Manuscript accepted on :
Published online on: 25-12-2015
Plagiarism Check: Yes
Masoomeh Adib1, Atefeh Ghanbari1*, Cyrus Emir Alavi2 and Ehsan Kazemnezhad Leyli3
1Social Determinants of Health Research Center (SDHRC), Guilan University of Medical Science, Rasht . IR Iran.
2Anesthesiologist, Vascular Surgery and Dialysis research Center, Guilan University of Medical Science, Rasht . IR Iran
3Biostatistic, Social Determinants of Health Research Center (SDHRC), Guilan University of Medical Science, Rasht . IR Iran.
DOI : https://dx.doi.org/10.13005/bpj/519
Abstract
Airway suction is one of the most popular methods for drainage airways in patients with artificial airway; thus, correct suction of airways is important. Hence, the purpose of this study is to determine the effects of suction methods with and without normal saline on hemodynamic and respiratory patients. This randomized crossover clinical trial was conducted on two groups consisting of 37 mechanically ventilated patients by suctioning with and without normal saline. After at least 2 hours, the second stage was conducted and the patients were displaced in groups A and B. respiratory and hemodynamic parameters were measured at different intervals. The average age of patients was 21.8 ± 51.2; in terms of consciousness, 70% of patients were Sedate. Systolic blood pressure (P = 0.20), diastolic blood pressure (P <0.0001), average arterial pressure (P <0.0001) and heart rate (P <0.0001) increased over time immediately after the suction and then declined; in approximately 5 minutes after suction, it approached its baseline. This difference was significant in other cases except for systolic blood pressure. The mean respiratory rate, mean airway pressure, mean oxygen-saturated haemoglobin, mean end-tidal carbon dioxide were similar in both suction groups with and without normal saline during different time steps and no significant differences were observed. As long as there is no sufficient evidence to use normal saline on endotracheal suctioning, this method is not recommended to be used routinely. It is recommended to substitute strategies such as airway hydration, adequate hydration of patients, early mobilization of patients and administration of mucolytic drugs.
Keywords
Endotracheal suction; normal saline; intensive care units; hemodynamics; respiration
Download this article as:| Copy the following to cite this article: Adib M, Ghanbari A, Alavi C. E, Leyli E. K. Effect of Endotracheal Suctioning with and without Normal Saline on Hemodynamic and Respiratory Parameters in Patients Undergoing Mechanical Ventilation in ICU of Hospitals Supervised by Guilan University of Medical Sciences. Biomed Pharmacol J 2014;7(2) |
| Copy the following to cite this URL: Adib M, Ghanbari A, Alavi C. E, Leyli E. K. Effect of Endotracheal Suctioning with and without Normal Saline on Hemodynamic and Respiratory Parameters in Patients Undergoing Mechanical Ventilation in ICU of Hospitals Supervised by Guilan University of Medical Sciences. Biomed Pharmacol J 2014;7(2). Available from: http://biomedpharmajournal.org/?p=3079 |
Introduction
Patients receiving mechanical ventilation require endotracheal intubation to their airway. endotracheal tube causes several problems for the patient, including weakened cough reflex due to closure of the glottis and more concentrated secretions due to removal of a part of the upper airway which keeps the air warm and humid [1].
On the other hand, artificial airway and positive pressure ventilation induces increased production of bronchial secretions; because the patient loses the ability to cough while mechanical ventilation, secretions tend to accumulate and obstruct the airway [2]. There are ways to clean airway including chest physiotherapy, frequent position changes, moving a patient quickly, wetting airway and airway secretion suctioning [1]. Airway suctioning is one of the most common methods done in patients with artificial airway [3]. The number of suctions is based on patient needs [1]. Therefore, the number of suctions is different in each disease. Its average has been reported 7-18 times daily [4].
