Manuscript accepted on :30-10-2019
Published online on: 22-11-2019
Plagiarism Check: Yes
Reviewed by: Aravinth Subramanium
Second Review by: Hazem Shaheen
Final Approval by: Ayush Dogra
Senthurselvi Ramamoorthy* and Bhuvaneswari K
and Bhuvaneswari K
Department of Pharmacology, PSG institute of Medical Sciences and Research, The Tamilnadu Dr.MGR Medical University, Coimbatore, India, 641004
Corresponding Author E-mail: senthur_selvi@yahoo.co.in
DOI : https://dx.doi.org/10.13005/bpj/1829
Abstract
Polycystic Ovarian Syndrome (PCOS) is a common disease exclusively seen in women of reproductive age group. World Health Organization reports that Polycystic Ovarian Syndrome approximately affects 5-10% of the reproductive female population worldwide. Women with PCOS have chronic inflammation. This in turn leads to increased incidence of non-communicable diseases like cardiovascular disease and diabetes2. Chronic inflammation in PCOS patients can be identified using serum markers such as C - reactive protein [CRP], Interleukin-6 [IL-6] and Interleukin-18 [IL-18].So the main objective of the study was to assess the status of inflammation in patients with Polycystic Ovary Syndrome (PCOS) and to assess the influence of drugs prescribed for PCOS on inflammation. Patients were divided into three groups as healthy volunteers, newly diagnosed PCOS patients, already on treatment patients for PCOS. High sensitivity CRP (hs-CRP), IL-6 and IL-18 were assessed. There was an increase in the hs-CRP, IL-6 and IL-18 compared to healthy volunteers in both newly diagnosed and already diagnosed groups. But there was no statistical significance (hs-CRP=0.975, IL-6=0.746, IL-18 = 0.148) between them. The mean value has decreased in the already on treatment group as duration of treatment increases. There was no statistical significance between them. There was an inversely proportional relationship between the mean values of inflammatory markers and duration of treatment.
Keywords
Polycystic ovarian syndrome; Insulin Resistance; Inflammation; inflammatory markers; hs-CRP; IL-6; IL-18
Download this article as:| Copy the following to cite this article: Ramamoorthy S, Bhuvaneswari K. A Cross Sectional Study on the Status of Inflammatory Markers in Polycystic Ovary Syndrome (Pcos) in Indian Population. Biomed Pharmacol J 2019;12(4). |
| Copy the following to cite this URL: Ramamoorthy S, Bhuvaneswari K. A Cross Sectional Study on the Status of Inflammatory Markers in Polycystic Ovary Syndrome (Pcos) in Indian Population. Biomed Pharmacol J 2019;12(4). Available from: https://bit.ly/2OaJUE4 |
Introduction
Polycystic Ovarian Syndrome (PCOS) is a common disease exclusively seen in women of reproductive age group.World Health Organization reports that Polycystic Ovarian Syndrome approximately affects 5-10% of the reproductive female population worldwide. A study by Ridhi R et al. shows it affects the Indian female adolescents approximately by 9.13%1.
Women with PCOS have chronic inflammation. This in turn leads to increased incidence of non-communicable diseases like cardiovascular disease and diabetes2. Chronic inflammation in PCOS patients can be identified using serum markers such as C – reactive protein [CRP], Interleukin-6 [IL-6] and Interleukin-18 [IL-18].
Insulin resistance [IR] and its associated hyperinsulinemia leads to a sequence of events collectively called as insulin resistant syndrome. The sequence of events includes cardiovascular disease, hypertension, polycystic ovary syndrome and non-alcoholic steato hepatitis3. Insulin resistant syndrome and diabetes are inter-related but are different entities. All insulin resistant individuals need not be diabetic, but develops diabetes only if he is not able to make up the degree of hyperinsulinemia needed to overcome the insulin resistance. Even though an insulin resistant individual need not be diabetic the risk of developing the consequences of insulin resistance syndrome are high. Patients with insulin resistance syndrome have increased concentrations of plasminogen activator inhibitor-1, C-reactive protein and increased white cell count. Hence these patients are at increased risk of developing PCOS.
