Samaneh Rashidi1, Ali Yadollahpour1* and Maryam Mirzaiyan2
1Department of Medical Physics, School of Medicine, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran. 2BS Student of Anaesthesia, School of Medicine, Esfahan University of Medical Sciences, Isfahan, Iran.
DOI : https://dx.doi.org/10.13005/bpj/866
Abstract
During the recent years several non-pharmaceutical treatments have been proposed as alternative or adjunctive treatment for chronic wounds. Low level laser therapy (LLLT) is a new technique used for the treatment of wounds. The present study reviews the most current laser radiation based methods for wound treatments and clinical considerations for the different wounds. In addition, the proposed mechanisms of action of LLLT associated with wound healing processes are briefly discussed. Several studies have been conducted to gain better understanding of the healing process of laser, however; to better clarification of various stages of healing procedure and scientifically determining the influential parameters of LLLT, further controlled trials are needed.
Keywords
Low Level Laser Therapy; Wound; Chronic; Clinical Consideration; Mechanism of Action
Download this article as:| Copy the following to cite this article: Rashidi S, Yadollahpour A, Mirzaiyan M. Low Level Laser Therapy for the Treatment of Chronic Wound: Clinical Considerations. Biomed Pharmacol J 2015;8(2) |
| Copy the following to cite this URL: Rashidi S, Yadollahpour A, Mirzaiyan M. Low Level Laser Therapy for the Treatment of Chronic Wound: Clinical Considerations. Biomed Pharmacol J 2015;8(2). Available from: http://biomedpharmajournal.org/?p=5912 |
Introduction
Wounds are among the most common health problems worldwide. Traumatic scars and surgical cicatrix form a wide range of acute and chronic wounds, associated with increased morbidity (1). The significant impacts of wounds incidents on physical and mental health usually drive scientists to find efficient treatments. The classification of wounds into acute and chronic types
is a key to know the medical guidelines and especially the quality of therapeutic cycles in wound treatment. More specifically, surgical wounds are superficial or deep wounds on skin, mucous membranes, fascia, and muscle layers. In conventional wound treatment some specific drugs such as topical administrative ones are used (1). Relatively high prevalence of wounds and high costs of conventional methods as well as emergence of drug resistance of chronic wounds have boosted the rapid raising of alternative wound healing methods. During the last decade several methods based on laser, electric and magnetic fields, light, and ultrasound have been developed as an alternative or adjunctive treatment for chronic and acute wounds treatment (2-7). Despite the limited therapeutic window of low level laser therapy (LLLT) in some patients, laser seems to be a promising hope for many patients. To develop any therapeutic modality, knowing the basic physical and physiological characteristics of the target tissue is the first step (8). To evaluate the wound tissue, study the four basic topics is necessary: history of wound, history and types of previous therapeutic methods, history and types of health-care procedures for wound management, history of previous wound.
Irrespective to whether the wound is superficial or deep, plasma leakage provokes the body’s immune system to activate especial parts of coagulation cascade and inflammatory system which in turn (associated with the formation of
prostaglandins as a result of the effect of cyclooxygenase on membrane phospholipids), through accumulation of serous exudates. During this process, the inflammatory phenomena are
moderate. Gradually, as a result of cooperation of different compound systems, the basal epidermis tissue begins to form epidermis scars. After that, granulation tissue forms dermis scars due to the stimulation of fibrogenesis by adult connective cells; specific mechanism of these cells is their change into fibroblast replacing the fibrocytes by themselves (2, 8-12).
Factors like wound size including depth, width and length, necrotic tissue type, exudate type and amount, surrounding skin color, peripheral tissue edema and granulation tissue are the main parameters determining an appropriate technique for wound healing(8) (13).
Skin is composed of five main layers. The fibroblast layer of the skin includes two main proteins; collagen and elastin. The main rule of these elements is the protection of skin steadfastness. Any trauma damaged this layer caused the skin to lose its consistency. When the injury extends down through dermis layer by passing from keratinocyte, the vessels endothelium
damaged. Now the acute inflammatory phase of the body begins and blood vessels dilation allows migration of especial blood components like monocyte and platelet to the area of the injury (10).
