Manuscript accepted on :28 April 2018
Published online on: 09-05-2018
Plagiarism Check: Yes
Zahraa Abdulaali Jlekh and Zainab M. Abdul-Ameer
Department of Conservative and Cosmetic Dentistry, College of Dentistry, University of Baghdad, Baghdad, Iraq.
Corresponding Authors E-mail: dr.alkarkhi@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/1429
Abstract
This in vitro study aimed to assess and compare premolars cuspal deflection that restored with different bulk fill resin materials types (SonicFillTM2, Beautifil Bulk Fill restorative, and FiltekTM Bulk Fill posterior restorative) to those incrementally restored group with conventional composite restorations (low shrinkage universal Tetric Evoceram). A total of 40 intact human maxillary first premolars were prepared into large MOD. Then teeth were randomly classified into four groups (n=10 for each group) according to restorative materials as following: Group A: Teeth were restored with Sonic FillTM2 composite, Group B: restored with Beautifil Bulk Fill restorative material, Group C: Teeth were restored with Filtek BulkTM Fill posterior restorative, and Group D: Teeth were restored with Universal Tetric Evo Ceram®. Digital microscope was used to measure intercuspal distance between two index reference points on the tips of the cusps before preparation, after preparation, and 15minutes after completion of restorations. The differences registered as cuspal deflection. All teeth were exposed to inward cuspal deflection after restoration and all groups that restored with bulk fill restoration reported lower cuspal deflection in compared to group D that restored with conventional composite in layering technique. Beautifil Bulk Fill restorative produced significantly greater cuspal deflection than other bulk fill groups. The study concluded that the use of new bulk fill restorative materials might reduce amount of cuspal deflection significantly. However, type of bulk fill restorative materials also influenced on amount of cuspal deflection so restoration with Sonic Fill™2 composite and Filtek Bulk™ Fill posterior reported lower cuspal deflection than Beautifil Bulk Fill restorative material.
Keywords
Beautifil Bulk Fill Restorative Material; Bulk Fill; Cuspal Deflection; Filtek BulkTM Fill Posterior Restorative; Intercuspal Distance Sonic FillTM2 Composite;
Download this article as:| Copy the following to cite this article: Jlekh Z. A, Abdul-Ameer Z. M. Evaluation of the Cuspal Deflection of Premolars Restored with Different Types of Bulk Fill Composite Restoration. Biomed Pharmacol J 2018;11(2). |
| Copy the following to cite this URL: Jlekh Z. A, Abdul-Ameer Z. M. Evaluation of the Cuspal Deflection of Premolars Restored with Different Types of Bulk Fill Composite Restoration. Biomed Pharmacol J 2018;11(2). Available from: http://biomedpharmajournal.org/?p=20381 |
Introduction
The composite resin materials have been widely used as a direct posterior restoration due to increase patients’ demands to tooth color restoration and environment-friendly nature of composites.1 Nevertheless, the polymerization shrinkage or bulk contraction that induced by densification of resin matrix through polymerization process is represented as a major drawback for using direct composite resins,1,2
Polymerization shrinkage stress is associated with two clinical problems (microleakage and cuspal deflection) depending on the bond strength; microleakage results from that the bond strength of the adhesive system is lower than polymerization shrinkage stress, which may lead to composite-tooth interface failure and marginal gap formation. Consequently, this may cause secondary caries and sensitivity after restoration, while cuspal deflection occurs when the adhesion bond strength is enough to resist polymerization shrinkage stresses. Therefore, no detachment arises, however the internal stress of restoration will reduce the intercuspal distance by pulling cusps together.1,3-7
Cuspal deflection may cause enamel cracks, tooth fracture and sense clinically by the patient as postoperative sensitivity and pain.8
Two main groups of biomechanical factors are affecting on amount and type of cuspal deflection, the geometrical factors (include cavity dimension and thickness of cavity walls after preparation) and material properties (polymerization shrinkage, elastic modulus, flow and hygroscopic expansion of composite material), which represent the first group. while the second group is described as clinical factors and included placement technique, direct or indirect restoration, using stress absorbing layers with low elastic modulus liners, and light curing unit and protocol.9,10
Incremental layering technique was suggested as a golden standard technique for placement of resin composites in large cavities due to its ability to reduce the consequences of shrinkage stress and allow adequate degree of conversion.11
New types of restorative materials called bulk fill restorative materials have been introduced to reduce time required for placement. These materials can be placed in bulk layer up to 4-5mm with adequate polymerization and low polymerization shrinkage stress.12
However, little information is available regarding the effect of these restorative materials on cuspal deflection. So that this study aimed to assess cuspal deflection of upper first premolars restored with newly developed types of bulk fill restorative materials and compare them with conventional composite placed in oblique incremental layers technique.
