Manuscript accepted on :20-July-2019
Published online on: 23-07-2019
Plagiarism Check: Yes
Reviewed by: Giovanni Damiani
Second Review by: Nicolas Padilla
Final Approval by: Dr. Ian James Martin
1Saveetha Medical College and Hospital, SIMATS, Chennai, 602105, India.
2Department of Pharmacology, Saveetha Medical College and Hospital, SIMATS, Chennai, 602105, India.
Corresponding Author E-mail: sheelapharm15@yahoo.in
DOI : https://dx.doi.org/10.13005/bpj/1752
Abstract
Neonatal hyperbilirubinemia, normally seen in 60% of term babies and 80% of preterm babies during the first week of life. Physiological jaundice appears between 30-72 hours after birth and eventually disappears on 10th day of life. Various reasons and risk factors are associated with jaundice. Eventhough, hyperbilirubinemia is not life threatening condition, the lack of timely treatment to newborns may lead to increased complications and death. The study was carried to identify the incidence, various aetiologies and treatment to hyperbilirubemic neonates. After obtaining, prior approval from ethical committee the study was initiated. The details of neonates admitted in neonatal wards during the year of 2017-2018 were collected from the Medical record department in a tertiary care hospital. The total number of live births in 2017-2018 was 1748 and 74 neonates were identified and treated for hyperbilirubinemia. The present study showed the incidence to be more in female babies than male babies. The female babies were about 55% and male babies were 44% . The preterm babies were 21% and term babies were 78%. The mode of delivery through LSCS was 56% and normal vaginal delivery was 43%. Hyperbilirubinemia seen in Multiparous was around 64% and in primiparous was around 35% . Majority of the newborns were in normal weights and physiological jaundice was the most common type of jaundice seen in newborns. Though, the recent techniques like Hour –Specific nanograms are available, the study indicates the necessity in educating mothers before delivery itself and introducing preventive steps, like pre-discharge assessment to reduce readmission and severity in newborns. The study finds a definite scope for further research and a need for easy techniques to early detection and treatment for the babies.
Keywords
Hyperbilirubinemia; Hour-Specific Nanogram; Physiological Jaundice; Preterm
Download this article as:| Copy the following to cite this article: Rithanya S, Sheela D. A Treatment Profile of Neonatal Hyper-Bilirubinemia in a Tertiary Health Care Hospital. Biomed Pharmacol J 2019;12(3). |
| Copy the following to cite this URL: Rithanya S, Sheela D. A Treatment Profile of Neonatal Hyper-Bilirubinemia in a Tertiary Health Care Hospital. Biomed Pharmacol J 2019;12(3). Available from: https://bit.ly/32NmSIz |
Introduction
Neonatal hyperbilirubinemia, the most common health problem in newborns and requires an essential medical attention. Normally, jaundice occurs in 60% of the term babies and 80% of the preterm babies within the first week of life [1,2]. Neonatal jaundice is prone to appear when the serum bilirubin level exceeds 5 mg/DL. In term babies, physiological jaundice appears between 30-72 hours of age and proceeds to a maximum intensity on fourth day which eventually disappears by 10thday of life [3]. The serum bilirubin level in above case does not exceed 15 mg/DL. Physiological jaundice in preterm babies is similar to term babies with maximum intensity reaching on 5-6 day and may persist up to 14 days. The serum bilirubin level in these babies may exceed 15 mg/DL. At normal concentration, bilirubin acts as an antioxidant, whereas when the concentration is increased they become as severe neurotoxin and responsible to produce acute or chronic bilirubin encephalopathy which leads to irreversible brain damage [4]. A study carried in Australia exhibited the incidence level of neonatal jaundice between 7.1 and 45 per 10,000 birth and kernicterus of 0.4-2.7 [5]. The other study conducted among Indian workers identified the overall incidence rate to be 54% to 77%. The various reasons and risk factors associated for the hyperbilirubinemia in neonates are ABO and other blood group incompatibility,glucose-6-phosphate dehydrogenase deficiency, infections, prematurity, low birth weight, lactation failure in excessive breastfeeding, cephalohematoma or bruises, babies of diabetic mother, hypothyroidisim, rare conditions such as Gilbert’s syndrome, Crigler-Najjar syndrome and family history of neonatal jaundice in siblings[6]. A worldwide study conducted in low- income population identified around 14 million newborns with jaundice and required phototherapy [7]. The bilirubin level in the skin was measured with the help of hand-held device, transcutaneous bilirubinometer. In absence of this instrument, jaundice can be assessed visually. The relationship between serum bilirubin levels and the progression of skin discoloration can be described using kramer’s rule. According to this rule, appearance of yellow colour in head and neck region indicates total serum bilirubin levels to be 4-8 mg /DL, in upper trunk (above umbilicus), to be 5-12 mg/DL, in lower trunk and thighs (below umbilicus), to be 8-16 mg/DL, in arms and lower legs to be 11-18 mg/DL and in palms and soles to be > 18mg/dl.