It is important to describe whether the wound is a full thickness or not, because the wound extending through dermis, may involve subcutaneous tissue and possibly bone and muscles. In full thickness wound, bone, tendons, and muscles may not be exposed. In some cases, slough may be seen which does not obscure the depth of tissue loss (9, 14).
Some wounds include necrotic tissues; most of the time hyperglycemia in diabetic patients causes infection, progressive, and necrotic wounds after a simple injury. The main characteristic of such wounds is that the wound depth cannot be
diagnosed if necrotic materials or debris cover the ulcer (14).
Wounds Treatment
Several medications are used for the treatment of wounds (15-19). However, each drug has its own side effects in addition to the gradual increase in drug-resistant behaviors in wound treatment.
To develop and optimize an efficient LLLT technique it is essential to determine the exact mechanisms of action and interaction of laser with living tissues. In this regard, several animal studies have been performed (5, 10, 20-22). These studies showed that hyperglycemia and acidosis delay the wound healing. Laser irradiation can inhibit this process with no serious or bloody exudates (23).
Studies investigating the laser as an adjunctive or alternative treatment for surgical wounds have shown its efficacy in enhancing surgical closure, reducing infection and pain, and shortening the overall wound healing period. Laser therapy showed a promising outcome in the treatment of lower extremity venous ulcer as an adjunctive treatment of standard therapy (15). However, the same protocol failed in the treatment of pressure ulcers (15). Different parameters (wavelength, power, energy, pulse frequency, pulse duration, etc) and irradiation conditions like exposure time, frequency, and duration of treatment influence the treatment outcome (3, 24-26). Therefore, to develop a successful treatment appropriate selection of these parameters is necessary.
LLLT and Wound Treatment
Therapeutic effects of LLLT for treatment of injured tissues and suppression of pain, make this technique to be promoted as a form of laser medicine which use low level (low power) laser or light emitting diodes to alter cellular functions (6, 14). The benefits of LLLT have been proved to be considerable in acute pain treatment, improvement of tissue scars resulting from surgical incision through promotion, fortification, and commissioning of cellular cycle to generate productive and substitute cells (6). The main areas of application of LLLT in medicine are represented in Figure 1 (10).
Low-dosages of laser which are used in LLLT affect enzymatic chain reactions, cellular immunity, the quantity and quality of immune cells, cell proliferation process, tissue secretions, etc by the least systemic side effects and the most
sufficient therapeutic impressions(23, 27).
LLLT Physical Parameters
The most important physical characteristic of laser, making it appropriate for medical therapy, is the dissemination of electromagnetic radiation with particular properties; monochromaticity coherence and low divergence. The intensity of
laser, which is correlated with its spectral distribution, is known as monochromaticity; though for LLLT purposes, this is not a critical parameter. An operational scheme of laser can be described by the excitation of a medium through the introduction of energy(13, 28). The most significant interaction between the laser beam and tissue is absorption. Because of the absorption bands broadness, thereis no specific essential to have a spectrally narrow laser (13, 28).
Laser – Biological Tissue Interaction
Like any other electromagnetic treatment, the primary effects of laser interaction with a biological tissue are divided into thermal and non thermal. LLLT is basically a non thermal energy application. Although delivery and absorption of any energy to the body will produce heat in some extent, non thermal in this context means no accumulative thermal energy occurs or temperature elevation in macroscopic scale is averaged zero. Photobioactivation is a common term for LLLT and indicates stimulating various biological events using light energy without significant temperature changes. There are some other alternative terms such as photobiostimulation and photobiomodulation. When a laser beam, or- a photon, alters the energy level of an atom through shifting between e2 and e3, this event establishes a change in physicochemical cellular function which acts as a trigger agent for beginning a mimicry cascade system. A second photon that will be in phase, propagate in the same direction as the excited photon. This phenomenon, that is called stimulated emission, is the basic of laser light generation. It has been mentioned that in most of the biological tissues, photons are preferably scattered in forward direction.