The null hypothesis of the study that there are no differences in amount of premolars cuspal deflection between bulk fill restorations with bulk fill resins based materials
Materials and Methods
Forty intact, non- carious human maxillary first premolar teeth were collected for this study. All teeth extracted for orthodontic causes and immediately stored in distilled water. The teeth were cleaned carefully for any calculus deposits with air scalar and polished pumice. All selected teeth had nearly similar crown shape and size, uniform occlusal anatomy and cracks free on visual examination by using magnifying lens and by transilluminating from LCU. Maximum deviation for bucco-palatal width (BPW) of the premolars was not more than 10% from determined mean.
Each tooth was marked 2±0.5 mm above the CEJ with an indelible pen. Then roots of each tooth were mounted with vertical long axis by aiding of surveyor into customized silicon mold filled with cold cure acrylic (Vertex, Netherland). Two heads of pins (reference points) were bonded with single bond universal (3M ESPE,) into indentation prepared on the tips of the cusps (Buccal and palatal) of each tooth by small carbide round bur (comet, Germany).
Large MOD cavity with parallel walls was prepared in each tooth by using a flat-ended diamond fissure bur (Microdent, China) with parallel sided in a high-speed hand piece with coolant water. The movement of hand piece was restricted by using a modified dental surveyor to ensure standardization of cavity in all preparation, burs were replaced every four preparations to ensure high cutting efficiency.
The dimension of cavity was standardized 3mm width at the pulpal floor and gingival seats of the boxes, 3mm depth at the occlusal isthmus that measured from the cavo-surface margin of palatal wall to pulpal floor, and gingival seat of box with 1mm axial walls depth and height as in Figure.1 The cavo-surface margins of the cavity were prepared at 90° and rounded internal line angle of the cavity.
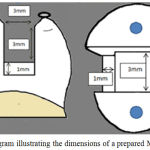 |
Figure 1: Diagram illustrating the dimensions of a prepared MOD cavity
|
All materials used in this study are labeled in Table (1). Materials were used according to manufacturer’s recommendations.
In all prepared tooth, single bond universal (3M ESPE, USA) was used in etch and rinse mode according to manufacturer’s recommendations. Then divided into four groups according to type of restoration
Group A: after placement transparent plastic SuperMat® band, teeth were restored with Sonic FillTM2 composite (Kerr Corporation, USA). According to manufacturer’s, The Sonic FillTM handpiece was turn through foot pedal to activate the sonic vibration, which changed the viscosity of the Sonic FillTM2 composite material from high viscosity to low viscosity, then the cavity was filled in one increment (bulk) and cured with LED light cure unit (power intensity of 800mw/cm2) for 20 seconds.
Additionally, the restoration was cured for 20 seconds from the lingual and buccal after removal of the SuperMat® matrix band.
Group B: Teeth were restored with Beautifil Bulk Fill restorative material according to manufacturer’s recommendations. It placed in one increment (bulk) and cured as in Group A.
Group C: Teeth were restored with Filtek Bulk Fill posterior restorative in bulk increment and cured as in Groups A and B.
Group D: Teeth were restored with Universal Tetric Evo Ceram® in eight triangular increments of approximately 2-mm thickness, three wedge shape layers for each box and the occlusal surface was restored with two layers. Each increment was cured for 20 second according to manufacturer’s instruction.
