M.C. Jobin Christ, S. Dhulakshika, R. Divya, R. Kousalya and R. Aparna
Department of Biomedical Engineering, Rajalakshmi Engineering College, Chennai, India.
DOI : https://dx.doi.org/10.13005/bpj/1780
Abstract
This paper provides an insight into the non-contact vital parameter measurements, especially the heart rate of a person from a short distance. The increasing demand to new developments in healthcare technologies poses inevitability to the thought of easing the patient monitoring in a non-invasive and unobtrusive manner. Patients, who are in need of regular checkups, find the existing modes of electrode-based and probe-based monitoring, a discomfort. To make the monitoring environment comfortable for the patients and to take the results in a continuous and rapid manner, the non-contact heart rate measurement comes as a boon to the healthcare sector. This paper deals with miniaturized radar-based non-contact heart rate measurement using hand gestures in a precise manner. Though there were lots of methods proposed for contactless measurements, this approach comes with better accuracy and ease of handling.
Keywords
Comfortable; Gestures; Healthcare; Heart rate; Non-contact; Radar
Download this article as:| Copy the following to cite this article: Christ M. C. J, Dhulakshika S, Divya R, Kousalya R, Aparna R. A Novel Approach for Non-Contact Heart Rate Measurement. Biomed Pharmacol J 2019;12(3). |
| Copy the following to cite this URL: Christ M. C. J, Dhulakshika S, Divya R, Kousalya R, Aparna R. A Novel Approach for Non-Contact Heart Rate Measurement. Biomed Pharmacol J 2019;12(3). Available from: http://biomedpharmajournal.org/?p=28811 |
Introduction
Heart rate is one of the most commonly measured and monitored among other vital parameters such as respiration rate, blood oxygen saturation, arterial blood pressure, etc. Whatever the sensing principle or the monitoring method used, data referred to the heart rate is considered be the primary vital sign information which is used in both emergency and clinical situations. The post-processing of the data acquired by any method helps in patient heart diseases or abnormalities diagnosis. Noncontact detection and monitoring of human heart rate is a reliable and stable methodology that can be extended to wide range of applications in the fields of emergency and military healthcare. It can be the part of a low-power medical sensor network system in medical centers for collection and monitoring of certain physiological parameters.
In most cases, heart rate-monitoring techniques require contact between the person and the equipment which may cause discomfort for the person, while recording made without any physical contact can create a comfortable environment for the patient and a continuous recording by the physician. A radar-based sensing method helps in this regard and further developments can enhance the non-contact recording of heart rate in multi person scenario13.
A complete transmitter-receiver Doppler radar system, which uses a 4 GHz continuous wave radar signal transmission and receiving system, to extract base-band data from a phase-shifted signal to monitor several patients simultaneously and in different situations like standing, walking, or lying11.
A technique for monitoring vital signs using near-field coherent sensing (NCS) uses electromagnetic energy that is directed into the body tissue with energy higher than typical RF methods so that the backscattered signal from internal organs is implicitly amplified. At the same time, the shorter wavelength inside the body renders a small mechanical motion into a relatively large phase variation, which also increases the sensitivity. The far-field NCS signals were recorded at sampling points 1m in front of the chest and above the wrist and the demodulated heart signal and wrist pulse signal were found to match well with the known vibration15.
A system of two single-channel radars offset in space by a path length, which is equivalent to 90-degree phase shift was used. It provides an affordable way for exploiting microwave interferometry, through indented radar configuration, to overcome the null-point issues while monitoring vibrations from a distance. It can find immense application in both vital sign detection and structural vibration detection use-cases where affordable solution is sought2.
The existing methods use probes and electrode-gel based systems to acquire electrical activity of the heart from the person. The electrocardiography (ECG) is a technique to measure the electrical activity of the heart with the help of 12 lead electrode system by using surface electrodes placed at different locations on the surface of the skin. Phonocardiography (PCG) which consists essentially of recording and processing the acoustic waves produced by heartbeats travelling through the body up to the skin and this is one of the first heart monitoring methods developed and it is based on the observation that heart contractions produce acoustic waves travelling through the blood at the corresponding speed of sound. Echocardiography is also a painless non-invasive technique that uses sound waves to image movement of the heart. These images give details of the size and shape of the heart. They can also provide information on well-being of the heart’s chambers and valves.