The laser light possesses some unique characteristics making it appropriate for different medical applications. The most important features include monochromacity, coherence, and polarization. Of these, monochromacity is the most important parameter influencing the therapeutic effects. Previous studies have proposed three main reactions for laser-tissue interactions: photochemical, photothermal and photoplasmal (5, 6, 29). In photochemical reaction, the cell’s function is inactivated temporarily, due to the very low-power irradiation that induced toxic chemical procedures.
In this kind of interaction, light is absorbed by tissue chromophores, besides, the increase of local temperature, triggers the process of heat transmission (conduction) to cooler areas. Noticeably, greater degree of heat may possibly lead to denaturization, necrosis and even vaporization and spallation (29, 30) Irradiation of low intensity visible light can change the activity of biomolecules such as DNA and RNA, but these molecules do not absorb the light directly. The cell membrane is probably the primary absorber of the energy which then generates intracellular effects through a second messenger or cascade type response. The magnitude of this photoresponse is reportedly determined in part by the state of the cells/tissues prior to irradiation, summarized in a simple statement that ‘starving cells are more photosensitive than well fed ones’. The laser light irradiation of the tissues is seen then as a trigger for the alteration of cell metabolic processes, via a process of photosignal transduction. The often cited Arndt-Schults Law supports this proposal.
Several studies have been conducted to shed more light on the understanding of the mechanism of actions of laser medicated wound treatments (1, 3, 9, 16, 28). Various physiological and cellular mechanisms of laser-tissue interaction have been proposed. However, as the majorities of these studies were in vitro, realistic assumptions should be adapted in generalizing the findings into the living mammalian tissues.
The main physiological and cellular effects of laser-tissue interaction are modulation of cell proliferation, cell motility, activation of phagocytes and macrophages, stimulation of immune responses, increasing cellular metabolism, modulation of proliferation of fibroblasts, alteration of cell membrane potentials, stimulation of angiogenesis, alteration of action potentials, and alteration of endogenous opoid production.
Clinical considerations of LLLT in wound
Currently, in clinical settings LLLT is used for different types of wounds as adjunctive or alternative treatment when there is no definitive drug treatment (6, 8). Several clinical trials have been conducted to investigate and develop the LLLT for chronic wounds (25, 31, 32). Among the others, numerous studies were allocated to the diabetic wounds; because the necrotic tissue due to hyperglycemia set aside the highest range of morbidity to themselves like cutaneous wounds including excoriation, superficial and deep wounds due the venous and arterial obstruction (33).
One of the problems in use of LLLT is the application of optimal dose of exposure (34). The lots of inquiry have accomplished on tissues, proved the depth of laser penetration to be different in various tissues, the oral mucosa is quite transplant as the wavelength and does not absorb light well, bone and skin are approximately the same as mucosa, whereas muscles absorb the most light (6, 35). LLLT can be used in such classification as abrasions knife cuts, Para-scrotal wet eczema, necrotic wounds, and inflammation (6, 35).
LLLT has analgesic, vasodilating and antiinflammatory properties (9). Usually, drug administrative and surgical methods are associated with pain, swelling, scars and secretions of wound individually but lasers can affect the whole factors; for example laser stimulates microcirculation which leads to the change of capillary hydrostatic pressure that may results in absorption of edema and eventually eliminating of inflammatory metabolites (8, 25, 36).
Dose Considerations
One of the main challenges in developing laser therapy in the clinical setting is contradictions in defining one global dose units. Different studies have reported different units of doses. In addition different laser machines work with different units such as Joules/ cm2, Joules, Watts, watts/cm2, etc. The most critical and reliable dose unit for laser therapy is energy density in J/cm2. Few devices enable the practitioner to set the dose in J/cm2.