Dino-lite digital microscope (AnMo Electronics Corporation, Taiwan) was used to precisely measure the intercuspal distance (distance between two references points) of sample in micrometer (µm).
Intercuspal distance was measured for unaltered tooth, after tooth preparation, and 15minuntes after tooth restoration. The cuspal deflection after cavity preparation (CD1) was measured by subtracting the intercuspal distance after cavity preparation from intercuspal distance for unaltered teeth. The ICD after preparation was recorded as initial distance while ICD after 15 minutes was recorded as final distance.13Then the cuspal deflection that occurred as a result of polymerization shrinkage stress (CD2) was measured by subtracting final distance from initial distance.
Table 1: manufacturers information of materials used in this study
| products | Manufacturers | Description | Main composition | Fillers loading |
| Beautifil Bulk (universal)
LOT: 051617 |
SHOFU, Japan | Giomer nano-hybrid bulk fill | Matrix: Bis-MPEPP, UDMA, Bis-GMA, ,TEGDMA
Fillers: S-PRG fillers |
87% wt., 74.5% vol. |
| FiltekTM Bulk Fill Posterior Restorative (A2)
LOT: N840827 |
3M ESPE, St. Paul, USA | Nano-filled bulk fill composite | Matrix: Aromatic UDMA, UDMA, AFM, 1, 12-DDMA
Fillers: aggregated zirconia/silica cluster filler, ytterbium trifluoride filler, non-agglomerated/non-aggregated silica filler, non-agglomerated/nonaggregated zirconia filler. |
76.5 %wt., 58.5% vol. |
| SonicFill™2
(A2) LOT: 6173799 |
Kerr Corporation,
Orange, CA, USA |
Sonically activated nano-hybrid bulk fill composite | Matrix: Bis-GMA , Bis-EMA
Fillers: new filler system containing nano-scale zirconium oxide and silica oxide particles |
81.3% wt., unreported%vol. |
| Universal Tetric EvoCeram®
(A2) LOT: U56297 |
Ivoclar Vivadent, Liechtenstein | Conventional nano-hybrid composite | Matrix: Bis-GMA, Bis- EMA and UDMA.
Fillers: Barium glass, ytterbium- trifluride, mixed oxide and Prepolymer |
75-76% wt., 53-55%Vol. |
| Single Bond Universal
LOT: 65520 |
3M ESPE, Germany | Single-component universal | Bis-GMA, HEMA, VitrebondTM copolymer, filler, ethanol, water, initiators, silane | 10% wt. |
Bis-GMA, bisphenol A diglycidyl ether dimethacrylate; UDMA, urethane dimethacrylate; Bis-MPEPP, bisphenol A polyethoxy-dimethacrylat; TEGDMA, triethylene glycol dimethacrylate; AFM, Addition-fragmentation monomers; DDMA, dodecanediol dimethacrylate; Bis-EMA, bisphenol A ethoxylated methacrylate; HEMA, 2-hydroxyethyl methacrylate.
Results
The descriptive statistics for inward cuspal deflection CD1and CD2 in micrometer are summarized in Table 2. There was non-significant differences among all groups after cavity preparation (CD1) (one-way ANOVA P<0.01).While there was significant difference among all groups after 15minutes from complete restoration (P=0.000).
