Manuscript accepted on :12-June-2019
Published online on: 28-06-2019
Plagiarism Check: Yes
Reviewed by: Mr. Guy-Armel Bounda
Second Review by: Renato Cuocolo
K. Rekha*1, Vaiyapuri Anandh2, D. Samuel Sundar Doss3 and A. Dinesh4
1Saveetha College of Physiotherapy, Saveetha University, India, Chennai, Chennai, India.
2Department of Physical Therapy, Applied Medical Sciences College, Majmaah University, KSA.
3Saveetha Medical College, Saveetha University, Chennai, India.
4Control and Automation Engineer.
Corresponding Author E-mail: futurdreams88@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/1702
Abstract
The Flutter is a medical handheld device, which is designed for patients suffering from various lung diseases. This device is designed to mobilize the excessive secretion of in the direction of airways and helps to loosen the mucus from the lungs and removed. Sometimes mucous in the lungs can become thick and hard to clear from the airways. If this mucous stays in the airways, it could block them, making it harder to breathe. Infection is also possible when mucous stays trapped in the airways. When one breathes out through the Flutter, it causes the ball inside to bounce. This bouncing causes increased pressure inside the chest and sends vibrations down through the airways. The combination of increased pressure and vibrations helps the mucous move from the lungs into the airways where it can be coughed out. Some patients cannot blow very forcefully, so our project is designed in such a way that the resistance of the blow is measured using a strain gauge. If the value goes below the certain threshold, limit the beep sound is heard and a light indication is provided so that we can find whether the patient should blow out even more faster. This device is small, portable, and easy to use and has no side effects.
Keywords
Audio Feedback; Arduino; Flutter Device; LCD; Siren; Visual Feedback
Download this article as:| Copy the following to cite this article: Rekha K, Anandh V, Doss D. S. S, Dinesh A. Biofeedback Flutter Device. Biomed Pharmacol J 2019;12(2). |
| Copy the following to cite this URL: Rekha K, Anandh V, Doss D. S. S, Dinesh A. Biofeedback Flutter Device. Biomed Pharmacol J 2019;12(2). Available from: https://bit.ly/2Yh2Cwk |
Introduction
Respiratory disorders are broadly classified into two major categories obstructive lung disease and restrictive lung disease. Obstructive lung diseases has an impact on expiration process. Chronic obstructive pulmonary disease (COPD) is a prevalent respiratory disease, which is a common cause of morbidity and mortality in developed and developing countries. Disease is characterised by chronic airflow limitation, which is not fully reversible, and it is progressive in nature with an abnormal inflammatory response of the lungs. Smoking is the major cause for COPD. Smoking affects the epithelial layers as it comprises of pseudo stratified columnar cells. The role of these ciliary cells is to act as defense mechanism.1 The most common pathophysiological feature of lung disease is impaired mucociliary transport and hypersecretion leading to mucus retention, atelectasis, pneumonia and decline in pulmonary function which significantly contributes to mortality and morbidity. Physiotherapy contributes in assessing and treating respiratory disorders mainly in airway clearance because mucus retention has huge impact on ventilator pump function, which increases the work of breathing and reduces the exercise tolerance. Further, it affects daily living activities and quality of life.2
Chronic obstructive pulmonary disease is chronic bronchitis and emphysema. Chronic bronchitis is a disease characterized by cough producing sputum for at least 3 months and two consecutive years. This disease is believed to be related to long-term irritation of tracheobronchial tree. The common cause for the disease is Cigarette smoke and other pollutants. These pollutants initially stimulate irritation in the trachea caused by the bacteria, virus, allergens, smoke, foreign bodies, cytokines and leukocytes which activates the goblet cells in the airways. Increased production of goblet cells produces more amount of sputum that declines the pulmonary functions.3
Emphysema is characterized by destruction of the respiratory bronchioles, edema, inflammation and thickened bronchiolar walls. It is associated with a prolonged history of smoking and chronic bronchitis and indicates significant irreversible lung damage. In addition, a less common type of emphysema not associated with smoking is alpha-antitrypsin deficiency. Antitrypsin deficiency reduces lung elasticity and contributes to characteristic increase in lung compliance, also includes irreversible alveolar damage resulting from loss of elastic recoil. Excessive distension and dilatation of the terminal bronchioles and destruction of the alveoli reduces the surface area for gas exchange.