Internal fetal heart rate monitoring uses an electronic transducer connected directly to the fetal skin. A wire electrode is attached to the fetal scalp or other body part through the cervical opening and is connected to the monitor. This type of electrode is sometimes called a spiral or scalp electrode. Internal monitoring provides a more accurate and consistent transmission of the fetal heart rate than external monitoring because factors such as movement do not affect it. Internal monitoring may be used when external monitoring of the fetal heart rate is inadequate, or closer surveillance is needed. Even though, the advancements in technology made possible, the wearable systems. The minimal obtrusive nature and the cost for developing such miniaturized systems are still constrains pertaining to wearable systems. Cardiotocography is used during pregnancy to monitor the fetal heart and contractions of the uterus. It is most commonly used in the third trimester. Its purpose is to monitor fetal well-being and allow early detection of fetal distress. It involves the placement of two transducers onto the abdomen of a pregnant woman. One transducer records the fetal heart rate using ultrasound. The other transducer monitors the uterine contractions. Some of the methods to measure is listed in the given table1:
Table 1: Summary of the different contact and non-contact methods for heart rate measurement
| Different methods | Types | Procedure |
| Contact
heart rate measurements |
Cardioto
-cography
|
Records the foetal heartbeat and the
uterine contractions during pregnancy- elastic belt is placed around the mother’s abdomen and measured. |
| Mobile
foetal heart rate monitor
|
Mobile machine
for checking fetal heart rate by placing probes over the mother’s abdomen |
|
| Ultrasound- foetal
heart rate monitor |
Probes are used
to measure the fetal heart rate by the principle of doppler effect. |
|
|
Non contact heart rate measurements |
Laser-based monitoring systems | Fiber-optical probe
is used to measure the heart rate by transmission and reflection of light. |
| Electro
Magnetic based monitoring systems |
Radar emits a
continuous stream of electro-magnetic radiation towards the subject to pick up the heart rate. |
Materials and Methodology
An open-source physical computing platform based on a simple microcontroller board, Arduino and its development environment IDE, for writing codes for the board, were used to provide necessary power supply to the physical board and necessary program was loaded onto the board using the software to measure the frequency shift and speed of the flow of blood.
The non-contact acquisition of the heart rate of an individual was done with the help of the microwave sensor HB100 that had within it a miniaturized transceiver Doppler radar module1. Though it had a wide coverage range of 7 meters, the distance preferred was only 20 centimeters between the hand and the sensor. The sensor was operated at a low potential of 5V. The radiation coming from the sensor was far below the safety limits. Hence these qualities made it a better choice used for recording.
As the acquired potential was in micro volts, necessary amplification and filtering from any external noise was required. That was done by making use of LM324 amplifier that served as the base for the linear amplifier and band pass filter design. The four amplifier stages within it, was an added advantage to reduction of complexity in the circuit.
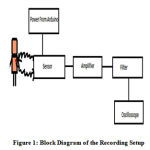 |
Figure 1: Block Diagram of the Recording Setup |
The electronic circuit for the recording setup involved the use of HB100 microwave sensor and the combination of a differentiator and an integrator, with different cut off frequencies, was incorporated into the LM324 Amplifier, hence giving rise to a linear amplifier with the band pass filter with a lower cut off frequency of 2Hz and an upper cut off frequency of 75Hz. The linear amplifier had a gain of 100 while the filter had a gain of 125.
The experiment was carried out by making the subject to sit and then the setup was kept at a distance of 50cm from the subject. The subject was asked to fold and unfold their right hand, rhythmically at a distance of 20 cm from the sensor.
The oscilloscope recorded the movement of the hand and at one point, after a response time of around 5 minutes; it recorded the electrical activity of the heart according to the hand gestures. The same was repeated for left hand. From both the observations, the heart rate was determined by calculating the R-R interval. The R-R interval was obtained from the oscilloscope.
 |
Figure 2: Non-Contact Recording Setup |
The time period of one minute (60 seconds) divided by the R-R interval would give the heart rate. The transceiver radar system was designed to operate reliably under different conditions. This non-contact measurement marks the new era of the completely unobtrusive and affordable systems that can improve better diagnosis and detection of anomalies in the population.
 |
Figure 3: Unfolding Gesture Detection |
 |
Figure 4: Folding Gesture Detection |
Cross Validation using Patient Monitor
The recordings were then cross validated by using patient monitor system, placing three surface electrodes on the skin of the subject at three different locations: at left wrist, at right wrist and at left foot ankle. The electrodes were then connected using leads and the probe is connected to the patient monitor. The patient monitor used was GOLDWAY UT6000A.
Cross Validation using Stethoscope
The recordings of about 10 subjects were then cross validated using stethoscope after validating with patient monitor to check the integrity of the results. The subject’s heart rate was counted by placing the diaphragm part of the stethoscope on the left side of the chest, the location at which, the heart sound was heard clearly. The heart beat was then counted for a minute and thus the values were cross checked with that of the non-contact recording setup.