Despite the necessity of suction in some patients, this approach can lead to complications such as damage to the trachea, bleeding, infection, cardiovascular and hemodynamic disturbances, impaired blood gas exchange and hypoxemia, bronchoconstriction, atelectasis, increased intracranial pressure, impaired blood supply to the brain and increased resistance and airway pressure [5, 6]. In addition, patients complain about pain and discomfort and a feeling of suffocation during suctioning [7]. These effects lead to an increase in the patient’s stay in hospital and intensive care unit and impose on-going costs to the patient and family [8]. Despite all these complications, patients believe it is necessary and makes breathing easier [7]. Various methods are used to drain secretions in the suctions. Suction may be applied open or closed, deep or shallow, with or without normal saline [3]. Due to the health risks associated with this suctioning approach, it is necessary to examine the method of suctioning by nurses and guidelines are required to prevent non-uniformity [7]. One of the most common methods used to drain secretions is to inject a normal saline before suction of trachea. The results of a study in USA showed that 74% of hospitals use normal saline when suctioning [9]. It has been nearly two decades that normal saline has been used before suctioning secretions, in intensive care units around the world. This is based on the hypothesis that 3-5ml normal saline reduces adhesion and instillation of secretions, and makes the suction catheter more slippery and, as a mechanical stimulator, stimulates the cough reflex, and ultimately leads to increased discharge of secretions and permits easier movement of secretions [10, 2]. However, there is insufficient evidence to support this theory. Some studies have shown that normal saline has no advantage but can even be harmful [11]. Possible side effects of insertion of normal saline during suctioning include impaired alveolar gas exchange and decreased oxygen-saturated haemoglobin, decreased venous oxygen saturation, increased incidence of nosocomial pneumonia and increased intracranial pressure [12].
Several studies have been conducted to evaluate the effects of normal saline. Ji showed that inserting normal saline influences haemoglobin saturation and reduced it [13], whereas Akgui showed that normal saline did not cause significant difference in oxygen saturation and gases in atrial blood [14]. Another study also showed that normal saline did not influence the concentration of oxygen and carbon dioxide, but decreased the arterial oxygen saturation. Noting the side effects such as increased heart rate, this study also pointed out that stimulatory effect of normal saline on increased cough reflex led to hypertension and increased intracranial pressure [15], while some other studies found no change in blood pressure after suctioning with normal saline [7, 16]. Meanwhile, Punchalski pointed out the effect of normal saline to dilute concentrated secretions and moist the suction catheter [17].
Despite many controversies, normal saline before suctioning is one of the most common interventions in respiratory care. Studies show that 74% of American medical centres use normal saline for suctioning the airway [17]. Given that tracheal suctioning is associated with high complications [16, 18, 19], therefore, there has been always disagreements on how to do it and factors which cause effectiveness of discharge [14, 19]. Thus, the purpose of this study is to determine the effects of suctioning methods with and without normal saline on hemodynamic and respiratory condition of patients.
Materials and Methods
This study was a randomized crossover clinical trial for two groups in two steps. Participants included mechanically ventilated patients with tracheal tube admitted to the intensive care unit of Poursina and Razi Hospital, a referral centre for patients requiring special care in Rasht, Gilan province in northern Iran.
A total of 74 patients were selected by gradual sampling and participated in six cases based on four random blocks each including 37 patients.
Patients were included in the study who had a 7-8 endotracheal tube, were connected to the mechanical ventilator with adjustable volume for at least 48 hours and at most one week and had a stable hemodynamic condition (high systolic blood pressure 90mmHg, urine at least 30ml/h of balanced electrolytes without serious arrhythmias).
Patients who had a history of heart diseases, hypertension, chronic obstructive pulmonary diseases and a history of cardiac and respiratory drug use as well as patients who used muscle relaxant drugs or their ventilator was adjusted in the studied period and patients who did not require suction after 2 hours were excluded.
The data was collected in three parts. The first part is about demographic characteristics (age and sex), the second part includes clinical characteristics (type of disease, level of consciousness, ventilator mode and level of PSV, PEEP, fio2), and the third part includes results of measurements of hemodynamic and respiratory parameters.