Low grade inflammation which is of chronic is related to obesity, IR syndromes such as polycystic ovary syndrome, and an increased risk of cardiovascular disease4. In obese patients enlargement of adipose tissue causes adipocyte hypertrophy and hyperplasia and this huge adipocytes outshine the local supply of oxygen causing the cell hypoxia independently with stimulation of cellular stress pathway5. This leads to independent inflammation of the cells and cytokines and other pro-inflammatory signals to get released. As a fragment of this chronic inflammatory process, locally released chemokine draws pro-inflammatory macrophages into the adipose tissue. These then produce structures similar to crown round the huge lifeless or dying adipocytes. These tissue macrophages release cytokines which then trigger the inflammatory process in adjacent adipocytes, aggravating inflammation and insulin resistance.
There is also genetic basis for the inflammation observed in PCOS6.Variants in the gene encoding TNFα7, type 2 TNF receptor and IL-68-10 and its signal transducer11 have been reported in association with PCOS in European population. These findings are in conceptual agreement with a common evolutionary background for PCOS and metabolic disorders.Interleukin-6 is an endocrine cytokine produced by mononuclear cell and adipose tissue that is directly responsible for stimulating hepatic CRP synthesis12-15. CRP in turn has emerged as a major predictor of metabolic dysfunction in asymptomatic individuals, and is also produced by adipose tissue16, 17. Hence C-reactiveprotein is the most consistent circulating marker of low- grade chronic inflammation in PCOS. Like C-reactive protein and IL-6, IL-18 is also a proinflammatory cytokine which promotes secretion of TNF-α18, which further stimulates the production of IL-6.
So this study was basically carried out to see if there is any association between inflammation and PCOS. If the serum inflammatory markers are higher then there is an association between inflammation and PCOS in Indian Population.
In addition to it we would also like to see drugs used in PCOS have any influence over the inflammation in PCOS.Numerous therapies have been projected for the treatment modalities of polycystic ovarian syndrome, but the ideal treatment for infertile women with polycystic ovarian syndrome has not yet been clear. Drug treatment comprises clomiphene citrate, insulin sensitizing agents, gonadotropins and gonadotropin- releasing hormone (GnRH) analogs. Surgical treatments include laparoscopic ovarian drilling and the application of assisted reproduction techniques. Besides this loss of weight, diet and physical exercise have been shown to develop hyper insulinemia, menstruation abnormalities and ovulatory rates. Even though these many drugs and modalities of treatment were available for PCOS, only few drugs targeted in reduction of inflammation.Studies showed that there was a decrease in interleukin-6 and interleukin-18 level after metformin treatment for three months in polycystic ovary syndrome patients. This shows metformin decreases the inflammatory markers and have beneficial effect on inflammatory process of PCOS19. Many earlier studies spoke about metformin and their anti-inflammatory properties. There were no studies demonstrating the anti-inflammatory effect of other drugs used to treat PCOS in practise. So we thought to see any other drugs used to influence the inflammation.
Materials and Methods
This study was a prospective cross sectional study. The study population was from all the patients who attended the outpatient Department of Obstetrics and Gynecology in PSGIMSR Hospital, Coimbatore. We included all the PCOS patients according to Rotterdam consensus criteria with age group 18-45 years and excluded those patients presenting with a history of inflammatory diseases or intake of inflammatory drugs and also pregnant women. Healthy Volunteers of age group 18- 45 years women with normal reproductive cycle were included and those who present with history of inflammatory drugs or diseases are excluded. Further those who have hypertension or diabetes are also excluded from the healthy volunteers.
The overview of the study design is given in the figure below. The patients were divided into three groups.
Group 1: Healthy volunteers
Group 2: Newly diagnosed PCOS
Group 3: Already on treatment for PCOS
Sample size estimated according to previous literature search.30 participants in each group was taken. The study design was submitted to the Institute Human Ethics Committee (IHEC) stating its purpose preceding the study. After its approval the study was initiated. The details and the usefulness of the study design were described to every participant individually and clarified their doubts before getting the informed consent forms. The informed consent forms provided to the participants were either in English or in Tamil. The participants, who gave written informed consent, came under the inclusion criteria were enrolled for the study. Healthy volunteers were also given the informed consent. The patients who declined to give informed consent were also excluded from the study.
