Manuscript accepted on :11-April-19
Published online on: 25-06-2019
Plagiarism Check: Yes
Reviewed by: Vinay Jagga
Second Review by: Xinhai Shan
Final Approval by: Prof. Juei-Tang Cheng
S.V. Shmeleva1, Ya.V. Shimanovskaya2, A.V. Romanova2, A.N. Vakulenko1, S.B.Kachalov3 and N.V. Logachev3
1K.G. Razumovsky Moscow State University of technologies and management (the First CossackUniversity), Moscow, Russia.
2Russian State Social University, Moscow, Russia.
3FGBOVO State University of Management (GUU), Moscow, Russia.
Corresponding Author E-mail: ilmedv1@yandex.ru
DOI : https://dx.doi.org/10.13005/bpj/1717
Abstract
An important element of the human musculoskeletal system is the hip joint, it has a complex structure. The hip joint is very vulnerable and can sometimes be severely affected. Injuries, degenerative processes in cartilage, and excessive physical exertion create conditions for destructive changes in the structures of the hip joint. Degenerative-dystrophic changes in the structure of the joint form the need for endoprosthetics. After endoprosthetics, a complex rehabilitation process is needed, which should be based on regular dosed physical exercises, which do not allow weakening the muscles, which provide movement in it, and rationally combine them with massage and hydro-procedures. In this way, it is possible to return the optimal motor ability of the limb after hip joint arthroplasty and to ensure a person’s return to his normal life. Improving the efficiency of recovery after hip arthroplasty can be continued with further research in this direction.
Keywords
Endoprosthetics; Hip Joint; Musculoskeletal System; Rehabilitation; Restoration
Download this article as:| Copy the following to cite this article: Shmeleva S. V, Shimanovskaya Y. V, Romanova A. V, Vakulenko A. N, Kachalov S. B, Logachev N. V. Overview of Modern Approaches to the Restoration of the Anatomical and Functional State of the Hip Joint in Various Pathologies. Biomed Pharmacol J 2019;12(2). |
| Copy the following to cite this URL: Shmeleva S. V, Shimanovskaya Y. V, Romanova A. V, Vakulenko A. N, Kachalov S. B, Logachev N. V. Overview of Modern Approaches to the Restoration of the Anatomical and Functional State of the Hip Joint in Various Pathologies. Biomed Pharmacol J 2019;12(2). Biomed Pharmacol J 2019;12(2). Available from: https://bit.ly/2KCtofD |
Introduction
Ontogenesis is often accompanied by the development of various dysfunctions and pathological processes1,2. The reasons for their appearance are the adverse effects of the environment on the human body3, a decrease in its reactivity and a hereditary predisposition to the development of various diseases4,5. Often, the developmental disorders in the body can be the musculoskeletal system and especially the joints6,7.
According to statistics, pathological changes in the hip joint occur at any age8,9. Their severity is so great that endoprosthesis of this joint can be prescribed to the patient10,11. This operation is quite difficult and requires subsequent long-term and systematic physical rehabilitation12.
Of great importance in the process of physical rehabilitation after hip joint arthroplasty, therapeutic physical training, as well as hydro-rehabilitation, physiotherapy and massage, is of great importance. Exercise in such patients should be aimed at improving muscle tone and improving motor function, especially in the area of the implanted joint, this has a positive effect on the recovery of patients after this operation13.
The main factor that determines the type and nature of physical therapy for total hip replacement is the state of the muscular system of this node of the body. Long-term abandonment of joints without effective treatment leads to muscle degradation. This is characteristic of both injuries and diseases – arthritis, arthrosis14.
Physical rehabilitation in the post-immobilization period plays a major role throughout the treatment cycle. It is an important way to restore not only the physical condition of the patient, but also his psycho-emotional attitude15.
Further development of options for the effective physical rehabilitation of individuals who have undergone hip joint arthroplasty, which could bring them back to normal life in a short time is very important.
Considering the importance of the problem, the following goal has been set: to consider the issues of restoring the anatomical and functional state of the hip joint after endoprosthesis replacement.
Material and Research Methods
The material of the study served 69 literary sources. As methods of the study, methods of analysis and synthesis, methods of induction and deduction, and a method of generalization were used.