Table 2: The descriptive statistics for inward cuspal deflection CD1and CD2 in micrometer (µm)
| CD1 | CD2 | ||||
| groups | n | Mean | ±SD | Mean | ±SD |
| A | 10 | 4.6482 | 1.170515 | 5.9415 | 0.54315 |
| B | 10 | 3.8571 | 0.974685 | 7.0677 | 1.263111 |
| C | 10 | 4.3821 | 1.273434 | 5.7807 | 1.198434 |
| D | 10 | 4.3185 | 1.08428 | 9.4749 | 1.441092 |
| P-value | 0.478 | 0.000 | |||
Discussion
Cuspal deflection was regarded as one of common complication that occur as a result of the polymerization stress of resin-based composites on tooth structure and can act as a preloading that facilitate fracture of the tooth under tension and may represent the main cause of failure through composite curing.14,15
Extracted teeth have been broadly used in cuspal deflection measurement because they eliminated the problem of the compliance of the testing system and supporting structures.16 Maxillary first premolar teeth were used in this study because these teeth are uniform in size and shape.17
Large MOD cavity was prepared in the present study to weaken the remaining tooth structure, increase C-factor, and result in a 63% loss in relative cuspal stiffness; consequently, it increases compliance of the cusp for favor possible deflection and gives imitation of clinical state.18-20 In addition, the polymerization shrinkage force of composite can cause less negative cuspal deflection in MO or DO versus MOD restorations because they need small amount of filling material.3,21-23
The distances between two reference points were measured after 15 minutes from completing restoration because the cuspal deflection was much slower and longer than polymerization shrinkage of the composites and several studies reported that the maximum amount of inward displacement is occurred through this time and the specimens were totally hydrated.24-26This might attributed to the remaining free radicals. Double bonds in resin base restoration persisted to react. Therefore, the deformation was continued for several minutes after complete polymerization procedure.27,28
From the results of current study it’s obvious that no significant differences among all experimental groups when displacement is measured after cavity preparation. These results are accordance with other studies, reported that the teeth were exposed to deformation after cavity preparation but this deflection was not statically significant among all groups because they had performed by same operator and prepared by standardized method.
The result of this study showed cuspal deflection (an inward deflection) for all groups after completing restorative procedure. This result is in agreement with other studies, concluded that the polymerization shrinkage stress development after polymerization process caused an inward cuspal deflection.13,18,21,26,30-33
The null hypothesis was rejected because the mean value of cuspal displacement for premolars restored with conventional composite in oblique layering technique is significantly greater than mean value of groups restored with bulk fill restorative material. This result is in agreement with other studies, found that the bulk fill composite resin materials caused less cuspal deflection than conventional composite.12,17,32-37
This reduction may attribute to that the new bulk fill resin-based materials are induced lower shrinkage stress than those of a conventional composite through incorporation of stress-relievers to change the shrinkage dynamics , using novel chemistry, increase filler loading with decrease resin matrix, and consequently, reduce polymerization shrinkage stress.33,35,37
On other hand, this result is in disagreement with other studies, found that the bulk fill resin-based composites do not differ from conventional composites in the shrinkage stress, integrity of the margin, cuspal flexure and can be sufficiently cured at 4mm depth.29,38
Group C (restored with Filtek™ Bulk Fill Posterior Restorative) show lowest mean value of cuspal deflection after restoration, this may be due to eliminate the monomer TEGDMA (286 g/mol) from its resin system. In addition, Filtek Bulk Fill has two innovated monomers, which play important role in reducing shrinkage stress as AUDMA and AFM. AFM has addition fragmentation chain-transfer capability, the advantage of addition fragmentation chain-transfer is that makes the covalent network capable of adapting to stress generation via bond breakage and reformation, without net loss of crosslinking via an allyl disulfide bond.39,40
In this study, group A (restored with Sonic FillTM2) and group C (restored with FiltekTM Bulk Fill posterior restorative) showed lower mean cuspal deflection, but no statistically significant difference between them. According to the manufacturers, SonicFill2 and FiltekTM Bulk Fill Posterior resin-based composites have innovated monomers and mechanism respectively, which reduce shrinkage stress. Sonic FillTM2 contains rheological modifiers, which react with sonic energy to allow for dropping in viscosity and increasing particle motion upon activation with a designated handpiece, leading to increased pre-gel stress-relief via internal flow and consequently, leading to lower cuspal deflection.37
Group B (restored with Beautifil Bulk Fill) show higher cuspal deflection than other bulk fill types used in this study, this may due to present polymerization modulators with high molecular weight in other bulk fill composites materials tested in this study, which reduce polymerization shrinkage by delaying gel point, and giving additional time to recompense of the shrinkage.41
Conclusion
The conventional composite resin that placed incrementally resulted in greater cuspal deflection compared to bulk fill resins-based material. Cuspal deflection magnitude in bulk fill resins-based material depends on type of filling materials.