However, most recent studies and evidence have argued that Joules (energy) may be the most critical
parameter rather than energy density. For dose calculation, some machines offer on board calculation and other machines require the operator to make calculations. The common considerations for dose calculation are summarized in Table 1. The most guidelines suggest that the energy density per treatment session should be within the range of 0.1 – 12.0 J/cm2. However, there are some instructions, for special diseases and exposure conditions that recommend up to 30 J/ cm2.
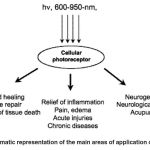 |
Figure 1: Schematic representation of the main areas of application of LLLT (10) |
It has been previously suggested that a maximal (single treatment) dose of 4 J/cm2 should not be exceeded. The evidence would not support that contention. Again as a generality, lower doses should be applied to the more acute lesions which would appear to be more energy sensitive.
LLLT Advantages over other treatments
The process of wound healing is a dynamic and intricate procedure which considered as a natural response to any injury occurs in live tissues. An initial factor for reaching to the successful and efficient treatment of wounds is following post treatment procedure and assessment of the entire patient (27).
Clinicians usually attach more importance to this clinical operation in drug administrative methods. Drugs which are usually administered in wound healing have both systemic and localized impressions. Systemic effects and also side effects of drugs require specific evaluation. By application of LLLT, we have this opportunity to affect specific areas so the risk of any systemic effects especially on vital organs will be elicited (35).
Electrical and magnetic stimulations are the two main techniques used for wound healing (2, 11). Electrical stimulation is an adjunctive therapy that is underutilized in plastic surgery and could improve flap and graft survival, accelerate
postoperative recovery and decrease necrosis. It also has been suggested to reduce infection and improve cellular immunity. Enhancing the perfusion of tissue as an additional effect of electrical stimulation, help expedite wound healing.
Obviously one of the problems which appear in wounds is insufficient oxygen supply; this will prevent normal healing process. Additional oxygen supply to wounds particularly necrotic ones as in diabetic ulcers will accelerate healing procedure.
It has been shown that LLLT helps to eliminate hypoxia and the ischemia had been induced to the tissue by means of obstruction of the vascular system(22, 37).
Future Perspectives
According to the wide range of LLLT application specifically in the field of wound healing, now laser therapy is not just a science, but an amenable technique for almost any kinds of wound. Therefore for the purpose of achieving better results; researches are underway that will help to improve the techniques and devices used for laser therapy
(7).
Clinical application of laser is easy by the specialists and fortunately can be well tolerated by the patients. Though, scientists continue to get supportive data and wound related researches for both enhancing LLLT therapeutic quality and frustrating or at least minimizing the adverse effects/ side effects (25, 31, 32, 38-40).
Hopefully by further trials and researches, LLLT will be investigated to determine if it can be well efficient in augmentation of other regenerative therapies such as cell therapy, platelet rich plasma,
or skin grafting (39).
Conclusion
Despite widespread studies on different aspects of LLLT in wound healing, several main questions still remain unanswered. The exact mechanisms of laser-tissue interaction, crucial parameters determining the therapeutic outcomes and efficacy of LLLT on different chronic wounds treatment are the main issues need further research. LLLT shows high therapeutic efficacy for different chronic wounds particularly skin wounds and diabetic ulcers and necrotic wounds. Further controlled trials in combination with molecular and cellular level assessments are needed to expand our knowledge on the exact mechanisms of action.
References
- Rocha Júnior AM, Vieira BJ, Andrade LCFd, Aarestrup FM. Effects of low-level laser
therapy on the progress of wound healing in humans: the contribution of in vitro and in vivo experimental studies. Jornal Vascular Brasileiro. 6(3):257-65 (2007). - Mostafa J, Ali Y, Zohre R, Samaneh R. Electromagnetic Fields and Ultrasound Waves in Wound Treatment: A Comparative Review of Therapeutic Outcomes. Biosci, Biotech Res Asia.; 12(Spl.Edn.1):185-95 (2015).