Research Results
Morphofunctional Features of the Hipjointon the Background of High Muscular Activity
The structure of the hipjoint provide sunhindered flexion of the hip – up to contact with the frontsur face of the body. Such a movement can easily be performed by any person — noteven playing sports, if the lower legisbentat the knee joint by 90° or more. When the legissignificantly extended, there are difficulties associated witht hemanifestation of passive insufficiency of the muscles of the posteriorsurface of the thighand the pelvicregion. However, system atictraining will help to overcome these difficulties: after 3 months, 14-15-year-olds can perform max for ward witht heirlegsextendedinfull16,17.
When the thigh of a jog leg is retracted at the moment of crossing the barrier, a different situation arises. For ballet dancers and gymnasts the abduction of the supine thigh reaches 150-160°. Due to the rotation of the femur outwardly, the large skewer retreats back and bypasses the upper edge of the acetabulum, which projects most outwardly. Runners across the barriers in the position characteristic of crossing the barrier, supination is practically absent18.
The lowest passage of the center of gravity of the athlete’s body over an obstacle is provided by a 90° thigh abduction. However, the combined action of the restraints (bones) and movement brakes (tension on the pubic-femoral and medial parts of the iliophora ligament) stops it at the border of 62-71°. This is the limit to which an athlete can be reached with the complete elimination of passive insufficiency of the muscles of the inner surface of the thigh – antagonists to movement. Runners at 110 m compensate for the lack of lead by some curvature of the spine in the lumbar spine (and with a strong limitation in the chest) and by raising the corresponding half of the pelvis. In women who overcome barriers with a height of 76.2 cm, isolated lead is enough. However, the absolute majority of athletes still tilt the pelvis in the direction of the jogging leg, whose knee runs at a height of 15-20 cm from the barrier. The elimination of these unmotivated movements is a certain reserve of the running speed19.
Due to the difficulties in achieving the required range of hip abduction, the inclination of the body forward at the moment of passing the barrier plays an important role. It not only allows you to lower the trajectory of the center of gravity, but also facilitates the supination of the thigh. Even a slight supination shifts back the big spit and increases the hip abduction almost to the required 90°. Rigidly fixing the iliac crests and giving the body an inclined position characteristic of the hurdlers over the obstacle, we determined that the average passive abduction of the thigh of the jogging leg in 10 male masters of sports is 82.9°. Withdrawal of the other hip from them was only 73.7° – with a high confidence of the differences in the scope of this movement on the jog and swing leg. However, at the moment of running this limit, the athlete cannot be reached, since he is actively withdrawing his hip. The active lead, measured in the laboratory with the same hurdler, was: on the jog leg – 75.4°, on the fly leg – 68.9°. Consequently, the inclination of the pelvis toward the jogging foot when passing high barriers is objectively necessary20.
The first problem is solved quite easily. Regular use of appropriate exercises for 3 months increases the elasticity of the adductors to such a level that they no longer offer resistance to hip abduction. This limits the effect of these exercises. However, the advantage of hurdler over non-sports, as well as the excess of the scope of this movement with the jogging leg compared to the flywheel, proves the possibility of a deeper, arbitrary correction of limiting hip abduction21.
One of the most difficult elements in gymnastics is the “cross splits”, where it is necessary to simultaneously withdraw both thighs by 90°. This eliminates the possibility of lateral tilt of the pelvis and the friendly bending of the spine. The gymnast compensates for the lack of abduction of the hip by a large inclination of the pelvis forward and the associated deep deflection in the lumbar spine, as well as supination of the legs. These movements bring the big skewer back, where the acetabulum is sloped down-in, and the movement stops come in contact much later. In addition, in the “transverse splits” hip abduction is performed passively – under the action of body weight. Still, this element is performed only by those gymnasts who are characterized by a high level of general flexibility and adequate individual characteristics of the structure of the hip joint22,23.
In many sports, the degree of extension of the hip at the hip joint is of great importance. Limit its scope is necessary when performing longitudinal “splits”, jump “ring” and many other elements in the gym; with the last two steps in the high jump; when the bar is pulled in a “scissors” way; when pushing away in a pole vault; with a deep lunge in fencing – so as not to lose visual control over the situation22,24.
The scope of this movement ranges from 57 to 15°. Such a significant scatter of data is explained by the degree of accuracy and validity of measurements – in particular, by subtracting from the general arc of the movement of the friendly extension of the spine and pelvic tilt. In this regard, active extension, accompanied by overcoming the passive resistance of the quadriceps, will be even less15,25.
