Manuscript accepted on :04-Mar-2019
Published online on: 28-06-2019
Plagiarism Check: Yes
Reviewed by: Arulmani Thiyagarajan
Second Review by: Stefano Omboni
Final Approval by: Md. Mahmudul Hasan
Amirul Fikri Rizfan1, Kalvin Ghosh1, Ahmad Mustaqir1, Resni Mona2, Jannathul Firdous2 and Noorzaid Muhamad*2
1Faculty of medicine, Universiti Kuala lumpur Royal College of Medicine Perak, No.3, Jalan greentown, 30450, Ipoh, Perak, Malaysia.
2Cluster for Integrative Physiology and Molecular Medicine (CIPMM), Faculty of Medicine, Universiti Kuala Lumpur Royal College of Medicine Perak, Jalan Greentown, 30450 Ipoh, Perak, Malaysia.
Corresponding Author E-mail: noorzaid@unikl.edu.my
DOI : https://dx.doi.org/10.13005/bpj/1699
Abstract
Due to continuous debate of incompatible results of blood pressure by the two devices such as the automated oscillometer and the traditional mercury sphygmomanometer, a study was carried out to compare the accuracy of the two devices as well as the best position to measure blood pressure. A comparative study regarding the difference in values of BP (mmHg) between traditional auscultatory method and automated oscillometric readings in supine and sitting positions was conducted among medical students. Oscillometer produced high readings than the readings of sphygmomanometer. Besides, the blood pressure readings for systolic and diastolic are higher while sitting when compared to supine position as the blood is unevenly distributed to all part of the body in sitting position. This will lead to the increase in ionotropic effect of the heart to pump blood towards the upper part of the body. The differences between two methods showed there have a major problem or error in measuring blood pressure. It is therefore necessary to improve the method and ways to check the health especially in this area where slight differences may contribute to large errors.
Keywords
Auscultatory Method; Arteries; Blood Pressure; Sphymomanometer; Socio-Demographic Variables; Supine and Sitting Position
Download this article as:| Copy the following to cite this article: Rizfan A. F, Ghosh K, Mustaqir A, Mona R, Firdous J, Muhamad N. Comparison Between Auscultatory and Oscillometric Reading of Blood Pressure Measurement While in Sitting and Supine Position. Biomed Pharmacol J 2019;12(2). |
| Copy the following to cite this URL: Rizfan A. F, Ghosh K, Mustaqir A, Mona R, Firdous J, Muhamad N. Comparison Between Auscultatory and Oscillometric Reading of Blood Pressure Measurement While in Sitting and Supine Position. Biomed Pharmacol J 2019;12(2). Available from: https://bit.ly/2RMhKQ4 |
Introduction
Increase in blood pressure is associated with the risk of coronary heart disease and developing numerous complications like renal impairment and visual impairment. Recently, there is a sharp rise in population having hypertension across the world. Accurate measurement of blood pressure is therefore important in the growing enigma of hypertensive disorders.1 Since blood pressure is the significant factor to detect the changes in human body and there has been two methods for arterial pressure measurement such as auscultatory method and oscillometric method. Both of the method has been widely used throughout the world and oscillometer is most commonly used in hospital due to its convenience and automatic measurement.2
Mercury products are being slowly phased out, making traditional sphygmomanometers obsolete. This creates the controversy regarding the accuracy of the automated oscillometric devices compared to the standard auscultatory mercury technique of measuring BP. Hearing Korotkoff sounds (K-sounds) to determine systolic and diastolic blood pressure (BP) was the most standard non-invasive method to acquire BP measurement for nearly 100 years.3 It is most widely used tool used in assessing patients with hypertension and risks of cardiovascular diseases. The oscillometric method usually cause an overestimation or underestimation.4 From the previous studies, it was observed the systolic measurements are higher while the diastolic measurements are lower using automated oscillometer. These values are compared to Korotkoff sound method where these sounds are produced between systole and diastole because the artery collapses completely and reopens with each heartbeat, producing a knocking sound which can be heard through the stethoscope. In most studies, automated oscillometer primarily overestimates diastolic BP.1 The mean diastolic BP was significantly greater using the auscultation/mercury technique than the automatic oscillometric technique.5
Correct blood pressure (BP) measurement is highly vital in the diagnosis of arterial hypertension (AH), and controversy exists whether supine BP should be treated as equal to sitting BP. Previous study indicated that the systolic and diastolic BP in the supine position was significantly higher than in the sitting position. Body mass index (BMI) and the measurement of BP (supine and sitting) seem to have significant impact on the pressure increment from a sitting to the supine position.6 Therefore, this study is to investigate the accuracy of both of the devices in the search of the most accurate way to measure blood pressure.