- Samaneh R, Ali Y, Mostafa J, Mahmud NA, Zohre R. Laser Therapy for Wound Healing: A Review of Current Techniques and Mechanisms of Action. Biosci, Biotech Res Asia.; 12(Spl.Edn.1):217-23 (2015).
- Yadollahpour A, Jalilifar M. Electromagnetic Fields in the Treatment of Wound: A Review of Current Techniques and Future Perspective. J PURE APPL MICROBIO.; 8(4):2863-77 (2014).
- Al-Watban FA, Zhang XY, Andres BL. Lowlevel laser therapy enhances wound healing in diabetic rats: a comparison of different lasers. Photomedicine and laser surgery.; 25(2):72-7 (2007).
- Hopkins JT, McLoda TA, Seegmiller JG, Baxter GD. Low-level laser therapy facilitates superficial wound healing in humans: a triple-blind, sham-controlled study. Journal of athletic training. 39(3):223 (2004).
- Green JB, Metelitsa AI. Optimizing outcomes of laser tattoo removal. Skin Therapy Lett.; 16(10):1-3 (2011).
- Hawkins D, Houreld N, Abrahamse H. Low level laser therapy (LLLT) as an effective therapeutic modality for delayed wound healing. Annals of the New York Academy of Sciences.; 1056(1):486-93 (2005).
- Calin MA, Coman T, Calin MR. The effect of low level laser therapy on surgical wound healing. Romanian Reports in Physics. 62(3):617-27 (2010).
- Hamblin MR, Demidova TN, editors. Mechanisms of low level light therapy. Biomedical Optics 2006; International Society for Optics and Photonics (2006).
- Yadollahpour A, Rezaee Z. Electroporation as a New Cancer Treatment Technique: A Review on the Mechanisms of Action. Biomedical & Pharmacology Journal.; 7(1):53-62 (2014).
- Yadollahpour A, Rashidi S. Therapeutic Applications of Electromagnetic Fields in Musculoskeletal Disorders: A Review of Current Techniques and Mechanisms of Action. Biomedical and Pharmacology Journal.; 7(1):23-32 (2014).
- Karu T. Photobiological fundamentals of lowpower laser therapy. Quantum Electronics, IEEE Journal of; 23(10):1703-17 (1987).
- Baranoski S, Ayello EA. Wound care essentials: Practice principles: Lippincott Williams & Wilkins; (2008).
- Lauchli S. [Alternative methods for wound treatment]. MMW Fortschritte der Medizin.; 149(46):41-2 (2007).
- Randall P, Randall RJ. The effects of various methods of treatment on wound healing: an experimental study. Plastic and reconstructive surgery; 14(2):105-17 (1954).
- Shal’nev AN. [New methods and means for local wound treatment]. Voenno-meditsinskii zhurnal. 9:72-3 (1985).
- Szmyt K, Lukasz K, Bobkiewicz A, Cybulka B, Ledwosinski W, Gordon M, et al. Comparison of the effectiveness of the treatment using standard methods and negative pressure wound therapy (NPWT) in patients treated with open abdomen technique. Polski przeglad chirurgiczny; 87(1):22-30 (2015).
- Wright AE. An Address on Wound Infections; and on some New Methods for the Study of the various Factors which come into consideration in their Treatment. Proceedings of the Royal Society of Medicine; 8(Gen Rep):41-86 (1915).
- Conlan MJ, Rapley JW, Cobb CM. Biostimulation of wound healing by low energy laser irradiation A review. Journal of clinical periodontology. 23(5):492-6 (1996).
- Rabelo SB, Villaverde AB, Nicolau RA, Salgado MAC, Melo MDS, Pacheco MTT. Comparison between wound healing ininduced diabetic and nondiabetic rats after low-level laser therapy. Photomedicine and Laser Therapy; 24(4):474-9 (2006).