Thus, it turns out that active training does not have a direct effect on the hip joint. Moreover, an attempt to directly influence it (for example, extending the femur while tilting the pelvis backwards in a lunge) quickly leads to pain in the anterior inferior iliac spine and inter-invertal line – at the sites of attachment of the ilio-femoral ligament (in the extension process, it stretches and twists)26,27. It becomes clear that regular exercise can create conditions for destructive changes in the articular cartilage of the hip joint and the formation of an early need for its endoprosthesis.
Traumaticinjuries of the Hipjoint
Joint injuries are a large group of injuries that differ in their consequences as well as severity. They include ligament damage, bruises, dislocations, intra-articular fractures, etc.28. Causes of joint injuries can be sports or domestic injuries, accidents, criminal incidents, industrial accidents, natural or industrial disasters. Constant symptoms of injury are: pain, swelling and limited movement13,29.
Failures and dilutions in most cases are caused by a pressure on a constricted thigh, or a force applied to a pelvic bone. This is most often caused during dormant traffic situations, fatigue or jumping from a height. The front end is a critical condition that requires immediate displacement. The burden of reversing the wake-ups of the system is affected by the flow of the affected vascular systems, and the high development of the hubs. This condition is especially dangerous for elderly people, whose fracture of the structures of the hip joint is diagnosed several times more often than in young people30.
Coxitis of the hip joint (arthritis of the hip joint) is an inflammatory process that occurs in the tissues of the joint. This disease can be caused by systemic infections that reach the joint with blood flow, excessive stress on the joint, metabolic disorders. In addition, coxit can develop as a complication of influenza, acute respiratory viral infection and other acute or chronic infectious processes. Often the cause of the pathology of the hip joint can be the following conditions.
Aseptic necrosis is a partial or complete death of the tissues of the femoral head, developing against the background of alcohol abuse, a long course of treatment with hormonal drugs, injuries left without treatment31.
Hip dysplasia is a congenital dislocation caused by bone development defects. These include underdevelopment, “flattening” of the acetabulum, irregular size or shape of the femoral articular head, improper mutual position of bone structures, and excessive elasticity of ligaments that are unable to hold the femoral heads in the acetabulum32,33.
Dislocations and subluxations in most cases are caused by falling on the bent thigh, on the knee or applying force to the pelvic bone. Most often this occurs during road accidents, falls or jumps from a height34.
Fracture of the hip joint is an extremely dangerous condition that requires immediate medical attention. The severity of fractures of the hip joint is due to the passage of important blood vessels next to it, and a high risk of bleeding or thrombosis. This condition is especially dangerous for elderly people, in whom the fracture of the hip joint structures is diagnosed several times more often than in young people35.
Tendinitis-inflammation of the tendons of the femoral muscles attached to the hip joint occurs due to excessive loads, injuries or as a complication of the inflammatory process in other structures left untreated36.
Stretching the ligaments of the hip joint is one of the most common States of traumatic origin among professional athletes. Excessive amplitude of hip movement and a large number of loads combined with lack of rest are the most common causes of stretching36,37.
Ligament rupture – complete or partial — is a rare condition for the hip joint. To break needs to be applied a large enough force in combination in violation of the axis of the body (for example, direct the position of the body c sharp abduction of the hips to the side). Most often, such injuries are diagnosed after road accidents. Any injury to the hip joint leads to the beginning of dystrophic changes in it with the development of degenerative changes and deterioration of functioning36,38.
Thus, it is clear that the hypotrophy of the leading and diverting muscles of the thigh leads to the loss of a large area of the vascular network that feeds the joint. Traumatization of structures is an important cause of its morphofunctional changes, which will require a serious therapeutic effect.
The Problem of Joint Replacement
Joint replacement is one of the main methods of surgical treatment of patients with joint diseases39. Such surgical intervention is a mandatory component of rehabilitation therapy of patients with degenerative diseases of the musculoskeletal system. This makes it possible to relieve pain and improves the quality of human life, returning mobility to his joints13.
Determining the indications and contraindications for surgery, it is necessary to assess a number of factors: the patient’s consent to the operation, changes in the data of x-ray examination; saturation of pain in the joints; information about the patient (somatic condition, age, nature of previous surgical therapy, sex);the level of severity of functional damage40,41.
In the process of choosing a method of treatment, the phase of the disease is of great importance. The main clinical symptom of joint damage is the intensity of the pain syndrome. At the same time, the pain is accompanied by various functional pathologies and radiological manifestations, which become strongly expressed in the final phases of the disease16.