PCOS patients were selected according to Rotterdam Consensus Criteria 2003 which is given below.
Polycystic ovaries(12 or more follicles in each ovary, each follicle measuring 2-9 mm in diameter and/or ovarian volume > 10 ml, one polycystic ovary is sufficient for diagnosis)
Oligo-/anovulation; clinical diagnosed as Oligo-/amenorrhea (menstrual cycles longer than 35 days or less than 10 menstruation/year)
Hyperandrogenism (clinical or biochemical)
Basic demographic data like name, age and measurements like Height, weight, body mass index were recorded. History of the patient and if the patient is on already treated group then their treatment history were noted.
Our study was to observe if there were abnormalities in High sensitivity C – reactive protein, Interleukin-6 and Interleukin-18 in PCOS patients and to compare those with the healthy volunteers.
The high sensitivity CRP was tested in the Clinical Biochemistry lab using the Cobas Integra C – reactive protein (Latex). This machine works by the methodology of “Particle enhanced turbidimetric assay”.
The Interleukin-6 and Interleukin-18 were estimated in the Pharmacology laboratory using Krishgen Biosystems, imported from California, USA and read by an Elisa reader which is a Bio-rad system at an absorbance of 405 and 450 nM.
Statistical analysis was performed by using SPSS software version 19. The results were analyzed using one way ANOVA and post hoc analysis was done using LSD.
Results and Discussion
Our study was intended to evaluate the status of inflammation, by measuring hs-CRP, IL-6 and IL-18, in PCOS patients in Indian population. It was also aimed to assess the influence of drugs prescribed in PCOS patients on the inflammation.
Polycystic Ovary Syndrome is an endocrine disorder which is very common in the female population in the reproductive age group20. Most women shows the features of metabolic syndrome. It is also concomitant with hypertension, diabetes, dyslipidaemia, gestational type 2 diabetes21.
PCOS is associated with obesity and also increased incidence of insulin resistance22. There is also increased risk of cardiovascular complications. The inflammation which is of chronic low grade is related to PCOS. The C-reactive protein levels are an acute phase reactant and is circulating marker of cardiovascular events. CRP > 3mg/L in a patient is equal for metabolic syndrome as in ATP III guidelines. IL-6, TNF-α, IL-18 concentrations in serum is the predictors of cardiovascular events1. So, in this study we proposed to measure the IL-6, IL-18 and hs-CRP levels in PCOS patients in Indian population. There are various studies showing the significance of IL-6, IL-18 and hs-CRP in PCOS in other countries. There are no studies showing this significance in Indian Population.
There were many therapies of polycystic ovarian syndrome including drugs as well as surgical therapies and life style modifications. In previous studies drugs like metformin and thioazolidinones like pioglitazone, rosiglitazone decreases insulin resistance and also known to decrease the inflammation. Other drugs like myoinositol, clomiphene citrate improves ovulation alone. Their role in inflammation was not known in PCOS.
Ninety participants were recruited in our study. These participants were divided into three groups as normal controls, newly diagnosed patients and already diagnosed on treatment patients. Low grade chronic inflammation is associated with Polycystic Ovary Syndrome and it can be assessed using inflammatory markers like IL-6, IL-18 and hs-CRP. These are strong predictors of cardiovascular complications. Kelly et al. reported a study exhibiting an increase in CRP which shows a low grade chronic inflammation in PCOS patients. In this study they showed a mean value of PCOS patients was greater than normal controls2.
In our study there was no significant increase in the CRP levels (p=0.975).There was no significant difference between the newly diagnosed and already diagnosed patients suggesting that hs-CRP didn’t rise significantly in already diagnosed group as they were on treatment (Table 2&3).
In the same way there was also no significant changes in the IL-6 levels (p=0.746). There was an increase in their mean values when compared to normal controls. Mean value for normal controls was 34.35+93.88 whereas for newly diagnosed patients it was 90.58+308.62 and for already diagnosed it was 91.41+476.6 suggesting there was a rise in IL-6 levels in PCOS when compared to normal controls but that was not significant. Between newly diagnosed patients and already diagnosed patients there was no much difference between the levels (Table 2&3).