Materials and Method
A comparative study regarding the difference in values of BP (mmHg) between traditional auscultatory method and automated oscillometric readings in supine and sitting positions was conducted among male and female pre-clinical students of Universiti Kualalumpur Royal college of Medicine Perak (UniKL RCMP).
Sample Size
The population size is 195 and we are using openepi.com to estimate the sample size to get approximately 95% of confidence level for this population. In order to get the samples, simple random sampling method is chosen.
Study Variables
Study Variables are chosen as shown in Table 1.
Table 1: Study variables involved in the study.
| variable | Operational definition of variable |
| Gender | Male and female as respondents |
| Height | Respondents asked about their height |
| Weight | Respondents asked about their weight |
| BMI | Respondents about their BMI value |
| Systolic and diastolic blood pressure reading using oscillometer in sitting and supine position | Respondents blood pressure was measured |
| Systolic and diastolic blood pressure reading using sphymomanometer in sitting and supine position | Respondents blood pressure was measured |
Measuring Blood Pressure
Two consecutive observations of BP in a sitting position was recorded using mercury sphygmomanometer and oscillometer (OMRON Automated Blood Pressure Monitor MX3). Right upper-arm length and circumference determined the appropriate BP cuff used with the sphygmomanometer and was recorded in the sitting position. Then, two more consecutive observations of BP were followed by using a mercury sphygmomanometer and an oscillometer while in a supine position. This was done by the respondents when seated in a recliner chair at 45oC angle. Each subject was examined in a specific order, first two readings of BP using both the mercury sphygmomanometer and oscillometer in a seating position. This was followed by 3 mins of rest after that two more readings of BP using both the sphygmomanometer and oscillometer in a supine position was taken.2
Results
Blood pressure reading was gained through 152 respondents with age range between 18-30 years old. Out of the 152 respondents, the distribution according to gender was more towards male than female. There were 89 male participants (58.55%) and 63 female participants (41.42%). Besides, the number of respondent with the BMI range between 17- 22 were 99 respondents (65.13%), 23-29 were 41 respondents (26.97%) and 30-35 were 12 respondents (7.90%).
In comparing the relationship between sitting systolic BP (Y-axis) and supine systolic BP (X-axis) of oscillometric reading using positive linear graph, the mean average values of BP while sitting (122.84 mmHg) was higher compared to supine BP value (118.97 mmHg) for systole as shown in Fig. 1. The mean difference between the two positions was 3.87 mmHg. It was opposite in SD values where it was higher in supine (15.12) compare to sitting(12.55). High SD value indicates that the data points are spread out over a wider range of values. This shows the inconsistency of automated oscillometric readings since the values deviate more when compared to the sphygmomanometer.
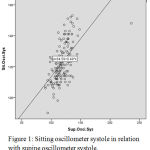 |
Figure 1: Sitting oscillometer systole in relation with supine oscillometer systole.
|
In comparing the relationship between sitting diastolic BP (Y-axis) and supine diastolic BP (X-axis) of oscillometric reading using positive linear graph, the mean average values of BP while sitting ((77.64 mmHg) was higher compared to supine BP value (77.64 mmHg) for diastole as shown in Fig. 2. The mean difference between the two positions for diastolic BP was 7.19 mmHg.