Calculation
Heart rate is calculated using the formula,
![]()
Then the error difference between actual value (reading from patient monitoring system) and the experimental value (reading from non-contact sensor) is calculated using the formula,
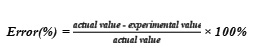
The error percentage can be used to indicate the accuracy of the system by the formula,
Accuracy (%) = 100-Error (%)
Results and Discussions
The cross validation by patient monitor system was useful in finding out the throughput of the system and its efficiency. The error rate was calculated as a result of cross validation. Figure 5 shows the results of the heart rate recording for 50 subjects and its comparison with that of the patient monitor.
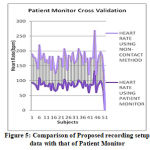 |
Figure 5: Comparison of Proposed recording setup data with that of Patient Monitor |
Figure 6 shows the corresponding error percentage. The sample recording result obtained along with its cross validation with that of patient monitor was shown in Figure 5. The waveforms of the non-contact recording setup were more or less similar to that of the patient monitor system.
 |
Figure 6: Error Percentage Graph |
 |
Figure 7: Recordings of Non-Contact Method and its comparison with that of Patient Monitor |
The waveforms obtained were not exactly the accurate wave pattern of electrocardiogram as the setup involves some noise due to probe and wires. The R wave peaks were prominent for almost all the subjects as that can be observed from the Figure 7.
From the Figure 6, it was found that both the recordings were almost matching with the minimal error in the range of (0 – 3) %. It was also found that many readings have 0% error.
The mean error rate was found to be 1.53% for the setup. The mean accuracy is 0.9846 and the relative accuracy is 98.46%
The integrity of the results was cross checked for ten subjects using stethoscope and its results were plotted and shown as Figure 8.
 |
Figure 8: Comparison of the results of proposed Non-Contact Method with that of stethoscope |
Heart rate is usually measured by placing electrodes on the chest (chest leads) and limb (limb leads). Electrocardiogram (ECG) is the waveform produced due to electrical activity of heart. The heart rate is determined by spontaneous action potential generation in the sinoatrial (SA) node and conduction in the atrioventricular (AV) node. It refers to the number of heartbeats over the course of a minute.
For the SA node, the rate of depolarization is altered, while the AV node’s rate of conduction is altered by autonomic nerve stimulation. This potential is not stopped here; it is carried up to peripheral endings. This was the reason that the PQRST waveform was obtained even from the hand gestures (peripheral endings).
Starling’s law of the heart states that higher venous blood return to the heart (also called the preload) will increase Stroke Volume (SV), which will in turn increase Cardiac Output (CO). This is because sarcomeres are stretched further when End Diastolic Volume (EDV) increases, allowing the heart to eject more blood. This will lead to an increase in Mean Arterial Pressure (MAP).
Exercise causes the heart to pump blood into the circulation more efficiently as a result of more forceful and efficient myocardial contractions, increased perfusion of tissues and organs with blood, and increased oxygen delivery. So, Hand Gestures for duration of more than 2 minutes will increase the heart rate momentarily due to changes in oxygen requirement to the muscle movement that induces increase in venous return to the heart, thereby increasing cardiac output. This causes increase in blood flow at the peripheral endings. As the effect of electrical activity is carried on towards the endings, pulse can be felt at the peripheral endings that are being recorded as ECG wave form. The response time was different for different people as observed in the experiment as their heart’s physiology is different for different persons. The left-hand response is more prominent as the heart is situated at the left side.
Conclusion
The focus of the paper is pertaining to contactless and unobtrusive measurement of heart rate from a very short distance. The signals, acquired using hand folding and unfolding gestures, were recorded from different subjects and the resulting signals were found to be similar to a normal ECG waveform. The estimated heart rate was found to more or less correlate with that of the acquired using ECG from a patient monitor. This indicates that microwaves are capable of penetrating through the skin and detects changes in blood flow at the peripheral endings, especially the left-hand movement showed better results. It was also observed that the recordings obtained using hand movements were more precise when compared to movement of objects.
A microwave sensor with a lower transmission frequency can be designed, within itself incorporating the filters and required amplifiers, to develop a miniaturized setup and a better penetration depth can, thus, be obtained to acquire the heart rate of an individual. Numerical analysis of the human heart rate using certain software applications can be developed that help to overcome the challenges in visual based analysis of the heart rate. A compact non-contact wireless wearable heart rate monitoring system can be designed for regular screening of the individual’s heart condition without the need to visit hospital.
With the knowledge of this paper, the methodology can further be extended to fetal heart rate monitoring without physical contact from the mother during labor that prevents discomfort and helps in early detection of still births, that are more likely to happen in case of any complications in the labor. This, in turn, provides an insight into rescue methods that help the doctors, save the neonate. As the maternal uterine muscle contraction varies according to changes in foetal movement, its vital signs and the foetal organ systems are more fragile in nature, even a faster heart beat can be more prominently reflect on mother’s uterine muscle contractions from which the foetal heart rate can be recorded. It would be an effective solution during labour as it avoids any physical contact from the mother and intermittent recordings at before, during and even after labour for duration of 20 minutes during the course of the labour would assist in monitoring the health of the foetus. The system can also be linked with mobile phone that records data regarding the health of foetal and reports it to the doctor using a mobile application in cases of emergency.