Thus, it is necessary to conduct a comprehensive diagnosis in a hospital, and surgery should be done at the stage of remission. Limitation of limb functioning due to joint damage, together with intense pain, is considered a significant indicator for joint prosthesis42.
To date, human age is not a factor affecting joint replacement. More important is the assessment of the patient’s somatic condition, needs, level of activity, lifestyle and desire to lead a full life. There are a number of indications for joint replacement surgery39: osteoarthritis 3-4 x-ray phase; intense pain and impaired functionality of the limbs in the case of no effectiveness of conservative therapy and the detection of x-ray changes, aseptic necrosis of the femoral head, in which there is a strong deformation of the head, bone and fibrous ankylosis. Also, endoprosthesis is carried out when there is damage to the articular tissues in the presence of rheumatoid arthritis, initial chronic arthritis and other rheumatoid pathologies, in which radiological bone-destructive changes occur. Joint replacement is carried out in the case of post-traumatic changes, in which there is severe pain and there is a violation of the supporting functions43. In addition, endoprostheticsis carried out in the case of clinical detection of shortening of the limb, where the joint surfaces are affected. Aseptic necrosis of the femur and tibial condyles with progressive varus or valgus deformity is another indication for joint replacement surgery44,45.
Contraindications to endoprosthesis include a negative somatic state of the patient, the probability of postoperative and intraoperative consequences and the presence of severe concomitant diseases that increase the anesthetic risk, as well as the detection of infectious foci46,47.
In some cases, options for phased surgical treatment with prior restoration of the functionality of other joints are considered. Due to this, the patient is able to stand and use crutches while walking 15,48.
The most common complications that can develop as a result of endoprosthesis replacement include instability of prosthesis elements49,50. Also, the negative factors in joint replacement include bone regeneration disorders that occur due to the progression of secondary osteoporosis51,52.
It was found that the occurrence of osteoporosis and the probability of instability of the endoprosthesis in rheumatic disease caused by the influence of the underlying disease, the complexity of functional disorders, the intensity of inflammation. Moreover, instability often occurs after taking drugs that violate the process of adaptation of bone tissues to heavy loads and inhibit local growth factors. For these reasons, the probability of endoprosthesis instability is significantly increased 53,54. In the event of instability, in which there is severe pain and a violation of the supporting capabilities of the limb, it is often necessary to carry out revision arthroplasty of the hip joint13,55.
The following types of arthroplasty are currently performed39:
Partial prosthetics. Removal of the femoral head and neck. The articular bed is made with the help of materials of artificial origin. Applying a special pin, a prosthesis is attached to the femur.
Total joint replacement. It involves the replacement of the hip joint. The endoprosthesis can be made of different materials. Now there are more than 200 different designs. Selected prosthesis individually, be sure to take into account the age, weight and health of the patient (figure 1).
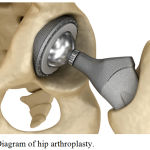 |
Figure 1: Diagram of hip arthroplasty.
|
Replacement of joint surfaces. Minimal surgical intervention is carried out. Is articulate the bed, the head of the femur fits over the hood, ensuring normal movement of the joint.
Thus, the pathology of the hip joint is often expressed very strongly, which requires replacement. This type of surgery is not very simple. After such an operation, the patient needs a rational physical rehabilitation.
Discussion
Rehabilitation after hip replacement is an integral stage of postoperative treatment aimed at restoring muscle tone and leg functionality. Rehabilitation is to limit (the features of) exercise in the period after the operation and during execution of the therapeutic physical training56,57. In rehabilitation after the endoprosthesis there are three periods: early, late and remote. For each of them a certain complex of gymnastics has been developed58. After hip replacement, an individual recovery plan consisting of different stages is developed for patients. This ensures the restoration of the patient’s adaptation to the prosthesis and the training of movements with it. Rehabilitation usually takes about two months. In older people, rehabilitation time can reach six months. Moving with crutches is allowed in the first week after surgery59.
The basic principles of the recovery period after hip replacement are: early onset; individual approach during rehabilitation; sequence; continuity; integrated approach30.
The absence of rehabilitation after endoprosthesis threatens with the appearance of dislocation of the endoprosthesis head due to the weakness of the ligaments, periprosthetic fracture, development of neuritis and other complications43.