Patients were initially divided in group A (suctioning with normal saline) and B (suctioning without normal saline) based on four random blocks in six permutation modes AABB, BBAA, BABA, ABAB, ABBA and BAAB which were used in 12 quaternary combinations to meet the sample size. Legal guardians of patients were asked to provide informed consent before enrolling in the study.
Suction was conducted only when the patient required suction. For this purpose, the respiratory parameters including respiratory rate, mean airway pressure (MAP), peak airway pressure (PIP), the degree of oxygen-saturated haemoglobin (O2 Sat), exhaled carbon dioxide (ETco2) and the hemodynamic parameters including heart rate, systolic and diastolic blood pressure and mean arterial blood pressure were measured and recorded before the suction. Thus, percentage of oxygen-saturated haemoglobin and end-tidal carbon dioxide, systolic and diastolic blood pressure and mean arterial blood pressure and heart rate were measured by a monitor connected to the patient. In addition to non-invasive measurement of blood pressure, this monitor was equipped with pulse oximeter and Capnograph. Moreover, respiratory rate, mean airway pressure and peak airway pressure were measured by a ventilator attached to the patient.
Then, suction was conducted for patients in group A without normal saline and group B with 5ml normal saline, as follows:
Before suctioning, the patient was given 100% oxygen for 2 min; then, suction was performed using a proper suction catheter (half of the diameter of the endotracheal tube) for 10 seconds a central suction with similar conditions for all patients. Then, BP (systolic, diastolic and mean arterial blood pressures), heart rate, respiratory rate and mean airway pressure and peak airway pressure at specified intervals, that is, immediately after suctioning and then 2 and 5 minutes later, as well as the percentage oxygen-saturated haemoglobin and end-tidal carbon dioxide at 15, 30 and 45 seconds and then 1, 2, 3, 4 and 5 minutes immediately after the suction were measured and recorded.
After at least two hours (wash out), the second phase of the study was conducted where patients in groups A and B were replaced together. If necessary, the suction was performed in each groups of patients, according to the new group. Measurements of respiratory and hemodynamic parameters were performed at intervals.
reliability of the monitoring device, Saadat Novin, which is capable of measuring hypertension, oxygen-saturated haemoglobin, end-tidal carbon dioxide as well as Evita 2 ventilator Drager, which is capable of measuring respiratory rate and mean airway pressure and peak airway pressure was confirmed by repeated utilization of the clinical environment (at least 3 times). By inserting data in software SPSS21, descriptive (mean, frequency) and analytic (paired t-test, independent t, wilcoxon, Mann-Whitney) statistics, analysis of repeated measures (RM ANOVA) were used for analyses. The significance level of tests was considered P <0.05.
Results
The results showed that 66% of patients were male, age ranged between 18-78 years (mean= 51.2 ± 21.07); in terms of alertness, 70% of patients were Sedate and 82.4% were on breath mode SIMV (mean, FiO2: 48/2 ± 12/8, PEEP: 5/1 ± 1/7, PSV: 12/8 ± 3/8) receiving mechanical ventilation.
Evaluation of blood pressure conducted in the phase prior to suctioning and three steps after suction (immediately 2 and 5 minutes later) found that mean systolic and diastolic pressures before suctioning were significantly different from the times after suctioning; therefore, no significant difference was found in the two methods with and without normal saline.
The repeated measure analysis of variance (RMANOVA) on hemodynamic parameters showed that systolic blood pressure (P = 0.20) and diastolic blood pressure (P <0.0001) and mean arterial pressure (P <0.0001) and heart rate (P<0.0001) increased immediately after suction and decreased after that over time. In 5 min after the suction, it almost approached its baseline; this difference was significant in other cases except for the systolic blood pressure. In addition, the results of RMANOVA using Green House test showed no interaction effect between two suction methods at different times in relation to hemodynamic parameters.