Conflict of Interest
There is no conflict of interest.
References
- Karaman E and Ozgunaltay G. Cuspal deflection in premolar teeth restored using current composite resins with and without resin-modified glass ionomer liner. Operative dentistry. 2013;38( 3):282-89.
- Loguercio, Alessandro Dourado, et al. Polymerization shrinkage: effects of boundary conditions and filling technique of resin composite restorations. Journal of dentistry. 2004;32(6):459-70.
CrossRef - Suliman A.A, Boyer D.B, Lakes R.S. Interferometric measurements of cusp deformation of teeth restored with composites. Journal of dental research. 1993;72(1):1532-36.
- Gonzalez-Lopez S, et al. Influence of different composite restoration techniques on cuspal deflection: an in vitro study. Operative dentistry. 2004;29(6):656-60.
- Tantbirojn, Daranee, et al. Tooth deformation patterns in molars after composite restoration. Dental materials. 2004;20( 6):535-42.
- Kim M.E and Park S.H. Comparison of premolar cuspal deflection in bulk or in incremental composite restoration methods. Operative dentistry. 2011;36(3):326-34.
CrossRef - Jafarpour S, et al. Effect of composite insertion technique on cuspal deflection using an in vitro simulation model. Operative dentistry. 2012;37(3):305-299.
CrossRef - Bausch J. Robert et al. Clinical significance of polymerization shrinkage of composite resins. The Journal of prosthetic dentistry. 1982;48(1):59-67.
CrossRef - Lee, Mi-Ra, et al. Influence of cavity dimension and restoration methods on the cusp deflection of premolars in composite restoration. Dental materials. 2007;23(3):95-288.
- Oskoee, Siavash Savadi, et al. The effect of composite fiber insertion along with low-shrinking composite resin on cuspal deflection of root-filled maxillary premolars. The journal of contemporary dental practice. 2012;13(5):595-01.
CrossRef - Park Junkyu, et al. How should composite be layered to reduce shrinkage stress: incremental or bulk filling?.Dental materials. 2008;24(11):1501-05.
CrossRef - El-Damanhoury H.M, and Platt J.A. Polymerization shrinkage stress kinetics and related properties of bulk-fill resin composites. Operative dentistry. 2014;39(4):374-82.
CrossRef - Campos Edson Alves, et al. Cuspal movement related to different bonding techniques using etch-and-rinse and self-etch adhesive systems. European Journal of Dentistry. 2009;3(3):213-18.
- Versluis, Antheunis, et al. Can hygroscopic expansion compensate polymerization shrinkage? Part I. Deformation of restored teeth. Dental materials. 2011;27(2):126-33.
CrossRef - Kwon, Youngchul, Jack Ferracane and In-Bog Lee. Effect of layering methods, composite type, and flowable liner on the polymerization shrinkage stress of light cured composites. Dental materials. 2012;28( 7):801-09.
- Sultan, Ahmed, Advan Moorthy, and Garry Fleming J.P. The adhesive potential of dentin bonding systems assessed using cuspal deflection measurements and cervical microleakage scores. Dental material. 2014;30(1):1154-60.
CrossRef - McHugh, Lauren E. J, et al. mImplications of resin-based composite (RBC) restoration on cuspal deflection and microleakage score in molar teeth: Placement protocol and restorative material. Dental materials. 2017;33(9): e329-e35.
- Abbas G, et al. Cuspal movement and microleakage in premolar teeth restored with a packable composite cured in bulk or in increments. Journal of dentistry. 2003;31(6):437-44.
- Fleming G. J . P, et al. Cuspal movement and microleakage in premolar teeth restored with resin-based filling materials cured using a ‘soft-start’ polymerisation protocol. Dental materials. 2007;23(5):637-43.
CrossRef - El-Helali, Ruaa, et al. Influence of resin-based composite restoration technique and endodontic access on cuspal deflection and cervical microleakage scores. Journal of dentistry. 2013;41(3):216-22.
- Palin, William M, et al . In vitro cuspal deflection and microleakage of maxillary premolars restored with novel low-shrink dental composites. Dental materials. 2005;21(4):324-35.