Many developmental changes were introduced in the management of neonatal jaundice. Hour–Specific monogram for predicting neonatal hyperbilirubinemia was imported by Bhutani et al which was also supported by American Academy of Paediatrics. Hence the present study was carried to evaluate the occurrence, various aetiologies and treatment profile for neonatal jaundice in a tertiary care hospital[8].
Materials and Method
The present retrospective study was carried in a tertiary care teaching hospital for 2017-2018. All the live births in the hospital during the study period were taken from Medical record department. Neonates admitted in neonatal ward with a visible jaundice during the study period were included. The most common treatment for non-severe hyperbilirubinemia was phototherapy and sunbath. The data collected for the study includes gestational age, gender, birth weight, birth order, mode of delivery, peak serum bilirubin level and the treatment profile. Aetiologies identified by thorough examinations in neonates were noted. An automated analyzer with calorimetric method was used to measure the serum bilirubin levels in the blood sample (venous) collected from the neonates. The clinical picture of neonatal jaundice was confirmed by carrying required test. The severity was categorized depending on bilirubin levels and it was grouped above 18 mg/DL in preterm babies and above 20 mg/DL in term babies.
Results and Discussion
The total number of live births in 2017-2018 was 1748 and 74 neonates were identified and treated for hyperbilirubinemia. The present study showed the incidence to be more in female babies than male babies. The female babies were about 55% and male babies were 44% (Table 1). The preterm babies were 21% and term babies were 78% (Table 1). The mode of delivery through LSCS was 56% and normal vaginal delivery was 43% (Fig 1). Hyperbilirubinemia seen in Multiparous was around 64% and in primiparous was around 35% (Fig 2). Majority of the newborns were in normal weights and physiological jaundice was the most common type of jaundice seen in newborns. Single surface phototherapy was the common treatment given to the newborns which was similar to other studies (Table 2). The next cause of jaundice was due to prematurity. There were various causes to jaundice which was shown in Table 2. A positive correlation was seen with birth weight and the peak bilirubin values in neonates (Table 3).
Table 1: Male and Female Ratio with Gestational Age in Percentage.
| Characteristics related with Neonatal Hyperbilirubinemia in percentage | ||
| Gender | Male | 44.59 % |
| Female | 55.40 % | |
| Gestational Age | Term | 78.37 % |
| Preterm | 21.62 % | |
Table 2: Birth weight, Treatment profile and Aetiology of Jaundice.
| Birth weight (in grams) and Treatment | percentage | Etiology | percentage |
| Normal (>2500 g) | 79.72 % | Cephalohematoma | 1.35 % |
| Low birth weight (1500 – 2500 g) | 16.21 % | Physiological jaundice | 66.21 % |
| Very low birth weight (1000-1500 g) | 2.70 % | Prematurity | 16.21 % |
| Extremely low birth weight (<1000 g) | 1.35 % | Sepsis | 6.75 % |
| Single surface phototherapy | 81.08 % | ABO incompatibility | 2.70 % |
| Double surface phototherapy | 2.70 % | Rh incompatibility | 1.35 % |
| Both(single and double surface phototherapy) | 14.86 % | Breast milk jaundice | 5.40 % |
| Triple and single surface Phototherapy | 1.35 % | – | – |
Table 3: Correlation of Birth Weight with Peak bilirubin levels.
| Groups | Mean+ SD | Correlation of Coefficient | Sig. |
| Birth weight (in grams) | 2.884 + 0.68 | r = +0.267 | 0.021
|
| Peak bilirubin (in gm/DL) | 14.90 + 3.51 |
Correlation is significant at 0.05 level (2-tailed)
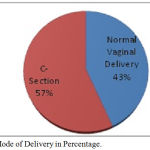 |
Figure 1: Mode of Delivery in Percentage.
|
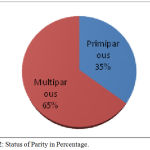 |
Figure 2: Status of Parity in Percentage.