References
- Akshada Ravindra Patil and Professor Soumitra Das. Fetus Heart Rate Monitoring Using Smart Phone. International Journal of Innovations and Advancement in Computer Scienc.7(3):2347 – 8616. (2018).
- Andrew Gigie, Smriti Rani, Arijit Sinharay and Tapas Chakravarty.J. Novel Approach for Vibration Detection Using Indented Radar. Progress in Electromagnetics Research. 87(13):147–162. (2018).
- Gu, R. Li, H. Zhang, A. Fung, C. Torres, S. Jiang and C. Li.Accurate Respiration Measurement using DC-coupled Continuous-Wave Radar Sensor for motion-adaptive cancer radiotherapy. IEEE Transactions on Biomedical Engineering. 59(11): 3117–3123. (2012).
- Li, J. Lin and Y. Xiao. Robust Overnight Monitoring of Human Vital Signs by a Non–Contact Respiration and Heartbeat Detector. Proceedings of the 28th IEEE Engineering in Medicine and Biology Society Annual International Conference. 11(9): 2235-2238. (2006).
- Girbau. D, Ramos. A, Lázaro. A and Villarino. R. Remote Sensing of Vital Signs Using a Doppler radar and Diversity to Overcome Null Detection. IEEE Sensors Journal. 12(3): 512–518. (2012).
- Gorgas DL.Vital signs and patient monitoring techniques, Clinical Procedures in Emergency Medicine. 4th edition JR Roberts and JR Hedges, Eds Sauders., Philadelphia, USA. (2004).
- I.V. Mikhelson, P. Lee, S. Bakhtiari, T.W. Elmer, A.K. Katsaggelos and A.V. Sahakian. Noncontact millimeter-wave real-time detection and tracking of heart rate on an ambulatory subject. IEEE Transactions on Information Technology in Biomedicine. 16(5):927–934. (2012).
- Kao. T. J, Yan. Y, Shen. T, Chen, A. Y and Lin J. Design and analysis of a 60-GHz CMOS Doppler micro-radar system-in-package for vital-sign and vibration detection. IEEE Transactions on Microwave Theory and Techniques. 61(40):1649–1659. (2013).
- Kazemi. S, Ghorbani. A, Amindavar. H and Li. C. Cyclostationary approach to Doppler radar heart and respiration rates monitoring with body motion cancellation using Radar Doppler System. Biomedical Signal Processing and Control. 13(11):79–88. (2014).
- Li. C, Lubecke V.M, Boric-Lubecke. O and Lin.J. A review on recent advances in Doppler radar sensors for noncontact healthcare monitoring. IEEE Transactions on Microwave Theory and Techniques. 61(5): 2046–2060. (2013).
- Malikeh Pour, Ebrahim , Majid Sarvi and Mehmet Rasit Yuce. A Doppler Radar System for Sensing Physiological Parameters in Walking and Standing Positions. Sensors Journal of MDPI. 17(3):485. (2017).
- Ren. L, Wang. H, and Naishadham. K. Phase-based methods for heart rate detection using UWB impulse Doppler radar. IEEE Transactions on Microwave Theory and Techniques. 64(10): 3319–3331. (2016).
- Takuya Sakamoto, Pascal. J. Aubry, Shigeaki Okumura, Hirofumi Taki, Toru Sato and Alexander G. Yarovoy. Non-contact Measurement of the Instantaneous Heart Rate in a Multi-Person Scenario Using X-Band Array Radar and Adaptive Array Processing. IEEE Journal on Emerging and Selected Topics in Circuits and Systems, 8(2): 280 – 293. (2018).
- Tu. J, Hwang. T and Lin. J. Respiration rate measurement under 1-D body motion using single continuous-wave Doppler radar vital sign detection system. IEEE Transactions on Microwave Theory and Techniques. 64(6):1–10. (2016).
- Xiao nan Hui and Edwin C. Kan. Monitoring vital signs over multiplexed radio by near-field coherent sensing. Nature Electronics. 1(1): 74-78. (2017).
- Yanchun Zhang, Zhihui Li , Yan Gao and Chenggang Zhang. Effects of fetal microwave radiation exposure on offspring behavior in mice. Journal of Radiation Research.56(2): 261-268. (2014).
- Y. Yunqiang and A.E. Fathy . Development and implementation of a real-time see-through-wall radar system based on FPGA. IEEE Transactions on Geoscience and Remote Sensing. 47(5): 1270–1280. (2009).