Bronchiectasis is a respiratory pathway disease characterized by abnormal and permanent dilatation of the airways caused by perpetuation of inflammatory processes induced by frequent bacterial infections, which results in alteration in the ciliated epithelial lining and mucociliary damage producing thicker mucous. Destruction of the elastic and mucosal structures of the airway walls are evident with dilatation and fibrosis. The walls are lined with hyperplastic, nonciliated, mucus secreting cells that have replaced the normal ciliated epithelium this change is significant because it interrupts the mucociliary blanket and causes pooling of infected secretions, which further irritates and damages the bronchial wall.
Cystic Fibrosis is a critical genetic disorder, which mainly affects all the system in human being especially respiratory system, digestive system, liver, and pancreas. The indications of this disease are clubbing of nails and toes, gallstone, enlarged heart, trouble in digesting food and frequent lung infections. Cystic fibrosis patients may feel trouble to breath because of narrowing of the airway and one such defect is surplus of Na-Cl released through sweat. These irregularities are due to the abnormality in Na-Cl transport channel. CFTR is associated with the staging of sweat, digestive fluid and mucus and the main role of this regulator protein is to maintain the nature of the mucus in thin condition. The condition is diagnosed by sweat test and genetic testing. Earlier diagnostic methods such as titration procedure are used to diagnose cystic fibrosis and the drugs to treat or to cure cystic fibrosis is not available in our country. In India, knowledge on cystic fibrosis is less among the public. Lack of drugs and awareness among paediatricians is a big problem.4,5
Feedback Flutter Device
Besides medical treatment, physiotherapy plays an important role in treatment and various methods have been suggested to remove airway of secretions. The flutter is a simple and small medical device similar to whistle and be shaped like a pipe that creates a positive expiratory pressure (PEP) and high frequency oscillation when the expired air passes through it. These vibrations are thought to mobilize airway secretions facilitating their clearance and improving breathing.
Chronic obstructive pulmonary disease (COPD) is designated by airflow restriction, which is not fully reversible. This restriction is traditionally progressive and incorporated with an abnormal inflammatory response of the lungs to noxious particles or gases. Patients suffering from COPD may show pathologic converts not only in the large but also in the small airways, which are defined as less than 2mm in diameter. Airway inflammation may affect increased thick mucus secretions which can tiny the airways increasing the resistance to the airflow.
Flutter device is an oscillating PEP therapy and is automatically controlled; it provides similar frequency of oscillation within the range necessary to decrease the viscoelastic and spinnability properties of mucus. Flutter oscillates with a frequency most often between 6 – 26Hz, with an average PEP range of 5 – 19 Cm H2O, this oscillation frequency is higher than 0.3 – 0.4 Hz used in the in vitro experiments.6 In vitro studies, flutter device has showed its influence in varying expiratory pressures on the rheological properties of sputum and study demonstrated that the use of flutter device at different expiratory pressure is viable technique, which can be implemented, in clinical practice. Reviews have shown that flutter device does not have any difference in terms of sputum transportability during different expiratory pressures. Decreased sputum viscosity was reported for the pressure ranging between 15 cm to 25 cm H2O. Hence, from the evidences it is known that the patient need not generate a forced expiratory pressure to achieve the desired effect of sputum transportability. Because forced expiratory pressure increases the workload of the patient and patient becomes very tired rapidly. Hence it is suggested that flutter effectiveness could be compared by prolonging the treatment session, i.e. patient should perform slow and sustained expiration reducing the overload of respiratory muscles.