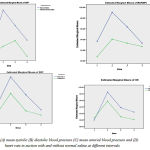 |
Figure 1: (A) mean systolic (B) diastolic blood pressure (C) mean arterial blood pressure and (D) heart rate in suction with and without normal saline at different intervals
|
On respiratory parameters, the results indicate that the respiratory rate, peak inspiratory airway pressure (PIP) and mean airway pressure (MAP), oxygen-saturated haemoglobin (O2sat) after suctioning with or without normal saline increased in both groups, but the difference was not significant. While tidal carbon dioxide (ETco2) significantly increased in group B in 45 seconds after suction (P = 0.03); however, no significant increase was found in 3 minutes (P = 0.46) and 4 minutes (P = 0.21) after suctioning.
RMANOVA on variations of respiratory parameters showed that the mean respiratory rate decreased immediately after suctioning, and increased subsequently; it approximately approached its baseline in 5 minutes, which was not statistically significant (Figure 5).
The mean peak airway pressure (PIP) decreased immediately after suctioning by 2.4 cmH2o and then increased; it approached the baseline in 5 minutes. These differences were not significant (Figure 6).
Mean pressure airway (MAP) which was 9.86 cmH2o in the pre-reduction increased gradually after the suction and reached 11cmH2o in 5 minutes after suctioning, but the difference was not statistically significant (Figure 7). The mean oxygen-saturated haemoglobin immediately dropped after suction, but the fluctuations were slight afterwards; these differences were not significant (Figure 8).
The mean end-tidal carbon dioxide slightly reduced immediately after suction (by 1mmHg); then, it increased and at the end of the fifth minute after suctioning approached to the baseline (Figure 9). RM ANOVA using Greenhouse test showed no interaction effect between the two methods of suction at different periods in relation to respiratory parameters measured above. In other words, respiratory response of both groups was similar to both suction methods with/without normal saline at different intervals and no significant difference was found between them (Figure 5-9).
 |
Figure 2: (A) the mean respiration rate, (B) PIP, (C) MAP, (D) O2Sat, (E) ETco2, in both suctions with and without normal saline at different intervals
|
Discussion
The results of the present study showed that systolic and diastolic blood pressures and mean arterial pressure increased after suctioning with or without normal saline. Although the increase in blood pressure was slightly higher in suction with normal saline, this difference was not significant in systolic and diastolic blood pressures at any time of suction for none of the two groups. While the increase in mean atrial blood pressure was significant over time immediately after the suction. Hypertension is an effect of endotracheal tube suctioning; its major cause is the pain caused by complications of suctioning which causes sympathetic stimulation and muscle contraction [20]. In Zaman and Shojaei, patients experienced an increase in blood pressure, particularly systolic blood pressure, after the suction [21]. Others also evaluated the effects of suction with normal saline on hemodynamic conditions including hypertension; the results indicate that normal saline inserted while suctioning increases blood pressure, but the difference is not significant [5, 7, 16, 22].
The results of this study are consistent with above studies. However, these studies have not evaluated mean arterial pressure. While this study found a significant increase in mean arterial pressure immediately after suctioning. In this case, suction as an invasive procedure leads to physiologic responses; the body response to suction as a stimulator has been higher in the phase immediately after the suction. This caused significant changes. The increase was light; therefore, the increase seems insignificant clinically. On the other hand, increase in cough reflex as a result of normal saline can lead to increase in mean atrial pressure [16].
In this study, the heart rate increased in both suctions with and without normal saline, but the increase was higher in suction with normal saline. However, the increase was not significant at any other time after the suction except for immediately after the suction. Suction can cause both tachycardia and bradycardia (due to vagus nerve stimulation) [23]. In this study, patients only experienced increase in heart rate, while 5% of patients experienced bradycardia in Zaman and Shojaei [21]. In Akgul, the results showed an increase in heart rate of patients in 4 and 5 minutes after the suction with normal saline rather than the suction without normal saline. As a stimulator, normal saline significantly increased the heart rate in patients [14]. Other study indicated that normal saline increased heart rate in 4-5 minutes after the suction, but it had no effect on blood pressure [16], while other studies indicated a significant difference in increased heart rate caused by suction with and without normal saline [7, 24].