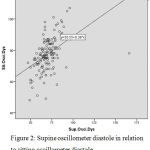 |
Figure 2: Supine oscillometer diastole in relation to sitting oscillometer diastole.
|
Relationship between sitting oscillometric systolic BP and sitting sphygmomanometer systolic BP was shown in Fig. 3. The graph shows a positive linear relationship between the value differences of the two variables. Systolic BP in sitting oscillometer had the tendency to have a greater value compared to the systolic BP sitting sphygmomanometer.
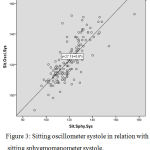 |
Figure 3: Sitting oscillometer systole in relation with sitting sphygmomanometer systole.
|
The below graph shows a relationship between supine oscillometric systolic BP and supine sphygmomanometer systolic BP with positive linear relationship between the value differences of the two variables. Systolic BP in supine oscillometer had the tendency to have a greater value compared to the systolic BP supine sphygmomanometer as shown in Fig. 4.
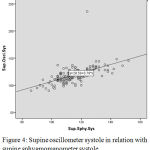 |
Figure 4: Supine oscillometer systole in relation with supine sphygmomanometer systole.
|
When comparing the relationship between supine sphygmomanometer systolic BP and sitting sphygmomanometer systolic BP, systolic BP in supine sphygmomanometer had the tendency to have a greater value compared to the sitting sphygmomanometer systolic BP as shown in Fig. 5.
 |
Figure 5: Sitting sphygmomanometer systole in relation with supine sphygmomanometer systole.
|
The relationship between supine sphygmomanometer diastolic BP and sitting sphygmomanometer diastolic BP was shown in Fig. 6. The graph shows a positive linear relationship between the value differences between the two variables where the diastolic BP in supine sphygmomanometer had the tendency to have a greater value compared to the sitting sphygmomanometer diastolic BP.
 |
Figure 6: Sitting sphygmomanometer diastole in relation with supine sphygmomanometer diastole.
|
Discussion
The mean systolic and diastolic blood pressure for oscillometric method was higher than the auscultatory method. In comparison to other studies, results from a study made by Johanna et al. showed that auscultatory method had a higher blood pressure reading than the oscillometric method.2 On the other hand, study by Mansoor et al. had similar results which indicates that automated oscillometer method of measuring BP had a higher blood pressure measurement compared to the auscultator method7. Furthermore, mean and median blood pressure measurement was significantly higher in sitting position than supine position. This may explain the mechanism of blood flow in our body as in supine position, blood is equally distributed to all parts of the body, maintaining a relatively lower pressure. On the other hand, in the sitting position, blood is not evenly distributed to all parts of the body, especially the upper torso. As the brain requires 15% of the cardiac output, the heart demonstrates a positive ionotropic effect resulting in higher blood pressure than supine position. This claim can be supported by a research done by Wei et al. that showed the sitting position had a higher systolic and diastolic blood pressure measurement.6 On the other hand, a study was discovered that systolic and diastolic blood pressure in supine position was statistically higher than in sitting position.8
An increase in pressure may induce myogenic response. The vasomotion of vessels can be affected by stress due to increased calcium level which in turn will increase pressure.9 This condition either induce or diminish vasomotion. Many vessels have this rhythmic diameter oscillation that can be caused by synchronous cytosolic calcium oscillations of smooth muscle cells.10 When smooth muscle cytosolic calcium contraction increase, pressure will modulate the vasomotion of vessels and causes arterial contraction. The obtained result was observed in blood pressure readings taken simultaneously using automated oscillometric technique in sitting and supine position. The measurement taken while in sitting position usually displays a higher blood pressure compared to supine positon.