Rehabilitation after any type of joint surgery, including hip replacement for an endoprosthesis, is performed by a rehabilitation doctor and (or) a physical therapy doctor. He will make an individual program taking into account the physical condition of the patient, the degree of adaptation to physical activity, his age, the presence of concomitant diseases.
Persistence, desire to get better, clearer implementation of the recommendations of doctors – the main criteria of a positive outcome of rehabilitation after surgery arthroplasty59.
Late rehabilitation after hip replacement begins 8-10 weeks after surgery and lasts up to 3 months. The duration of rehabilitation for each patient varies slightly depending on his age and other factors (figure 2)34,66.
 |
Figure 2: Rehabilitation after arthroplasty – long process.
|
Rational motive mode during rehabilitation involves training the patient to physical activity in everyday life. Therapeutic physical culture is supplemented by physiotherapy (mud or paraffin applications, balneotherapy, laser therapy) and massage60,61.
Adaptive motor mode in the long-term period is expanded at the expense of physical therapy on simulators. By this time, the ligaments and muscles have become stronger enough after surgery, so the intensity of the loads can be increased62.
Hydro-rehabilitation is the improvement of a person with the help of water, in order to form a qualitatively new higher level of his motor and social activity. In the process of hydrorehabilitation use of the ability of water treatments that have on the human body a complex effect. The effects of water itself (chemical, temperature and physical effects) are important, which is supplemented by hydrotherapy63,64.
Most often hydrotherapy includes: showers (Charcot, contrast, Vichy, Underwater shower-massage) and baths (hydromassage, pearl). Very popular therapeutic physical culture in the water – hydro-Kinesis therapy56. It provides maximum relaxation of all muscle groups, reduces the load on the body and facilitates exercise. These classes are suitable for people who find it difficult to perform classical exercises because of muscle weakness, severe pain. The main task of stimulating motor activity in water is the restoration of normal physical condition through active and passive movements. Staying in the water accelerates metabolism, increases thermogenesis, accelerates blood vessels, develops the respiratory system. In some cases (in case of serious injuries and diseases of the musculoskeletal system, paralysis), the facilitation of exercise is achieved by increasing the water temperature65.
Physical activity in water has a restorative effect on the body, increases joint mobility, develops muscles and relieves pain. In addition, at low temperature Aqua gym hardens the body, and at high promotes muscle relaxation. Effective use of hydrokinesotherapy in the form of therapeutic swimming66. Pool water (t-30-33°C) has a positive effect on blood circulation in the area of the operated joint. Movements performed in water, require less effort of the patient due to the apparent loss of weight of a body that facilitates the contraction of weakened muscles, greatly reduces stress and allows in the short term to achieve greater range of motion67. Resistance to water jet also has a healing effect. In addition, during classes in the pool, a certain psychotherapeutic effect is achieved. Light and painless movements in the water environment improve the health of patients and inspire them to believe in recovery68. After discharge from the hospital, the patient is supposed to keep a diary of physical activity. Physical activity should be regular. They should be combined with breathing exercises69.
Thus, anatomical and functional recovery of the hip joint after endoprosthesis replacement should be based on regular physical activity. They are possible on simulators, air and water environment with the use of physiotherapy and massage.
Conclusion
The hip joint plays an important role in human movement. It has a perfect structure. Despite this, this joint is very vulnerable and can sometimes be severely affected. Injuries, degenerative processes in the cartilage and excessive exercise can create conditions for destructive changes in the structures of the hip joint. The appearance of degenerative-dystrophic changes in the structure of the joint forms the early need for endoprosthetics. Subsequently, a complex rehabilitation process is required, which should be based on regular dosed physical exercises that do not allow the muscles to weaken, providing movement in it, they should be rationally combined with massage and hydro procedures. This effect is able to return the optimal motor ability of the limb after hip replacement and provide a person with a return to his normal life.
Conflict of Interest
There is no conflict of interest.
Financing Sources
The study was conducted at the expense of the authors.
References
- Medvedev IN, Skorjatina IA, Zavalishina SYu. Vascular control over blood cells aggregation in patients with arterial hypertension with dyslipidemia. Cardiovascular therapy and prevention, 15(1):4-9 (2016).
- Zavalishina SYu, Medvedev IN. Features aggregation erythrocytes and platelets in old rats experiencing regular exercise on a treadmill. Advances in gerontology, 29(3):437-441 (2016).