In recent years many equipment’s have been designed with biofeedback systems. Biofeedback system is the process that helps the person to become aware of their physiological functions using equipment’s that provides feedback on their performance. Respiratory training with biofeedback system facilitates the proper breathing pattern improves respiratory function, reduces respiratory rate and stress, improves gas exchange, improves ventilation and perfusion thereby decreases the activity of sympathetic nervous system by clearing secretions7. In literature survey, no studies were reported biofeedback systems in airway clearance device. Hence, this study aimed to introduce biofeedback system in flutter device as mucus clearance is the first step of respiratory rehabilitation. Pooling of secretions in the lungs has a major influence in mortality and morbidity. Conventionally flutter device does not provide any form of feedback to the patient. When the person performs expiration through the device, the steel ball inside the device oscillates to create vibrations over the chest wall. Obstructive lung disease is a problem with expiration and the major complication is secretions. Generally, participant does not receive any form of signal while performing expiration through the device. Therefore, this study is proposed to design an audio and visual feedback flutter device to provide feedback about their expiration and to motivate the treatment sessions. Hence, if the person is motivated to perform the device his performance in using the device will enhance. This will clear airways by mobilization of sputum and in turn reduce the episodes of dyspnoea. Therefore, the aim of the study is to design an audio-visual feedback flutter device.
Materials and Method
Flutter Device
Parts of Flutter Device
Flutter device is used to mobilize and eliminate mucus from the airways. The flutter device consists of four parts;
A mouth piece stem
A circular cone
A high density stainless steel ball
A protective cover
Working of Flutter Device
When the individuals perform an expiration through the flutter device, the steel ball inside the flutter device bounces and oscillates. These oscillations creates vibrations in the chest wall and that loosen mucus and also causes a slight increase in pressure that aids in keeping patient’s airways open. Mucus is then able to move up the airway which is coughed out and removed.
Instructions to use flutter device:
Relax and sit 90-degree position.
Place the device at particular angle on the mouth.
Fill lungs ¾ fully by inhaling.
Hold breath for 2 to 3 seconds
Exhale slowly, 100% fully.
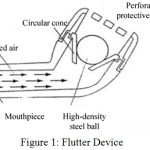 |
Figure 1: Flutter Device.
|
When using Flutter
Maximum oscillation can be achieved by moving the flutter slightly up or down.
The Patient should keep using it until no more mucus can be expectorated.18
Approximately 5 to 15 minutes can be taken to clear secretions.
Advantages of Flutter Device
Easy and safe to use.
Portable and relatively inexpensive and can be used on patient’s own.
Limitation of Flutter Device
Gravity dependent machine
Needs to be cleaned after every session
Can be used one patient only
Requires adequate cognitive function. E.g.: Motivation and Concentration
Requires adequate motor control that means sit in correct position, hold the device at the right angle and generate adequate expiratory pressure.
Proposed System
The proposed system consists of Arduino microcontroller, LCD, Siren and LED indicator. The screw gauge of the flutter device is connected to the Arduino microcontroller through the Mic, which converts an analog signal into digital signal. If the oscillation of the flutter device exceeds the threshold level, then the Arduino microcontroller sends a signal to the siren through a driver. Siren is used for the purpose of making noise to hear. Furthermore, the Arduino microcontroller sends the signal to the LED indicator, which blinks Red LED light for patient’s awareness and displays the oscillation and expiration time of the flutter device on the LCD display. Otherwise, the Green LED light blinks to indicate the device is in normal condition.
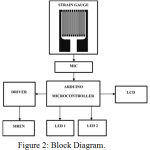 |
Figure 2: Block Diagram.
|
Hardware used
Microphone
Microphone is one of the transducer that converts sound waves into electrical waves. It changes analog information into digital information. The microphone is connected with the amplifier to produce large electrical signals. Without amplifier, the microphone produces only small amount of electrical signal. Because the Arduino board would not detect any meaningful signal. So the amplified signal from the output of an amplifier is able to detect large enough digital signal.
Arduino Microcontroller
Arduino microcontroller is the smart microcontroller unit that is programmed with Arduino software and there is no need to stalling other software for running Arduino programmes. It is an open source combination of both hardware and software. It is very flexible and easy to handle. It is also implemented for developers, designers and users for making useful things to the environments.
Arduino Uno is a board based on ATmega328 microcontroller. It has 14 digital input/output pins, six analogue inputs, a USB connection for programming the on-board microcontroller, power jack, an ICSP header and a reset button. It is operated with the help of 16 MHz crystal oscillator. It contains needed information for supporting microcontroller.