The results obtained proves the median difference between sitting oscillometric systole and sitting sphygmomanometer systole was large. This shows the clinical significance of the huge fissure which can differentiate between a hypertensive and non-hypertensive diagnosis. This fissure can lead to a lifestyle change in diagnosed patients and therefore demands undoubted accuracy. The automated oscillometer (OMRON Automated Blood Pressure MX3) produces a digital readout where the blood when passes through artery between systolic and diastolic pressure causes vibrations. This vibration is transduced into electrical signals.11 The inconsistency of oscillometer usually relies on vibrations which can be easily disturbed by small movements as it needs ultimate stillness during the transfer of vibrations from the arterial wall to the transducer.12 Furthermore, the vibrations need to travel through the air inside the cuff, as opposing to the auscultatory method, in which the vibrations travel directly to the diaphragm of the stethoscope. This causes a marked difference as vibrations travel easier and faster in solid than in the loosely packed molecules of gas.
Auscultatory measurement of blood pressure yields a lower systolic and a higher diastolic value when compared to direct intra-arterial recording.13 The accuracy of the oscillometric method in measuring BP has been widely controversial and was not satisfactory and had a wider distribution of differences in mean values and inaccuracies in SBP14.This finding was consistent with our study, acquiring data which indicated sphygmomanometers having the lowest value when compared to oscillometers. These automated oscillometers had the tendency to overestimate mean SBP values by 2 mmHg when compared to the sphygmomanometers. Not only that, the position in which the SBP and DBP values were taken indicated that sitting had the tendency to have higher mean and median values when measured using the sphygmomanometers. These values were demonstrated in the experiment with mean difference value ranging from 4.68 mmHg to 6.06 mmHg.
Furthermore, when comparing mean difference between sitting sphygmomanometer systole and the supine sphygmomanometer and mean difference between sitting sphygmomanometer DBP and the supine sphygmomanometer DBP, had value ranging from 9.002-12.554 mmHg. This value is relatively lower when compared to values of the oscillometers ranging from 10.424 mmHg – 15.138 mmHg. This relatively lower and more consistent mean value of SBP and DBP acquired from the sphygmomanometer can be attributed to the higher and sharper frequency of the Korotkoff sounds which comes from the resonant motion of the arterial wall.15
The Korotkoff sounds has been used as an indirect way to measure BP for the last 100 years which was developed by Dr. Korotkoff. Natural resonance sounds originated from the concept of spring-mass-damper system provides a concise, yet rigorous, explanation for the origin of Korotkoff sounds and correlates with the classical Newtonian physics. This theory of idealized spring-mass-damper model almost always reproduces the time-domain waveforms which can be actually heard as the actual Korotkoff sounds heard by the human ear. The muffling of the sounds is explained by the increased resistance of the artery to collapse, caused by downstream venous engorgement. This study clearly suggests that why the Korotkoff sound is the most consistent and precise method of taking SBP and DBP which can be attributed to its reliability of reproducing transient resonances which is explained by the physics of wall of motion.16
The auscultatory/mercury technique is always associated with higher BP readings when compared to the automated oscillometer readings. Higher values for discrepancies or error occurs in older adult patients (>65 years old). The mean discrepancy or error between the two methods was estimated as 2 mmHg.2 But these values are of clinical importance as these values play a major role in determining the number of cardiovascular associated disease cases.17,18 Data from study done by Antonakoudis et al. indicated that even a mere reduction in blood pressure is associated with reduction of stroke and following a trend which favours fewer cardiovascular deaths. In conclusion, minute amounts of reduction in BP readings are of clinical significance, due to the fact that even with a discrepancy of 2 mmHg in present studies, can result in major case reductions associated with vascular events.19
Conclusion
There is significant difference in readings between auscultatory and oscillometric method. Besides that, this research also proves that different position such as sitting and supine position may affect the blood pressure measurement. These differences shows that we still have a major problem or error in measuring blood pressure. Improving the method and ways can rectify slight differences that may contribute to large errors.
Acknowledgements
The authors thank the management, UniKL RCMP for allowing this project. Authors are also thankful to the respondents who filled in the survey which helps to carry out this project.
References
- Shahbabu B, Dasgupta A, Sarkar K, Sahoo SK. Which is More Accurate in Measuring the Blood Pressure? A Digital or an Aneroid Sphygmomanometer. Journal of Clinical and Diagnostic Research : JCDR. 2016;10(3):LC11-LC4.