- Shmeleva SV, Yunusov FA, Morozov YUS, Seselkin AI, Zavalishina SYU. Modern Approaches to Prevention and Correction of the Attorney Syndrome at Sportsmen. Prensa Med Argent, 104:2 DOI: 10.4172/0032-745X.1000281 (2018).
- Skoryatina IA, Zavalishina SYu. Impact of Experimental Development of Arterial Hypertension and Dyslipidemia on Intravascular Activity of Rats’ Platelets. Annual Research & Review in Biology, 14(5):1-9 (2017) doi: 10.9734/ARRB/2017/33758 (2017).
- Morozova EV, Shmeleva SV, Rysakova OG, Bakulina ED, Zavalishina SYu. Psychological Rehabilitation of Disabled People Due to Diseases of the Musculoskeletal System and Connective Tissue. Prensa Med Argent, 104:2 DOI: 10.4172/0032-745X.1000284 (2018).
- Skoryatina IA, Zavalishina SYu, Makurina ON, Mal GS, Gamolina OV. Some aspects of Treatment of Patients having Dislipidemia on the Background of Hypertension. Prensa Med Argent, 103:3. doi: 10.4172/lpma.1000250 (2017).
- Zavalishina SYu. Physiological Dynamics of Spontaneous Erythrocytes’ Aggregation of Rats at Last Ontogenesis. Annual Research & Review in Biology, 13(1):1-7. doi: 10.9734/ARRB/2017/33616 (2017).
- Belozerova TB, Agronina NI. Independent Quality Estimation of Social Services: Rendering to Patients and Invalids. Prensa Med Argent, 103:4. doi: 10.4172/lpma.1000255 (2017).
- Agronina NI, Belozerova TB. Rendering Social Services Assessment by Social Service Organizations in Belgorod and Kursk Regions in Russia. Prensa Med Argent, 103:4. doi: 10.4172/lpma.1000256 (2017).
- Belozerova TB, Agronina NI. The Development of the Social Service System in Russia. Prensa Med Argent, 103:4. doi: 10.4172/lpma.1000257 (2017).
- Medvedev IN. Correction of primary hemostasis in patients suffering from arterial hypertension with metabolic syndrome. Klinicheskaia meditsina, 85(3):29-33 (2007).
- Dreving EF. Traumatology. Moscow: Publishing Cognitive Book Press, 224 (2002).
- Kovalersky GN, Silin LL, Garkavi AV. Traumatology and Orthopedics. Moscow: Akademiya, 75-76.(2005).
- Tsykunov MB. Principles of drawing up rehabilitation programs for injuries in athletes. Modern problems of sports traumatology and orthopedics. Moscow, 75-77 (2005)
- Tkacheva ES. Physiological Features of Platelets in Milk and Vegetable Nutrition Piglets. Biomedical & Pharmacology Journal, 11(3):1437-1442. http://dx.doi.org/10.13005/bpj/1508 (2018).
- Zavalishina SYu. Physiological Features of Hemostasis in Newborn Calves Receiving Ferroglukin, Fosprenil and Hamavit, for Iron Deficiency. Annual Research & Review in Biology, 14(2):1-8. doi: 10.9734/ARRB/2017/33617 (2017).
- Mukhin VM. Physical Rehabilitation. Kiev: Olympic literature, 62 (2000).
- Jeffrey G. Physical examination of the musculoskeletal system. Moscow: Publishing House Panfilova, 472 (2014).
- Chinkin AS, Nazarenko AS. Physiology of sport. Moscow: Sport, 120 (2016).
- Perova EI. Physical rehabilitation after injuries as a condition for improving the quality of life of athletes. Moscow, 36-39.(2007).
- Gross J, Fetto J, Rosen E. Physical examination of the musculoskeletal system. Moscow: Publisher Panfilova, 472.(2013).
- Medvedev IN. Vascular-platelet interaction in pregnant cows. J. Agric. Sci, 23(2):310-314 (2017).
- Medvedev IN, Danilenko OA. Complex correction of vascular hemostasis in patients with arterial hypertension, metabolic syndrome, and recent ocular vessel occlusion. Russian Journal of Cardiology, 4:15-19 (2010).
- Oshurkova JuL, Glagoleva TI. Physiological Activity of Platelet Aggregation in Calves of Vegetable Feeding. Biomedical & Pharmacology Journal, 10(3):1395-1400 (2017).
- Novozhilov DA. Basics of traumatology of the musculoskeletal system. Leningrad: Medicine, 320. (2007).
