Manuscript accepted on :
Published online on: 26-12-2015
Plagiarism Check: Yes
Hassan Zabetian1, Mansour Deylami2, Amir Hossein Sharifian3 and Safar Zarei4
1Department of Anaesthesiology, Jahrom University of Medical Sciences, Jahrom, Iran. 2Department of Anaesthesiology, Golestan University of Medical Sciences, Golestan, Iran. 3Department of Student Research Committee, Jahrom University of Medical Sciences, Jahrom, Iran. 4Department of Physiology, Jahrom University of Medical Sciences, Jahrom, Iran.
DOI : https://dx.doi.org/10.13005/bpj/832
Abstract
Some information may be gathered during the medical procedures, including medical records or personal information. Many of them can be considered as secrets. The medical staff has the duty of privacy, which means keeping the secrets away from a third party. Hippocratic Oath accepts no exceptions but modern ethical references express the situations in which the disclosure of secrets is allowed, legal, or even necessary. The present study is about to evaluate the act of secrecy in medical staff of the tertiary health care centers affiliated with Jahrom University of Medical Sciences in south of Iran. This cross sectional study is done on 204 members of medical staff of 8 different wards in tertiary health care centers affiliated with Jahrom University of Medical Sciences in south of Iran, using a questionnaire of 31 questions in 5 major categories adding to a data sheet for demographic information (age, gender, ward). Validity and reliability of the questionnaire was proved by previous studies. Collected data analyzed by dependent T-test, Fisher’s exact and SPSS.17 using descriptive and deductive statistics. The mean rate of secrecy was 3.82± 0.75. Respecting others in the category of “goals of secrecy” earned 4.48, common medical services in the category of “reasons for disclosure” earned 3.89, damage to the patient in the category of “legal reasons for disclosure” earned 4.05, patient’s rights in “personal reasons for secrecy” earned 4.07, and informing the medical managers in “proper way to confront the offenders” with the score 2.85 were the highest scores of each category. The variant Ages (p=0.003) and wards (p=0.03) showed significant differences in the secrecy. Results show that the medical staff is not familiar enough to the legal and ethical indications of secrecy, so holding in-service courses may be effective.
Keywords
Medical Staff; Patients; Professional ethics
Download this article as:| Copy the following to cite this article: Zabetian H, Deylami M, Sharifian A. H, Zarei S. How Much the Act of Secrecy is Done by Medical Staff? A Descriptive Cross-Sectional Survey in South of Iran. Biomed Pharmacol J 2015;8(2) |
| Copy the following to cite this URL: Zabetian H, Deylami M, Sharifian A. H, Zarei S. How Much the Act of Secrecy is Done by Medical Staff? A Descriptive Cross-Sectional Survey in South of Iran. Biomed Pharmacol J 2015;8(2). Available from: http://biomedpharmajournal.org/?p=3174 |
Introduction
Secrecy is one of the main principles of communication in the society which used to be seen in the relation between patients and physicians for decades, and is mentioned in Hippocratic Oath (1). The oath accepts no exceptions in the secrecy but newer ethical references express some conditions in which the secrets can be released (2).
Hippocrates says: ” Anything I see or hear during the treatment process or even out of that should not be told to others ,and I shame to do so” (3-5). Many information of one’s life may be obtained during the treatment process and most of them are so private that even very close persons to the patient may not know them. Medical secrecy means that the doctor does not disclosure the secrets of the patient (6). Secrets are considered as the information that the patient is not willing to disclose them, adding to them which the doctor figured out himself (7). The doctor is allowed to release that kind of information which may cause damage, only for persons who can prevent that damage.
Principles of medical secrecy are three; subject, individual and the time. The subject is any type of information receiving the doctor from the side of the patient which must be kept classified, even though releasing it is better for the patient himself. Religious and legal laws emphasize confidentiality and the physician will be reprimanded if the information were disclosed (8).
Individual is simply the patient, who possesses some secrets. If the patient is alert and oriented, he talks about his own problem to the doctor. He would be able to tell or not every single secret or important information. In the case of children, mental retards or unconsciousness, the parents have the authority about the secrets (1). One’s health records belong to him and others should not have access to them without permission; if did so, the autonomy would be tarnished. All the medical staff is considered to observe the patient’s secrecy (1).
The third principle is time. Responsibility to keep the medical records secret would not be finished by the end of the relation between doctor and the patient. Records can’t be released after the retirement of the doctor. Neither curing nor death of the patients don’t cause releasing the information. Privacy is a life-long process (1).
Secrecy is explained by either ethics or law. From the ethics point of view, patients don’t give enough information to the doctor if they doubt the privacy. This causes poor performance of the doctor. Moreover, secrecy is an act of respect to the man’s autonomy (9, 10).