The Arduino board is very easy to operate while connect to the computer with USB cable or power adapter or battery. By using Arduino development environment (ADE), the microcontroller is programmed with the help of Arduino programming language.
LCD Display
LCD or Liquid Crystal Display works on the principle of light modulating properties and polarization property. The light modulating properties used for liquid light and polarization property used for the operation of the light. LCD only blocks the light instead of emitting light.
The Liquid Crystal Display displays value of oscillation in Hz and consumption time in sec.
The 16×2 LCD display has a total of 16 pins. Pin 7-14 are data lines, Pin 1, Pin 16 are for power and ground. Pin 4-6 are used to control the operation of LCD. Pin 3 is used to adjust the screen brightness of the LCD. The remaining Pin 15, 16 are used to power the back light.
 |
Figure 3: LCD Display.
|
Siren
Siren or buzzer is an audio signalling device. A piezo buzzer looks like a very small element similar to a capacitor. It needs a push-pull driver circuit to charge and discharge the capacitance of the piezo. However, a piezo will work quite well with a small modification with 1k Ohm resistor placed across the piezo buzzer to discharge its capacitance. The piezo buzzer requires a little drive circuit to get good sound level without any interruption.
If the oscillation of the flutter device extends the threshold frequency, the Arduino microcontroller exports signal to the siren through the driver. This will make a loud to noise to hear up to 60 decibel.
LED
LED is a semiconductor device that allows current flow in one direction. It emits light instead of blocking a light when forward voltage is applied in PN junction. The green and red LED is used in this proposed system. When the oscillation level is in uniform frequency, the Arduino microcontroller sends signal to the green LED to glow. Otherwise, Arduino operates the Red LED.
Software used
Proteus 8 Simulator
Proteus 8 is one of the best simulation software for various circuit designs of microcontroller. It has almost all microcontrollers and electronic components readily available in it and hence it is widely used simulator. It can be used to test programs and embedded designs for electronics before actual hardware testing. The simulation of programming of microcontroller can also be done in Proteus. Simulation avoids the risk of damaging hardware due to wrong design.
AVR Studio Version 4
It is used to write, build, compile and debug the embedded c program codes, which are needed to be burned in the microcontroller in order to perform desired operations. This software directly provides .hex file, which can be easily burned into the microcontroller.
Results
Frequency and Expiration Time Reading in the Flutter Device
The flutter device was connected with a microphone so that as the patient performs expiration through the device the signal is channelized through microcontroller and reaches the Liquid Crystal Display (LCD) displays value of oscillation of the steel ball in Hz and Expiration time in seconds. With the help of the software Proteus 8 Simulator and AVR Studio Version 4 the performance results of frequency and expiration time are stored in the Laptop for statistical analysis.
Discussion
Flutter device is known to be a good airway clearance equipment. Airway clearance is the first line of management for all respiratory disorders, hence airway clearance need more attention for this reason the study proposed to design the biofeedback systems for the flutter device. Biofeedback system is known to be a feedback provided auditory, visually or audio-visually. Therefore, in this study biofeedback system was enhanced using the simple methods of LED light and a buzzer.
The designed biofeedback systems were used for the respiratory disease individuals along with flutter device and the outcomes were tested. The working of the biofeedback system was ensured with the LED light and buzzer sound. Individual capacity of blowing through the flutter device was determined with the help of frequency outcome. When the person perform the expiration properly at the required range the feedback will be enhance that encourages the patient to perform the device well. And the display also reads the expiration time. How many seconds a person takes for the expiration could also be noted as most of the obstructive lung disease individuals have difficulty in performing expiration. When the expiration is encouraged the ball in the flutter device oscillates and creates vibration in the chest wall and simultaneously feedback of a buzzer or light will be enhanced to encourage the person. Prolonged expiration helps to improve collateral ventilation and prevents airway collapse mobilizes the sputum.