- Oshurkova JuL, Medvedev IN, Fomina LL. Platelets’ Aggregative Properties of Ireshire Calves in the Phase of Dairy-vegetable Nutrition. Annual Research & Review in Biology, 16(4): 1-6. doi: 10.9734/ARRB/2017/35868 (2017).
- Vainshten VG. Guide to traumatology. Leningrad: Medicine, 352 (1979).
- Glagoleva TI, Zavalishina SYu. Aggregative Activity of Basic Regular Blood Elements and Vascular Disaggregating Control over It in Calves of Milk-vegetable Nutrition. Annual Research & Review in Biology, 12(6):1-7. doi: 10.9734/ARRB/2017/33767 (2017).
- Medvedev IN, Gromnatskii NI. Effect of amlodipine on intravascular thrombocyte activity in patients with arterial hypertension and metabolic syndrome. Klinicheskaia meditsina, 83(2):37-39 (2005).
- Epifanov VA. Rehabilitation in traumatology and orthopedics. Moscow: GEOTAR – Media, 416 (2015).
- Eremeyshvili AV. Human Anatomy. Yaroslavl: Yaroslavl State University, 154 (2012).
- Vorobyeva NV. Physiological Reaction of Erythrocytes’ Microrheological Properties on Hypodynamia in Persons of the Second Mature Age. Annual Research & Review in Biology, 20(2):1-9. doi: 10.9734/ARRB/2017/37718 (2017).
- Epifanov VA, Yumashev GS. Operative traumatology and rehabilitation of patients with injuries of the musculoskeletal system. Moscow: Medicine, 283 (2003).
- Evseev SP, Kurdybailo SF, Malyshev AI, Gerasimova GV, Potapchuk AA, Polyakov DS. Physical rehabilitation of persons with disabilities of the locomotor system. Moscow: Soviet Sport, 488 (2010).
- Evdokimenko P. Osteoarthritis of the hip joints: Healing Gymnastics. Moscow, 96 (2012).
- Amelina IV, Medvedev IN. Relationship between the chromosome nucleoli-forming regions and somatometric parameters in humans. Bulletin of Experimental Biology and Medicine, 147(1):77-80 (2009).
- Kutafina NV. Platelet Parameters of Holstein Newborn Calves. Annual Research & Review in Biology, 15(2):1-8. doi: 10.9734/ARRB/2017/35214 (2017).
- Briggs T. Surgical orthopedics. Stenmore Guide. Moscow: Panfilov Publishing House, 320 (2014).
- Sizov AA. Investigation mistakes in investigation of crimes of foreign citizens, committed in the territory of Russia. Biosciences Biotechnology Research Asia, 12(1). http://www.biotech-asia.org/?p=5452> (2015).
- Dubrovsky VI. Sports Medicine. Moscow: Vlados Humanitarian Publishing Center, 157 (2008).
- Popov SN. Physical Rehabilitation. Rostov-on-Don, 127 (2005).
- Sizov АА, Zavalishina SJ. Russian Criminal Legislation in Prevention of Sexually Transmitted Diseases in the Territory of the Russian Federation. Biology and Medicine (Aligarh), 7(5): BM-142-15, 5 pages (2015).
- Skoryatina IA, Zavalishina SYu. A Study of the Early Disturbances in Vascular Hemostasis in Experimentally Induced Metabolic Syndrome. Annual Research & Review in Biology, 15(6):1-9. doi: 10.9734/ARRB/2017/34936 (2017).
- Skoryatina IA, Medvedev IN, Zavalishina SYu. Antiplatelet control of vessels over the main blood cells in hypertensives with dyslipidemia in complex therapy. Cardiovascular therapy and prevention, 16(2):8-14 (2017).
- Sorokovikov VA, Sidorov GV, Shurygina IA, Chernikova OM. State of the perspectives of the implementation of innovative technologies in traumatology and orthopedics. Bulletin of the East-Siberian Scientific Center of the Siberian Branch of the Russian Academy of Medical and Medical Sciences, 4-1:332-334 (2011).
- Zavalishina SYu, Medvedev IN. Comparison of opportunities from two therapeutical complexes for correction of vascular hemostasis in hypertensives with metabolic syndrome. Cardiovascular therapy and prevention, 16(2):15-21 (2017).
- Medvedev IN. Platelet functional activity in clinically healthy elderly. Advances in gerontology, 29(4):633-638 (2016).