CrossRef - González-López S, et a . Effect of restorative procedures and occlusal loading on cuspal deflection. Operative dentistry. 2006;31(1):33-38.
CrossRef - Behery, Haytham, et al. Cuspal Deflection of Premolars Restored with Bulk-Fill Composite Resins. Journal of Esthetic and Restorative Dentistry. 2016;28(2):122-30.
CrossRef - McCullock A. J , and B. G. Smith. In vitro studies of cuspal movement produced by adhesive restorative materials. British dental journal. 1986;161(1):405-09.
- Lopez, Santiago Gonzalez, et al. Influence of cavity type and size of composite restorations on cuspal flexure. Medicina oral, patología oraly cirugía bucal. Ed. inglesa. 2006;11(6) 536-40.
- Singhal S, Gurtu A, Singhal A, Bansal R, Mohan S. Effect of Different Composite Restorations on the Cuspal Deflection of Premolars Restored with Different Insertion Techniques-An In vitro Study. Journal of Clinical and Diagnostic Research. 2006;11(8):ZC67-ZC70.
- Ratih Diatri N, Joseph E, Palamara A and Harold H. Messer. Dentinal fluid flow and cuspal displacement in response to resin composite restorative procedures. dental materials. 2007;23(11):1405-11.
CrossRef - Blažić, Larisa, et al . Modulated photoactivation of composite restoration: measurement of cuspal movement using holographic interferometry. Lasers in medical science. 2011;26(2):179-86.
CrossRef - Güler, Eda and Emel Karaman. Cuspal deflection and microleakage in premolar teeth restored with bulk-fill resin-based composites. Journal of Adhesion Science and Technology. 2014;28(20):2089-99.
CrossRef - Suliman A. A, Boyer D. B and Lakes R. S. Cusp movement in premolars resulting from composite polymerization shrinkage. dental materials. 1993;9(1):6-10.
CrossRef - Alomari Q. D, Reinhardt J. W and Boyera D. B. Effect of liners on cusp deflection and gap formation in composite restorations. Operative Dentistry. 2001;26(4):406-11.
- Moorthy , A, et al. Cuspal deflection and microleakage in premolar teeth restored with bulk-fill flowable resin-based composite base materials. Journal of dentistry. 2012;40(6):500-05.
CrossRef - Elsharkasi M. M, et al. Cuspal Deflection in Premolar Teeth Restored with Bulk-Fill Resin-Based Composite Materials. Operative Dentistry. 2018;43(1):E1-E9.
- Francis A. V, et al. Cuspal Flexure and Extent of Cure of a Bulk-fill Flowable Base Composite. Operative Dentistry. 2015;40(5):515-23.
CrossRef - Rosatto C. M. P., et al. Mechanical properties, shrinkage stress, cuspal strain and fracture resistance of molars restored with bulk-fill composites and incremental filling technique. Journal of dentistry. 2015;43(12):1519-28.
CrossRef - Tomaszewska Iwona M., et al. Bulk fill restoratives: To cap or not to cap–That is the question?. Journal of dentistry. 2015;43(3):309-16.
CrossRef - Ólafsson, Vilhelm G., et al. Effect of composite type and placement technique on cuspal strain. Journal of Esthetic and Restorative Dentistry. 2017.
- Do, Thuydung, et al. Cuspal flexure, depth-of-cure, and bond integrity of bulk-fill composites. Pediatric dentistry. 2014;36(7):468-73.
- Park, Hee Young, et al. Novel dental restorative materials having low polymerization shrinkage stress via stress relaxation by addition-fragmentation chain transfer. Dental Materials. 2012;28(11):1113-19.
CrossRef - Fugolin A.P.P and Pfeifer C.S. New Resins for Dental Composites. Journal of dental research. 2017;9(10):1085-91.
- Tsujimoto, Akimasa, et al. Depth of cure, flexural properties and volumetric shrinkage of low and high viscosity bulk-fill giomers and resin composites. Dental materials journal. 2017;36(2 ):205-13.