Law protects the secrecy. Offering any medical record to a third party without the permission of the patient is forbidden unless allowed by the law itself (11). If there is a threat to the patient or others which can be prevented by releasing the secret, doing so would be not only legal but also necessary. However the possibility of danger should be real and imminent (12). College of physicians and surgeons of Ontario accepts the disclosure of secrets when the patient strongly says he wants to harm another person. In these cases, secrecy would be considered as violation (13). So on the CMA code of ethics, physicians are allowed to release the secrets whether requested by the law or if possibility of damage to the patient or others exists (14, 15). Disclosure of the information should be to the extent required, and only for the individuals who can prevent the damage (4).
Methods
Participants
The present descriptive cross-sectional survey was conducted in summer and autumn of 2012. The census samples included 204 members of treating staff in 8 different wards of gynecology, pediatrics, surgery, orthopedic, internal medicine , coronary care unit (CCU), neonatal intensive care unit (NICU), and the emergency department of tertiary health care centers affiliated with Jahrom University of Medical Sciences in south of Iran.
Procedure
The researcher obtained a license from the research council of the Iranian Ministry of Health and attended the hospitals in order to explain the goals of the study to the eligible staff and fill the questionnaires. After explaining the objectives of the survey to the authorities at the studied health care centers, the assistant visited all the wards to gather data. The questionnaires were distributed in different working shifts. The questionnaires, handed out all at once, were completed by the nurses at their leisure and returned.
Questionnaire
The validity and reliability of the self-made questionnaire confirmed by 5 experts .The reliability was confirmed by Cronbach’s alpha= 0.8. The questionnaire consisted of demographic information (age, gender, job experience and the ward) adding to 31 questions in 5 categories: goals of secrecy (questions 1-8), reasons for disclosure of secrets (9-19) , legal cases for disclosure(20-23), personal reasons for secrecy (24-27) and confronting the offenders (28-31). Each category contained 5 scores in which score5 showed the best and score 1 showed the least satisfaction.
Data Analysis
The sample size was calculated using 90% confidence intervals, with 2% precision. A sample size of about 177 individuals was suitable for this survey. To compensate for any refusal to provide data or nonvaluable subjects the sample size (177 individuals) was increased by 20%. Results were reported as the means ± standard deviation (SD) or median for quantitative variables and percentages for categorical variables. The groups were compared using the Student’s t-test and the chi-square test (or Fisher’s exact test if required) for categorical variables. P values of 0.05 or less were considered to be statistically significant. All the statistical analyses were performed using SPSS version 17.0 (SPSS Inc, Chicago, IL, USA) for Windows.
Ethical Consideration
The study was undertaken after being completely approved by the Institutional Review Board of the Iranian Ministry of Health. Written informed consent was obtained from each participants before their enrolment to the study.
Results
From the 204 samples, 134 (65.68 %) were female and 70 (34.32%) were male. 126 (61.7%) were in the range of 20 to 30 years old. 120 (58.8%) had 5 to 10 years of job experience. The distribution among different wards was as following: 35 members (17.1%) from gynecology ward, 29 (14.2%) from pediatric ward, 27 (13.3%) from emergency department, 26 (12.7) from surgery ward, 23 (11.3%) from orthopedic ward, 24(11.8%) from the internal ward, 21 (10%) from C.C.U and 19 (9.5%) from N.I.C.U.
Highest scores of every category is as follow: Goals of secrecy: 4.48, reasons of disclosure: 3.89, legal cases for disclosure: 4.05, personal reasons for secrecy: 4.07, confronting the offenders: 2.85. The mean scores in category of goals of secrecy is shown in Table 1. Respecting others earned the most (4.48) and preventing the defensive behavior of the patient got the least (3.94) scores in this category.
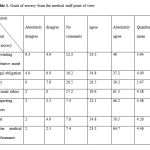 |
Table 1: Goals of secrecy from the medical staff point of view |
The reasons for disclosure of the medical records is shown in Table 2. Mean scores of subcategories are too close to each other (3.31 to 3.89) which may be concluded as low knowledge of the medical staff of allowed disclosure occasions.
 |
Table 2: Reasons for disclosure |
According to Table 3, the major legal reason for disclosure is paralysis of the patient (4.05). However, no significant differences were seen between the subcategories (P>0.05).
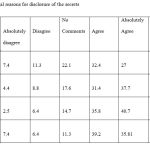 |
Table 3: Legal reasons for disclosure of the secrets |
Observing the patient’s rights (4.07) and professional ethics (4.03) are the major personal reasons of secrecy, in front of social norms (3.75) (Table 4).
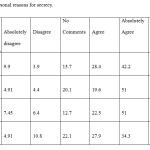 |
Table 4: Personal reasons for secrecy |
According to Table 5, the results of the question” how to confront the offenders?” legal procedure was the most popular answer (3) and cutting the salary and benefits earned the least score (2.53).