- Slobodskoy AB, Osintsev EYu, Lezhnev AG. Complications after hip arthroplasty. Bulletin of Traumatology and Orthopedics N. Priorov, 3:59-63 (2011).
- Medvedev IN. A comparative analysis of normodipin and spirapril effects on intravascular activity of platelets in patients with metabolic syndrome. Terapevticheskii Arkhiv, 79(10):25-27 (2007).
- Belokrylov NM, Sharova LV. Therapeutic physical culture in orthopedics and traumatology. Perm, 47-49 (2015).
- Medvedev IN. Neuropsychologicalchanges in cognitive function during the transition of the elderly in old. Advances in gerontology, 28(3):479-483 (2015).
- Ranu F. European experience in the management of patients with osteoarthritis. Rheumatology, 32:2-3 (2013).
- Glagoleva TI, Zavalishina SYu. Aggregation of Basic Regular Blood Elements in Calves during the Milk-feeding Phase. Annual Research & Review in Biology, 17(1):1-7. doi: 10.9734/ARRB/2017/34380 (2017).
- Glagoleva TI, Zavalishina SYu. Physiological Peculiarities of Vessels’ Disaggregating Control over New-Born Calves’ Erythrocytes. Annual Research & Review in Biology, 19(1):1-9. doi: 10.9734/ARRB/2017/37232 (2017).
- Epifanov VA. Healing Fitness. Moscow: GEOTAR-Media, 568 (2014).
- Medvedev IN. The Impact of Durable and Regular Training in Handto-hand Fighting Section on Aggregative Platelet Activity of Persons at the First Mature Age. Annual Research & Review in Biology, 15(2):1-6. doi: 10.9734/ARRB/2017/35048 (2017).
- Simonenko VB, Medvedev IN, Mezentseva NI, Tolmachev VV. The antiaggregation activity of the vascular wall in patients suffering from arterial hypertension with metabolic syndrome. Klinicheskaia meditsina, 85(7):28-30 (2007).
- Popov GI, Samsonov AV. Biomechanics of motor activity. Moscow: Academy Publishing Center, 320 (2014).
- Zhuravleva AN, Graevskaya ND. Sports medicine and physical therapy. Moscow: Medicine, 433 (2005).
- Medvedev IN. Physiological Dynamics of Platelets’ Activity in Aged Rats. Annual Research & Review in Biology, 18(2):1-6. doi: 10.9734/ARRB/2017/36821 (2017)
- Kozlova LV. Basics of rehabilitation for medical colleges. Rostov-on-Don: Phoenix, 475 (2014).
- Markov LN. Physical rehabilitation for injuries of the musculoskeletal system in athletes. Moscow, 118 (2007).
- Medvedev IN, Skoryatina IA. Erythrocyte aggregation in patients with arterial hypertension and dyslipidemia treated with pravastatin. Klinicheskaia meditsina, 92(11):34-38 (2014)
- Dyachkov MP. Therapeutic physical culture and methods of recovery. Moscow, 134 (2014).
- Bonkalo TI, Shmeleva SV, Zavarzina OO, Dubrovinskaya EI, Orlova YL. Peculiarities of interactions within sibling subsystem of a family raising a child with disabilities. Research Journal of Pharmaceutical Biological and Chemical Sciences, 7(1):1929-1937 (2016).
- Medvedev IN, Skoryatina IA. Pravastatin in correction of vessel wall antiplatelet control over the blood cells in patients with arterial hypertension and dyslipidemia. Cardiovascular therapy and prevention, 13(6):18-22 (2014).
- Lenchenko E, Lozovoy D, Strizhakov A, Vatnikov Y, Byakhova V, Kulikov E, Sturov N, Kuznetsov V, Avdotin V, Grishin V. Features of formation of Yersinia enterocolitica biofilms. Veterinary World, 12(1):136-140 (2019).
- Suleymanov SM, Usha BV, Vatnikov YA, Sotnikova ED, Kulikov EV, Parshina VI, Bolshakova MV, Lyshko MU, Romanova EV. Structural uterine changes in postpartum endometritis in cows. Veterinary World, 11(10):1473-1478 (2018).
- Yousefi M, Hoseini SM, Vatnikov YA, Nikishov AA, Kulikov EV. Thymol as a new anesthetic in common carp (Cyprinus carpio): Efficacy and physiological effects in comparison with eugenol. Aquaculture, 495:376-383 (2018).