Another study by Hector et al showed there was an increase in IL-18 independent of obesity23. In our study the results showed there was an increase in the mean values of IL-18 in PCOS patients when compared to normal controls. The mean value for Normal control was 131.4+224.17 whereas for newly diagnosed and already diagnosed group of patients it was 264.86+316.33 and 282.2+403.92 respectively. The difference was not statistically significant (p=0.148) (Table 2 &3). There were also, as in IL-6, no difference in newly diagnosed and already diagnosed patients.
When we considered the treatment prescribed to the patients in already diagnosed group, most of the patients were in Metformin combination. Nearly 70% of patients were in metformin combination. Metformin was given along with myoinositol, clomiphene citrate, Human Chorionic Gonadotropins (HCG). Only 46.67% patients were on monotherapy of metformin (Table 1). The other common drug prescribed was myoinositol combination. It was also given along with metformin, clomiphene citrate and HCG. Metformin along with myoinositol was given to 13.3% of patients.
86.67% of patients were on these treatments for less than 1 year and only 13.33% of patients were on these therapies for more than 1 year (Figure 1).
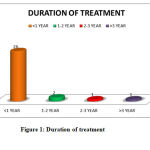 |
Figure 1: Duration of treatment |
Mekkawi et al stated that there was a statistical significant change in the Interleukin-6 and Interleukin-18 levels before and after metformin therapy showing metformin decreases the inflammatory markers in PCOS patients19. In previous studies it was known that there was an increase in the nuclear factor κ B (NFκB) in PCOS. Metformin inhibits NFκB which inhibits IL-1β and inhibits the production of pro inflammatory gene24.
In our study, the mean + SD for hs-CRP, IL-6,IL-18 were decreased between the patients as there was an increase in the duration of treatment (Figure 2,3,4).
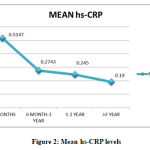 |
Figure 2: Mean hs-CRP levels
|
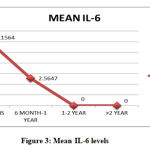 |
Figure 3: Mean IL-6 levels
|
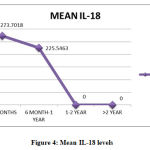 |
Figure 4: Mean IL-18 levels
|
Our results were consistent with Mohlig et al. who showed there was no substantial decrease in CRP and IL-6 levels. In their study these levels were increased in both normal and PCOS obese patients compared to the lean patients. There was a positive relationship between the obesity, insulin resistance and inflammatory markers than the PCOS itself. When a linear regression was done in their study it showed obesity was the one which increases the inflammatory marker than the insulin resistance9. Another study by Escobar-Morreale et al. also showed obesity causes an increase in the inflammatory marker and not the disease itself25.
Our study had only 13.3% of obese study population in the already diagnosed and on treatment group and 3.33% in the newly diagnosed PCOS group (Figure 5).
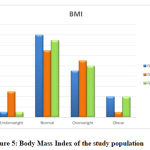 |
Figure 5: Body Mass Index of the study population
|
Also in our study there were about 86.7% of already diagnosed group of patients’ on treatment for less than one year (Figure 2). So even though there was a fall in the mean values of inflammatory markers there was no statistical significance in them.
The lack of statistical significance which may be due to small sample size in each group and wide range of values between the patients. The duration of treatment which was less than one year in most of the patients and hence the effect of drugs on the inflammatory markers could not be assessed. As this was a cross sectional study and blood samples were taken at one time the difference in the inflammatory markers could not be studied for the same group of patients. The influence of drugs prescribed was also in combination for most of the patients and so they could not be studied individually.
Summary and Conclusions
Though there are various pharmacological drugs available to treat PCOS, only few drugs targeted in reduction of inflammation. There were various studies, as we quoted earlier, demonstrating the effect of inflammation on PCOS. These studies were all done in other parts of the world. There were very less number of studies done in India. So we proposed to study the status of inflammation on PCOS in Indian population in particular South Indian population.
The pro inflammatory cytokines were produced when NFκB was stimulated. Metformin inhibits this NFκB and thus reduces the inflammation. Other drugs used in PCOS in practise like myoinositol, clomiphene citrate, hormones target at the disease per se and not on the inflammation produced by the disease.