|
Discussion
Mild increase in bilirubin level often disappears within two-three weeks in newborns whereas in-case of moderate to severe raised levels, an appropriate treatment is required[9]. Phototherapy, using conventional or fiber optic lights and exchange transfusion was the common and frequently used treatment to reduce the serum bilirubin levels. During phototherapy, exposure of skin to light source converts unconjugated bilirubin to water-soluble form and can be easily excreted by the normal mechanism. The blue-green light source was used in phototherapy for a better penetration into the skin and removes the unconjugated bilirubin by undergoing photochemical reaction [10]. Single, double and triple surface photo-therapies are available to decrease the bilirubin levels. Single surface phototherapy was found to be effective when compared to double surface which was used only to avoid the exchange transfusion [11]. In present study, only single surface phototherapy was used in major cases which was similar to previous studies. Exchange transfusion can be used in case if there is a risk of kernicterus, blood incompatibility or after intense phototherapy was unsuccessful [12]. Double volume phototherapy replaces 86% of blood and 63% in single volume phototherapy. Exchange transfusion may produce many adverse effects like thrombocytopenia, portal vein thrombosis, necrotizing enterocolitis , arrhythmia, cardiac, arrest, hypocalcemia, hypomagnesemia, hypoglycemia, respiratory and metabolic acidosis and other complications due to blood transfusion [13]. The practice of using the high dose intravenous immunoglobulin (iv IG) has reduced the need for exchange transfusion with Rh, ABO [14]. In present study, the absence of exchange transfusion indicates the lack of occurrence in the critical bilirubin levels in newborns. Krishna veni et al conducted a study to know the effect of gender on bilirubin levels and the study showed female babies to be more affected than male babies which was similar to our study [15]. Mostly term babies were affected with physiological jaundice which requires phototherapy for a short period as a treatment and this study also stipulates similar result [16].
Phenobarbitone, an antiepileptic drug has been used as a prophylactic treatment in the pre-term babies where there is a higher risk of jaundice. These drugs act by inducing the activity of uridine-di-phosphate glucuronosyl transferase enzyme and enhance the excretion of bilirubin and thereby reduce the concentration in newborn babies. Phenobarbitone can be used prophylactically in order to avoid exchange transfusion in babies which result in many complications.17 Alternate to conventional treatment, there are other pharmacological treatments to reduce neonatal jaundice. These include metalloporphyrins, clofibrate, bile salts, laxative, indole-3- carbinol and bilirubin oxidase which are under clinical trial. Metalloporphyrins, synthetic heme analogs can reduce the production of unconjugated bilirubin by competitively inhibiting heme oxygenase.18
Phenobarbitone, an antiepileptic drug has been used as a prophylactic treatment in the pre-term babies where there is a higher risk of jaundice. These drugs act by inducing the activity of uridine-di-phosphate glucuronosyl transferase enzyme and enhance the excretion of bilirubin and thereby reduce the concentration in newborn babies. Phenobarbitone can be used prophylactically in order to avoid exchange transfusion in babies which result in many complications [17]. Alternate to conventional treatment, there are other pharmacological treatments to reduce neonatal jaundice. These include metalloporphyrins, clofibrate, bile salts, laxative, indole-3- carbinol and bilirubin oxidase which are under clinical trial. Metalloporphyrins, synthetic heme analogs can reduce the production of unconjugated bilirubin by competitively inhibiting heme oxygenase [18].
A study conducted in India for a period of 7 years in a tertiary care hospital identified around 65% morbidity among extremely low birth weight babies [19]. Even,the chance of occurrence in kernicterus were more common in the very low birth weight than normal weight babies [20]. In present study,it is observed that the correlation of birth weight and peak bilirubin levels were statistically significant and this was supported by the data which indicated the presence of only 20% with a low birth weight and rest all have normal birth weight [21]. The study data also showed the absence of severe neonatal hyperbilirubinemia and a conventional treatment of phototherapy was only used. Mode of delivery also had influence to induce jaundice in newborns and there were higher chances of the jaundice in babies who were born by cesarean section than through normal vaginal delivery. In our study, around 56% of babies were delivered through cesarean section who were affected with jaundice when compared with normal delivery (43%) [22]. Mikael et al conducted a study to analyze various risk factors for non-hemolytic jaundice in neonates and identified primiparous to be one of the reason, and this was in contrary with the result of the present study[23].
Conclusion
Hyperbilirubinemia in neonates are more dangerous when they are not provided with appropriate treatment. Therefore in order to reduce the severity of jaundice in newborns, preventive steps should be taken in co-operation with physician and parents for early diagnosis and treatment of babies. Mothers can be educated about various factors which induce neonatal jaundice before delivery itself. A practice of routine bilirubin level assessment in the neonates before discharge will help in reducing re-admission of babies. Even with the availability of recent techniques like hour specific nomograms in identifying jaundice still, more research is required by research scientist to help the doctors by introducing easy techniques for early treatment for the babies.
Acknowledgements
The authors are thankful to Dr. Prashanth. R, 3rd year MD, Social and Preventive Medicine in helping for carrying statistical analysis.
Conflict of Interest
The authors declare that there is no conflict of interest
Funding source
There is no funding source.
References
- Aggarwal B, Agrawal A, Chaudhary P, Gupta G, Rana S, Gupta S. Neonatal Jaundice: Knowledge, attitude beliefs, and practices of postnatal mothers in a tertiary care hospital in Uttarakhand, India. Indian Journal of Child Health. 2017 Nov.22:603-8.