- Mathieu D, Wattel F, Bouachour G, Billard V, Defoin J. Post-traumatic limb ischemia: prediction of final outcome by transcutaneous oxygen measurements in hyperbaric oxygen. Journal of Trauma and Acute Care Surgery. 30(3):307-14 (1990).
- Herranz-Aparicio J, Vázquez-Delgado E, Arnabat-Domínguez J, España-Tost A, Gay- Escoda C. The use of low level laser therapy in the treatment of temporomandibular joint disorders. Review of the literature. Medicina oral, patologia oral y cirugia bucal.; 18(4):e603 (2013).
- Silveira PC, Streck EL, Pinho RA. Evaluation of mitochondrial respiratory chain activity in wound healing by low-level laser therapy. Journal of Photochemistry and Photobiology B: Biology; 86(3):279-82 (2007).
- Medrado AR, Pugliese LS, Reis SRA, Andrade ZA. Influence of low level laser therapy on wound healing and its biological action upon myofibroblasts. Lasers in surgery and medicine; 32(3):239-44 (2003).
- Yadollahpour A, Mostafa J, Samaneh R, Zohreh R. Ultrasound Therapy for Wound Healing: A Review of Current Techniques and Mechanisms of Action. J PURE APPL MICROBIO. 8(5):4071-85 (2014).
- Hussein AJ, Alfars AA, Falih MA, Hassan ANA. Effects of a low level laser on the acceleration of wound healing in rabbits. North American journal of medical sciences; 3(4):193 (2011).
- Lucas C, Criens-Poublon LJ, Cockrell CT, de Haan RJ. Wound healing in cell studies and animal model experiments by Low Level Laser Therapy; were clinical studies justified? A systematic review. Lasers in medical science; 17(2):110-34 (2002).
- Niemz MH. Laser-tissue interactions: fundamentals and applications: Springer Science & Business Media; (2013).
- Welch A, Torres JH, Cheong W-F. Laser physics and laser-tissue interaction. Texas heart institute journal; 16(3):141 (1989).
- Baxter G, Bell A, Allen J, Ravey J. Low level laser therapy: Current clinical practice in Northern Ireland. Physiotherapy; 77(3):171-8 (1991).
- Bjordal JM, Couppé C, Chow RT, Tunér J, Ljunggren EA. A systematic review of low level laser therapy with location-specific doses for pain from chronic joint disorders. Australian Journal of Physiotherapy; 49(2):107-16 (2003).
- Osman AH, Kamel MM, Wahdan MH, Algazaly M. Assessment to the Effects of Low Power Diode Laser on Wound Healing in Diabetic Rats. Life Science Journal. 2:10 (2013).
- Boras VV, Juras DV, Rogulj AA, Panduriæ DG, Verzak •, Brailo V. Applications of low level laser therapy. A textbook of advanced oral and maxillofacial surgery Croatia: In Tech: 327-39 (2013).
- Herascu N, Velciu B, Calin M, Savastru D, Talianu C. Low-level laser therapy (LLLT) efficacy in post-operative wounds. Photomedicine and Laser Therapy; 23(1):70- 3 (2005).
- Ohshiro T, Calderhead RG. Low level laser therapy: a practical introduction: John Wiley & Sons; (1988). 37. Thakral G, LaFontaine J, Najafi B, Talal TK, Kim P, Lavery LA. Electrical stimulation to accelerate wound healing. Diabetic foot & ankle. 4 (2013).
- Gam AN, Thorsen H, Lønnberg F. The effect of low-level laser therapy on musculoskeletal pain: a meta-analysis. Pain.
52(1):63-6 (1993). - Monteiro SO, Lepage OM, Theoret CL. Effects of platelet-rich plasma on the repair of wounds on the distal aspect of the forelimb in horses. American journal of veterinary research. 70(2):277-82 (2009).
- Posten W, Wrone DA, Dover JS, Arndt KA, Silapunt S, Alam M. Low level laser therapy for wound healing: mechanism and efficacy. Dermatologic surgery; 31(3):334-40 (2005).