Our study has shown that mean values of inflammatory markers were increased in Polycystic Ovary Syndrome (PCOS) in newly diagnosed and already on treatment for PCOS. 86.7% of the patients who were on already treatment for PCOS group were on treatment for less than one year. It has shown that there was an inversely proportional relationship between the mean values of inflammatory markers and duration of treatment.
We suggest larger follow up studies with longer duration of treatment so that influence of drugs on the inflammatory markers can be studied exhaustively in Indian population. Further studies are needed to demonstrate the effects of drugs for PCOS targeting on the inflammatory pathway so that these drugs not only brings down the severity of PCOS but also reduces the
cardiovascular risk factors associated with it.
Table 1: Represents the combinations of drug.
| Drugs | Percentage |
| Only Metformin | 46.67 |
| Metformin + Myoinositol | 13.33 |
| Myoinositol + Clomiphene citrate | 10 |
| Metformin+ Clomiphene citrate | 6.67 |
| Myoinositol + HCG + Clomiphene citrate | 6.67 |
| Myoinositol + Metformin + Clomiphene citrate | 6.67 |
| Myoinositol + HCG | 3.33 |
| Metformin + HCG | 3.33 |
| Myoinositol + HCG + LOD | 3.33 |
Table 2 and 3 represents the comparison of hs-CRP, IL-6 and IL-18 for the three groups.
Table 2: One way ANOVA
| hs-CRP | IL-6 | IL-18 | ||||
|
Between groups Within groups |
F | p-value | F | p-value | F | p-value |
|
0.025 |
0.975 |
0.293 |
0.746 |
1.954 |
0.148 |
|
Table 3: Post Hoc (LSD) analysis
| hs-CRP | IL-6 | IL-18 | ||||
| Between Groups Comparison | Mean Difference | P-value | Mean Difference | P-value | Mean Difference | P-value |
| I and II | 0.00667 | 0.963 | 56.23703 | 0.746 | 133.417 | 0.114 |
| I and III | 0.02433 | 0.867 | 57.06563 | 0.506 | 150.75323 | 0.074 |
| II and III | 0.03100 | 0.831 | 0.82860 | 0.992 | 17.33650 | 0.836 |
Acknowledgement
I am grateful to Dr. Seetha Panicker (HOD, Obstetrics & Gynecology) and Dr. G.Jayachandran (HOD, Biochemistry) of PSG Medical College and Research Institute for the necessary permissions granted and for the excellent amenities offered to carry out my study. My thanks to Professors Dr.Reena Abraham and Dr.Kanchanamalai, Obstetrics &Gynecology Department of PSG Medical college and Research Institute for giving me patients for my work. I am indebted to all the patients of my study for their kind participation and to the faculty and staff of Obstetrics and Gynecology department and to all the technical staff of Clinical Biochemistry and Pharmacology Laboratory for having spared their time and effort towards my thesis work.
Conflict of Interests
There is no conflict of interests.
References
- Nidhi R,Padmalatha V, Nagarathna R,Amritanshu Prevalence of polycystic ovarian syndrome in Indian adolescents. Journal of pediatric and adolescent gynecology. 2011; 24(4):223-7.
- Chris C.J.Kelly, Helen Lyall, John R.Petrie et al. Low grade chronic Inflammation in Women with Polycystic Ovarian Syndrome. The Journal of Clinical Endocrinology & Metabolism.2001,2453-2455.
- ACE position statement on the Insulin Resistance Syndrome, EnocrPract. May/June 2003; Vol 9 (No 3).
- Laure Morin-Papunen, Katrina Rautio, AimoRuokonen et al. Metformin Reduces Serum C-Reactive Protein Levels in Women with Polycystic Ovary Syndrome. J ClinEndocrinol Metab,2003; 88(10):4649-4654.
- Carl de Luca, Jerrold M. Olefsky. Inflammation and insulin resistance. FEBS [Federation of European Biohemical Societies] Letters 582(2008) 97-105.