- Wan AS, Daud SM, Teh SH, Choo YM, Kutty FM. Management of neonatal jaundice in primary care. Malaysian family physician: the official journal of the Academy of Family Physicians of Malaysia. 2016;11(2-3):16.
- Kulkarni S.K., Dolas A.L. and Doibale M.K. Risk factors of neonates with indirect hyperbilirubinemia in a tertiary care hospital. International journal of basic and applied medical sciences.2014 january -april ;4(1):395-399
- Rasul CH, Hasan MA, Yasmin F. Outcome of neonatal hyperbilirubinemia in a tertiary care hospital in Bangladesh. The Malaysian journal of medical sciences: MJMS. 2010 Apr;17(2):40.
- Shetty A, Kumar BS. A study of neonatal hyperbilirubinemia in a tertiary care hospital. International Journal of Medical Science and Public Health. 2014 Oct 1;3(10):1289-93.
- Jamir S, Ngangom AS, Hijam D, Longkumer C, Dubey A, Singh MA, Singh KI. A study of neonatal hyperbilirubinemia in a tertiary care hospital in the north eastern region of India. International Journal of Current Research and Review. 2016 Oct 15;8(20):25.
- Scrafford CG, Mullany LC, Katz J, Khatry SK, LeClerq SC, Darmstadt GL, Tielsch JM. Incidence of and risk factors for neonatal jaundice among newborns in southern N epal. Tropical Medicine & International Health. 2013 Nov;18(11):1317-28.
- Rasul CH, Hasan MA, Yasmin F. Outcome of neonatal hyperbilirubinemia in a tertiary care hospital in Bangladesh. The Malaysian journal of medical sciences: MJMS. 2010 Apr;17(2):40.
- Woodgate P, Jardine LA. Neonatal jaundice: phototherapy. BMJ clinical evidence. 2015;2015.
- Cuperus FJ. Novel treatment strategies for unconjugated hyperbilirubinemia. University Library Groningen][Host]; 2011.
- Silva I, Luco M, Tapia JL, Pérez ME, Salinas JA, Flores J, Villaroel L. Single vs. double phototherapy in the treatment of full-term newborns with nonhemolytic hyperbilirubinemia. Jornal de pediatria.2009Oct;85(5):455-8.
- Ballot DE, Rugamba G. Exchange transfusion for neonatal hyperbilirubinemia in Johannesburg, South Africa, from 2006 to 2011. International scholarly research notices. 2016;2016.
- Bujandric N, Grujic J. Exchange transfusion for severe neonatal hyperbilirubinemia: 17 years’ experience from Vojvodina, Serbia. Indian Journal of Hematology and Blood Transfusion. 2016 Jun 1;32(2):208-14.
- El Habashy SA, Toaima DN, Gad GI, El Nazer MG. High dose intravenous immunoglobulin in Rh and ABO hemolytic disease of Egyptian neonates. Egyptian Journal of Pediatric Allergy and Immunology (The). 2014;12(1):21-6.
- Veni DV. The study on the effect of gender on serum bilirubin concentration in infants with neonatal hyperbilirubinemia. Int J Pharma Biosci. 2013;4:603-8.
- Mitra S, Rennie J. Neonatal jaundice: aetiology, diagnosis and treatment. British Journal of Hospital Medicine. 2017 Dec 2;78(12):699-704.
- Yeung CY, Field CE. Phenobarbitone therapy in neonatal hyperbilirubinaemia. The Lancet. 1969 Jul 19;294(7612):135-9.
- Dennery PA. Pharmacological interventions for the treatment of neonatal jaundice. InSeminars in neonatology 2002 Apr 1 (Vol. 7, No. 2, pp. 111-119). WB Saunders.
- Chawla D, Parmar V. Phenobarbitone for prevention and treatment of unconjugated hyperbilirubinemia in preterm neonates: a systematic review and meta-analysis. Indian pediatrics. 2010 May 1;47(5):401-7.
- Watchko JF, Maisels MJ. Jaundice in low birthweight infants: pathobiology and outcome. Archives of Disease in Childhood-Fetal and Neonatal Edition. 2003 Nov 1;88(6):F455-8.
- Gupta MK, Kakkar M, Sethi C, Malhotra AK. Pattern of morbidity and mortality in LBW neonates: a study from Jaipur. Journal of Evolution of Medical and Dental Sciences. 2014 Feb 10;3(6):1339-46.
- Garosi E, Mohammadi F, Ranjkesh F. The relationship between neonatal jaundice and maternal and neonatal factors. Iranian Journal of Neonatology IJN. 2016 Mar 1;7(1):37-40..
- Norman M, Åberg K, Holmsten K, Weibel V, Ekéus C. predicting nonhemolytic neonatal hyperbilirubinemia. Midirs Midwifery Digest. 2016 Jan 1;26(1):113.