Concerning respiratory parameters, results showed that respiratory rate, peak airway pressure, oxygen-saturated haemoglobin and tidal carbon dioxide immediately decreased slightly after suction with and without normal saline. There was a significant difference between this and the time before suction as well as between both suctioning groups (with and without normal saline). Above respiratory parameters approached its baseline subsequently after the suction by slight increase and partial fluctuations. These effects were not significant in none of the time intervals and in none of the studied groups. The results also showed that mean airway pressure increased insignificantly at all times after the suction in both studied groups (with and without normal saline).
Results of some studies suggest that suction with normal saline does not influence oxygen-saturated haemoglobin, while other studies indicate a decrease in this parameter even to 5 minutes after the suction [7]. Akgul showed that suction with and without normal saline insignificantly reduced oxygen-saturated haemoglobin [14], which is consistent with this study. In contrast, other studies indicated that normal saline significantly reduced oxygen-saturated haemoglobin. This reduction increased over time by higher amount of normal saline [13, 16]. Najaf Yarandi showed that oxygen-saturated haemoglobin reduced in both suctions even in 20 minutes after the suction; this difference was significant in suction with normal saline [15].
Another study conducted on children showed that suction with normal saline considerably reduced oxygen-saturated haemoglobin, which was significant in 1 and 2 minutes after the suction [12]. Another study found significant reduction in oxygen-saturated haemoglobin in 4, 5 and 10 minutes [5]. Results of a review showed that although evidence indicate a reduction in oxygen-saturated haemoglobin by using normal saline, these changes are not significant clinically [25]. Reduction in oxygen-saturated haemoglobin after suction may be due to the interruption of ventilation and anxiety during suctioning. In these cases, the negative effects of suction seem to be transient. Further decrease in oxygen-saturated haemoglobin by suction with normal saline indicates harmful effects of normal saline o the patient’s oxygenation [9]. A study using normal saline showed that only 10.7 to 18.7% of normal saline exited after the suction; therefore, the residual can disturb the alveolar gas exchange [12].
Findings indicate that tidal CO2 increased after suctioning by minor fluctuations, but this difference was not significant, while Akyolcu and Akgul showed the reduction in the amount of tidal carbon dioxide after suctioning, which was not significant in both groups [14]. Another study also showed that tidal CO2 decreased even in 20 minutes after suction [15]. Here, the differences were not significant, while Zaman and Shoaei showed that hyperinflation before suction increased tidal CO2. In fact, hyperinflation which is a type on increase in pulmonary ventilation was followed by tidal CO2 [21]. Zahran found no significant difference in the amount of CO2 before and after the suction, but a significant increase in tidal CO2 by suction with normal saline after the suction [22]. In the present study, reduced pulmonary ventilation decreased tidal CO2 immediately after the suction; probably, drainage secretions improved pulmonary ventilation and increased tidal CO2.
The results of this study showed that the effect of suction with and without normal saline on other respiratory parameters including respiratory rate and airway pressure was negligible and changes were not significant. Thus, the respiratory rate approached the baseline in 5 minutes after the suction by partial fluctuations and the peak airway pressure decreased over time; moreover, the mean airway pressure slightly increased.
Drainage secretions after endotracheal tube suctioning decreased the airway resistance, increased the pulmonary dynamic compliance and finally reduced the peak airway pressure; however, the endotracheal tube suctioning is not able to discharge secretions of the peripheral airways [6]. Maybe this is a reason for keeping the airway pressure high. In Zahran, respiratory rate significantly increased immediately after suctioning with and without normal saline, while lung dynamic compliance significantly reduced simultaneously [22].