- Escobar-Morreale HF, Batella. Carretero JI, Alvarez- Blasco F et al. The Polycystic Ovary syndrome associated with morbid obesity may resolve after weight loss induced by bariatric surgery. J ClinEndocrinolMetab. 2005; 90:6364-6369.
- Escobar-Morreale HF, Calvo RM, Sancho J et al. TNF-alpha and hyperandrogenism: a clinical, biochemical and molecular genetic study. J ClinEndocrinolMetab. 2001; 86:3761-3767.
- Villuendas G, San Millan JL, Sancho J et al. The -597 G>A and -174 G>C polymorphism in the promoter of the IL-6 gene are associated with hyperandrogenism. J ClinEndocrinolMetab. 2002; 87:1134-1141.
- Mohling M, Spranger J, Osterhoff M et al. The polycystic ovary syndrome per se is not associated with increased chronic inflammation. Eur J Endocrinol. 2004; 150:525-532.
- Erdogan M, Karadeniz M, Berdeli A, et al. The relationship of interleukin-6- 174 G>C gene polymorphism with oxidative stress markers in Turkish polycystic ovary syndrome patients.JEndocrinol Invest. 2008; 31:624-629.
- Escobar-Morreale HF, Calvo RM, Villuendas G, et al. Association of the polymorphism in the interleukin-6 receptor complex with obesity and hyperandrogenism. Obes Res. 2003; 11:987-996.
- Jones TH. Interleukin-6 an endocrine cytokine. ClinEndocrinol (Oxf). 1994; 40:703-713.
- Fried SK, Bunkin DA, Greenberg AS. Omental and subcutaneous adipose tissue of obese subjects release interleukin-6:depot difference and regulation of glucocorticoid. J ClinEndocrinolMetab. 1998;83:847-850.
- Purohit A, Ghilehik MW, Duncan L, et al. Aromatase activity and interleukin-6 production by normal and malignant breast tissues. J ClinEndocrinolMetab 1995; 80: 3052-3058.
- Moshage HJ, Roelofs HM, van Pelt JF, et al. The effect of interleukin-1, interleukin-6 and its interrelationship on the synthesis of serum amyloid A and C-reactive protein in primary cultures of adult human hepatocytes. BiochemBiophys Res Commun 1988; 155:112-117.
- Ridker PM, Hennekens CH, Buring JE, et al. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med. 2000; 342:836-843.
- Ouchi N, Kihara S, Funahashi T et al. Reciprocal association of C-reactive protein with adiponectin in blood stream and adipose tissue. Circulation.2003; 107:671-674.
- Okamura H, Tsutsui H, Kashiwamura S et al. Interkeukin-18: a novel cytokine that augments both innate and acquired immunity. AdvImmunol 70:281-312.
- ELMekkawi S.F., ELHosseiny A.S. Effect of Metformin Therapy on Serum Interleukin-6 and Interleukin-18 Levels in Patients with Polycystic Ovary Syndrome. Nature and Science. 2010; 8(9):23-26.
- Knochenhauer ES, Key TJ, Kahsar-Miller M, et al. Prevalence of the polycystic ovary syndrome in unselected Black and White Women of the Southeastern United States: A prospective study. J ClinEndocrinolMetab 1998;83:3078-3082.
- Wild S, Pierpoint T, et al. Long term consequences of polycystic ovary syndrome: results of a 31 year follow-up study. Human Fertility. 2000; 3(2): 101-105.
- Barber T.M., McCarthy M.I., et al. Obesity and plycystic ovary syndrome. Clinical Endocrinology. 2006; 65(2): 137-145.
- Hector F., Escobar-Morreale, et al. Serum Interleukin-18 Concentrations are increased in the polycystic ovary syndrome: Relationship to insulin resistance and to obesity. The Journal of Clinical Endocrinology & metabolism. 2004; 89: 806-811.
- Isoda K, Young JL,et al. Metformin inhibits proinflammatory responses and nuclear factor-κ B in human vascular wall cells. Arterioscler. Thromb. vasc. Biol. 2006; 26:611-617.
- Escobar-Morreale H.F., Villuendas G, et al. Obesity, and not insulin resistance, is the major determinant of serum inflammatorycardiovascular risk marker in premenopausal women. Diabetologia. 2003; 46: 625-633.