- Landgraf J, Wishner SH, Kloner RA. Comparison of automated oscillometric versus auscultatory blood pressure measurement. Am J Cardiol. 2010;106(3):386-8.
- Xiong L, Panicker GV, Im JJ. A study for the development of K-sound based automatic blood pressure device using PVDF film. Conf Proc IEEE Eng Med Biol Soc. 2016;2016:255-8.
- Kallioinen N, Hill A, Horswill MS, Ward HE, Watson MO. Sources of inaccuracy in the measurement of adult patients’ resting blood pressure in clinical settings: a systematic review. Journal of Hypertension. 2017;35(3).
- Acton QA. Hemodynamics: Advances in Research and Application: 2011 Edition: ScholarlyEditions; 2012.
- Wei TM, Lu LC, Ye XL, Li S, Wang LX. Difference in blood pressure between supine and sitting positions in diabetic and non-diabetic subjects. Med Sci Monit. 2009;15(3):Cr123-7.
- Mansoor K, Shahnawaz S, Rasool M, Chaudhry H, Ahuja G, Shahnawaz S. Automated Versus Manual Blood Pressure Measurement: A Randomized Crossover Trial in the Emergency Department of a Tertiary Care Hospital in Karachi, Pakistan: Are Third World Countries Ready for the Change? Open Access Macedonian Journal of Medical Sciences. 2016;4(3):404-9.
- Eser I, Khorshid L, Gunes UY, Demir Y. The effect of different body positions on blood pressure. J Clin Nurs. 2007;16(1):137-40.
- Koenigsberger M, Sauser R, Bény J-L, Meister J-J. Effects of Arterial Wall Stress on Vasomotion. Biophysical Journal. 2006;91(5):1663-74.
- Kapela A, Parikh J, Tsoukias Nikolaos M. Multiple Factors Influence Calcium Synchronization in Arterial Vasomotion. Biophysical Journal. 2012;102(2):211-20.
- Berger A. Oscillatory Blood Pressure Monitoring Devices. BMJ : British Medical Journal. 2001;323(7318):919.
- Izumizaki M, Tsuge M, Akai L, Proske U, Homma I. The illusion of changed position and movement from vibrating one arm is altered by vision or movement of the other arm. The Journal of Physiology. 2010;588(Pt 15):2789-800.
- Sahu D, Bhaskaran M. Palpatory Method of Measuring Diastolic Blood Pressure. Journal of Anaesthesiology, Clinical Pharmacology. 2010;26(4):528-30.
- Keavney B, Bird R, Caiazza A, Casadei B, Conway J. Measurement of blood pressure using the auscultatory and oscillometric methods in the same cuff deflation: validation and field trial of the A&D TM2421 monitor. J Hum Hypertens. 2000;14(9):573-9.
- Babbs CF. The origin of Korotkoff sounds and the accuracy of auscultatory blood pressure measurements. J Am Soc Hypertens. 2015;9(12):935-50.e3.
- Freedman DS, Foltz JL, Berenson GS. Differences Between the Fourth and Fifth Korotkoff Phases Among Children and Adolescents. American Journal of Hypertension. 2014;27(12):1495-502.
- Nasution, Khairuninnisa, Tanjung HR. Impacts of counselling on adherence to prescribed medications and blood pressure of hypertensive patients in four Indonesian primary health centers. International Journal of pharmacy and pharmaceutical sciences. 2015; 7(3): 114-117.
- Amal khalil turki, Syed Azar. Elevated blood pressure among patients with hypertension in general hospital of Penang , Malaysia. Does poor adherence matter? International Journal of pharmacy and pharmaceutical sciences. 2010;2(1): 24-32.
- Antonakoudis G, Poulimenos I, Kifnidis K, Zouras C, Antonakoudis H. Blood pressure control and cardiovascular risk reduction. Hippokratia. 2007;11(3):114-9.