Conclusion
The biofeedback system was designed in a way that the circuit is easily detachable. So that the flutter device alone was sterilized after every use. The preferred method of sterilization was gas sterilization in the hospital sterilization unit. Where the device was sterilized and tested in the microbiology department following every use and ensured that there was no infection or growth of any microorganisms and there was no toxic agents reported after sterilization procedure. The device was ready to use after every sterilization. The flutter was reattached to the feedback circuit after every use. Therefore, the study ensured the quality in using the equipment and maintain the hygiene. Hence, the device is recommended for the use among individuals with these sterilization procedures in order to prevent infections and promote bronchial hygiene.
Conflict of Interest
There is no conflict of interest.
References
- Thorley A. J., Tetley T. D. Pulmonary epithelium, cigarette smoke and chronic obstructive pulmonary disease. International Journal of Chronic Obstructive Pulmonary Disease. 2007; 2(4), 409–428.
- Gosselink R. Physical therapy in adults with respiratory disorders: where are we? RevistaBrasileira de Fisioterapia. 2006; 10(4).
- Bhowmik A, Chahal K, Austin G, Chakravorty I. Improving mucociliary clearance in chronic obstructive pulmonary disease. Respiratory Medicine. 2009; 103(4): 496–502.
- Lester, Mary K.Nebulizer. Use and maintenance by cystic fibrosis patients: a survey study. Respiratory: 2004; 49(12): 1504-1508.
- Gondor M, Nixon PA, Mutich R, Rebovich P, Orenstein DM. Comparison of flutter device and chest physical therapy in the treatment of cystic fibrosis pulmonary exacerbation. Pediatr Pulmonol. 1999; 28: 255-260.
- McIlwaine M., Bradley J., Elborn J. S., Moran F. Personalising airway clearance in chronic lung disease. European Respiratory Review. 2017; 26: 143.
- Zhu Q., Zheng F. Respiratory training biofeedback system. 2011; 3915–3918.
- Shak S, Capon DJ, Hellmiss R, Marsters SA, Baker CL. Recombinant human dnase reduces the viscosity of cystic fibrosis sputum. Proc Natl Acad Sci USA. 1990; 87: 9188-92.
- Hubbard RC, McElavaney NG, Birrer P, Shak S, Robinson WW, Jolley C . A preliminary study of aerosolized recombinant human deoxyribonuclease in the treatment of cystic fibrosis. N Eng J Med. 1992; 326:812-5.
- Aiken ML, Burke W, McDonald G, Shak S, Montgomery AB, Smith A. Recombinant human dnase inhalation in normal subjects and patients with cystic fibrosis. JAMA. 1992; 267(14): 1947-51.
- Joan, CD, Patricia, JO. Physiologic evidence for the efficacy of positive expiratory pressure as an airway clearance technique in patients with cystic fibrosis. Journal of the American Physical Therapy Association. 2004; 84 (3): 524-537.
- Milic – Emili J, Henderson JAM, Dolovich MB. Regional distribution of inspired gas in the lung. Journal of the American Physical Therapy Association. 1966; 21: 749-759.
- Volsko TA, Difiore J, Chatburn RL. Performance comparison of two oscillating positive expiratory pressure devices: Acapella versus Flutter. Respir Care. 2003; 48: 124-130.
- Kluft J, Baker L, Castagnino M, Gaiser J, Chaney H, Fink RJ. A comparison of bronchial drainage treatments in cystic fibrosis. Pediatr Pulmonol. 1996; 22: 271-274.
- Basoglu OK, Atasever A, Bacakoglu F. The efficacy of incentive spirometry in patients with COPD. Respirology. 2005; 10: 349–353.
- American Association for Respiratory Care. Clinical practice guideline: Use of positive airway pressure adjuncts to bronchial hygiene therapy. Respir Care. 1993; 38: 516-521.
- Gondor M, Nixon PA, Mutich R, Rebovich P, Orenstein DM. Comparison of flutter device and chest physical therapy in the treatment of cystic fibrosis pulmonary exacerbation. Pediatr Pulmonol. 1999; 28: 255-260.
- Homnick DN, Anderson K, Marks JH. Comparison of the flutter device to standard chest physiotherapy in hospitalized patients with cystic fibrosis: a pilot study. Chest. 1998; 114: 993-997.