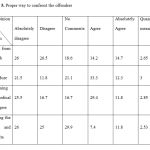 |
Table 5: Proper way to confront the offenders |
Discussion
Faber et al concluded that internal specialists do not decide to disclose the secrets according to the probability of violent actions from the side of the patient. History of previous violence and criminal records increases the probability of disclosure (16). Most of the patients of Cheng et al had issues that they didn’t wanted to be disclosed, which resulted in a poor tendency of following up (17).
Physicians should respect the privacy of the patients. The only information which is allowed by the patient himself may be a subject to offer a third party. For this, medical staff should be aware of the legal procedures. Ensuring and convincing the patient before the disclosure can also help.
In the case of strong threat for damages, act of disclosure would be preferred to secrecy, even there is not enough of legal request. The doctor should evaluate the dangers which threaten the patient from the disclosure, and which threaten a third party if kept secret. The correct decision is that prevents further damages for everybody. Making the right decision is serious.
As a conclusion, Secrecy is essential, but not absolute. Making the least damage for individuals and the society is the determinant of secrecy or disclosure. The best decision would be proved by wisdom and the law. Physicians are responsible for their patients’ medical records and any other kind of secrets lifelong. Base on the results which showed that the medical staff is not familiar enough to the legal and ethical indications of secrecy, so holding in-service courses may be effective.
Acknowledgments
This article was partly based on the thesis written by Dr. Sharifian, and was financially supported by the Jahrom University of Medical Sciences.
Disclosure of interest
None of the authors have any conflict of interest to declare.
References
- Javadpour M , Jabali M ,Raei M. A study of medical confidentiality in jurisprudence and law. Medical Law ; SUMMER 2010; 4(13);133-160.
- Edelstein L. The Hippocaratic Oath: text, translation and interpretation . In : Burns C, editor. Legacies in ethics and medicine. New York: Science History Publications, 1977 : 12.
- Ghobadifar MA, Mosalanejad L. Evaluation of staff adherence to professionalism in Jahrom University of Medical Sciences. Education & Ethic In Nursing. 2013, 2(2):1-10.
- Maarefi F, Ashktorab T, Abaszadeh A, Alavimajd M, Eslamiakbar R. Compliance of nursing codes of professional ethics in domain of clinical services in Patients Perspective. Education & Ethic In Nursing. 2014, 3(1):27-33.
- World Medicine Association. International code of medical ethics (1949) In: Encyclopedia of bioethics. New York: Free press, 1978 : 1749-50.
- Jean V. Mc Hale. Medical Confidentiality and Legal Privilege. ISBN: 0-415-04695-5- Routledge-1993
- Kleinman I , Baylis F , Rodgers S , Singer PA. Bioethics for clinicians : 8. Confidentiality . CMAJ 1997 ; 156 (4) : 521-524.
- Aghakahni n, Shari F, Sharifnia H, Hekmatafshar M, Beheshtipour N, Jamaiy Moghadam N, et al. Survey of Nursing Students’ views regarding professors’ adherence to professional ethics in Shiraz University of Medical Sciences, 2010. 2013, Education & Ethic In Nursing. 2(3):0-0.
- Williams J.R., Medical ethics Manual. By: The World Medical Association, 2005: p51.
- Taregh Salah al-din M, Masouliat-e-Tabib Al-jenaeiyah Al-motorattebah Ala Ifsha Al-ser al-mehani : URL : http://Kanoun.roo7.biz/t4238-topic(accessed on: 2010).
- Ghanoon tashkil nezam pezeshki Jomhouri Islami-e-Iran va Ainamehaye Mortabet, 1st Edition, Tehran, Pishgaman Tose-eh, 2006: p15-25.
- Sharp F. Confidentiality and dangerouseness in the doctor – patient relationship. The position of the Canadian Psychiatric Association. Can J Psychiatry 1985 ; 30 : 293-6.
- Duty to warn: report from council members dialogue. Toronto: college of physicians and surgeons of Ontario,1996:2-21.
- Confidentiality and disclosure of health information. Guidance from BMA’s Medical Ethics Department at BMA Website: bma.org.uk
- Canadian medical association. Acquired immunodeficiency syndrome .CMAJ 1989 ; 140 : 64A-B.
- Faber NJ, Winer JL, Boyer EG, Robinson EJ. Residents decisions to breach confidentiality. J Gen Intern Med 1989 ; 4 ; 31-3.
- Cheng TL, Savageau JA, Sattler AL, Dewitt TG. Confidentiality in health care : a survey of knowledge , perceptions and attitudes among high school students. JAMA 1993 ; 269 : 1404-7.







