.
Fetzer [19] performed a metaanalysis which included 20 studies, and concluded EMLA cream is a highly effective agent to decrease venepuncture pain. However, it is considered expensive and often impractical in emergency settings as it requires about 30 minutes to act. Also, EMLA cream may have mild local side effects, such as contact dermatitis, urticaria and local pallor. In our study, pallor at the site of application was observed in 6 patients and redness of skin in 2 patients on applying EMLA, which then resolved within 24 hours without any treatment. Thakur et al [20] first reported the first case of allergic contact dermatitis after applying EMLA cream confirmed with patch test, proving prilocaine was the allergic ingredient.
Our study demonstrates the efficacy of two different techniques, namely the Valsalva maneuver and EMLA cream, in terms of analgesic strength prior to performing venepuncture.
In our study, the highest pain score and VAS score was seen in patients who had performed Valsalva maneuver, vis-a-vis EMLA cream, and the difference was found to be statistically significant. (p=0.00)
In contrast, in the study conducted by Suren M et al [4], a prospective double-blinded, randomized controlled trial comparing EMLA cream with valsalva maneuver in adult patients undergoing venepuncture concluded that valsalva maneuver is equally effective when compared to EMLA in decreasing pain on cannulation.
A randomized controlled study conducted by O Akdas et al [13] compared Valsalva Maneuver with application of EMLA cream in paediatric patients undergoing VP prior to elective surgeries. Their study showed that EMLA cream was far more efficacious than Valsalva maneuver in decreasing pain on cannulation, and changes in hemodynamic parameters were significantly more in the valsalva group in comparison to the EMLA group following puncture. Although valsalva is a cost effective and convenient method to decrease venepuncture pain, EMLA cream is far better for alleviating pain.
In our study, we found that EMLA cream was significantly more effective in lowering pain on venepuncture when compared to Valsalva Maneuver. However, it is a point to be noted that success of cannulation in the first attempt was significantly more in Group V when compared to E, most likely due to increase in the vessel diameter on performing Valsalva. In contrast, the use of EMLA cream made the site of cannulation slippery and caused venoconstriction, making cannulation difficult in some cases. We excluded 2 cases from the study from group E and 1 case from group V due to more then 2 attempts for securing the cannula. Valsalva is a cost effective and convenient method that can be performed in any hospital setting easily, although not as efficacious as EMLA cream in terms of pain reduction.
The limitation of our study is mainly the unblinded nature of the trial, as the two study groups had different application techniques and mechanisms of action. This has to be accepted as a bias. Also, several factors may influence the pain felt on puncture, such as experience of the anaesthetist performing cannulation and technique of performing the procedure. To avoid bias, a study has to be conducted in much larger numbers to conclusively prove superiority of EMLA over valsalva.
Conclusion
Based on the results, we conclude that the EMLA cream is a superior analgesic modality when compared to Valsalva maneuver, prior to performing venepuncture.
Acknowledgement
I thank my institute and anaesthesia department for their support
Conflict of Interest
There is no conflict of interest.
Financial Funding
There is not funding source for this work
References
- Speirs A F, Taylor K H, Joanes D N, Girdler N M. A comparative study of topical skin analgesics and the anxiety and discomfort associated with venous cannulation. Br Dent J 2001; 190:444-9
- Agarwal A, Sinha P K, Tandon M, Dhiraaj S. Evaluating the efficacy of valsalva maneuver on venous cannulation.Anaesth Analgesia 2005; 101:1230-2.
- Boerner K E, Kathryn A. Birnie .Simple Psychological Interventions for Reducing Pain From Common Needle Procedures in Adults.Clin J Pain. 2015 Oct; 31(Suppl 10): S90–S98.
- Suren M , Kaya Z , Ozkan F, Erkorkmaz U, Arici S, et al. Comparison of use of Valsalva maneuver and EMLA cream to relieve venipuncture pain. Japanese society of anaesthesiologists,2012.
- Usichenko T I,Pavlovic D, Foellner S, Wendt M. Reducing venipuncture pain by a cough trick. Anaesthesia analgesia 2005;98:343-45.
- Basaranoglu G, Erden V, Delatiglu H, Pekel A F. The effect of Valsalva maneuver on venepuncture pain.Eur J Anaesthesiology 2006;23:591-3.
- Shivashankar A, Nalini K B. The role of nonpharmacological methods in attenuation of pain due to peripheral venous cannulation : A randomised controlled study. Anesth Essay Res.2018 Jan-Mar; 12(1): 7-10.
- .Zempski W T, Lijewski B, Kauffman R E, Malviya S V. Needle free powder lidocaine delivery provides rapid analgesia for venipuncture or cannulation pain in children.J Paediatrics.2008;121-979-87.
- Taddio A, Sion H K . Liposomal lidocaine to improve procedural success rates and reduce procedural pain among children- a randomised controlled trial.CMAJ 2005;172(13): 1691–1695.
- Jiminez N, Bradford H, Sousa M. A comparison of needle free injection for local anaesthesia versus EMLA for intravenous catheter insertion in paediatric patients.Anaesthesia analgesia 2006;102;411-4
- Yamamoto L G, Boychuk R B. Randomised controlled trial of 20 minute EMLA cream to reduce pain of peripheral iv cannulation.Am J Emergency Medicine 1998;16:634-46
- Kim W O, .Song B M. Efficacy and safety of a lidocaine/tetracaine medicated patch or peel for dermatologic procedures: a meta-analysis.Korean J Anesthesiol. 2012 May; 62(5): 435–440.
- Akdas O, Ozdemir H, Comlekci M. Effect of valsalva maneuver on venipuncture pain in children: Comparison to EMLA. Royal academy of Medicine,Ireland,2013.
- Taddio A, Ohlsson A.A Systematic Review of Lidocaine-Prilocaine Cream (EMLA) in the Treatment of Acute Pain in Neonates. AA Pediatrics February 1998, Vol 101;2.
- Henry TR. Therapeutic mechanisms of vagal nerve stimulation.J Neurology.2002;24:3-4
- .Liporace J, Hucko D, Morrow R, Sperling M. Vagal nerve stimulation: adjustments to reduce painful side effects. Neurology 2001;57:885-6.
- Frangos E ,Emily A . Richards Bushnell M C.. Do the psychological effects of vagus nerve stimulation partially mediate vagal pain modulation.Neurobiology of Pain 2017;1: 37-45.
- Lal M K, McClelland J, Phillips J, Taub N A, Beattie R M. Comparison of EMLA cream versus placebo in children receiving distraction therapy for venepuncture.Acta Paediatr. 2001 Feb;90(2):154-9.
- Fetzer S J. Reducing venipuncture and intravenous insertion pain with eutectic mixture of local anesthetic: a meta-analysis. Nurs Res. 2002 Mar-Apr;51(2):119-24.
- Thakur BK, Murali MR. EMLA cream induced allergic contact dermatitis ; a role for prilocaine as an immunogen. J Allergy and Immunol.1995;95:776-8