In literature, little is known on the effects of suction on airway pressure. In this regard, a study on physiologic effects of suction with and without normal saline on respiratory rate, peak airway pressure and values of atrial blood gases indicated no significant difference between two methods [26].
In general, suction with or without normal saline causes changes in hemodynamic and respiratory parameters. Although suction with normal saline causes negative effects, the changes are not significant except for increase in heart rate. This suggests that the changes do not cause a major risk. However, results of other studies found a significant relationship. Perhaps, the results of present study are due to the lack of samples and different design of the study; therefore, a broader study is required.
Yet, systematic reviews emphasize that little is known on helpfulness as well as side effects and risks of normal saline. In this regard, better quality clinical trials are required [25]. It is recommended to conduct other studies with different designs and more samples as well as measurements in different times.
Therefore, it is recommended to avoid routine administration of normal saline as long as the evidence lacks on tracheal suction. It is recommended to substitute strategies such as airway hydration, adequate hydration of patients, early mobilization of patients and administration of mucolytic drugs to minimize the side effects of suction.
Acknowledgement
The authors appreciate the staff of the Intensive Care Unit of the Poorsina and Razi medical centres, Rasht, for their collaboration in sampling procedures.
References
- Brunner LS, Smeltzer SCC, Bare BG, Hinkle JL, Cheever KH. Brunner & Suddarth’s textbook of medical-surgical nursing: Lippincott Williams & Wilkins; 2010.
- Black JM, Hawks JH. Medical-Surgical Nursing: Clinical Management for Positive Outcomes: Saunders/Elsevier; 2009.
- Branson RD. Secretion management in the mechanically ventilated patient. Respiratory care. 2007;52(10):1328-47.
- Jongerden IP, Rovers MM, Grypdonck MH, Bonten MJ. Open and closed endotracheal suction systems in mechanically ventilated intensive care patients: a meta-analysis. Critical care medicine. 2007;35(1):260-70.
- Favretto DO, Silveira RCdCP, Canini SRMdS, Garbin LM, Martins FTM, Dalri MCB. Endotracheal suction in intubated critically ill adult patients undergoing mechanical ventilation: a systematic review. Revista latino-americana de enfermagem. 2012;20(5):997-1007.
- Pedersen CM, Rosendahl-Nielsen M, Hjermind J, Egerod I. Endotracheal suctioning of the adult intubated patient—What is the evidence? Intensive and Critical Care Nursing. 2009;25(1):21-30.
- Lorente L, Lecuona M, Jiménez A, Mora ML, Sierra A. Tracheal suction by closed system without daily change versus open system. Intensive care medicine. 2006;32(4):538-44.
- Kohan M, Yarandi AN, Peyrovi H, Hoseini F. The Effects of Expiratory Rib Cage Compression before Endotracheal Suctioning on Arterial Blood Gases in Patients Under Mechanical Ventilation. Iran Journal of Nursing. 2007;20(51):37-49.
- Giakoumidakis K, Kostaki Z, Patelarou E, Baltopoulos G, Brokalaki H. Oxygen saturation and secretion weight after endotracheal suctioning. British Journal of Nursing. 2011;20(21):1344.
- Reeve JC, Davis N, Freeman J, O’Donovan B. The use of normal saline installation in the intensive care unit by physiotherapists. a review of practice in New Zealand. 2008.
- Care AAfR. AARC Clinical Practice Guidelines. Endotracheal suctioning of mechanically ventilated patients with artificial airways 2010. Respiratory care. 2010;55(6):758.
- Ridling DA, Martin LD, Bratton SL. Endotracheal suctioning with or without instillation of isotonic sodium chloride solution in critically ill children. American Journal of Critical Care. 2003;12(3):212-9.
- Ji YR, Kim HS, Park JH. Instillation of normal saline before suctioning in patients with pneumonia. Yonsei Medical Journal. 2002;43(5):607-12.
- Akgül S, Akyolcu N. Effects of normal saline on endotracheal suctioning. Journal of Clinical Nursing. 2002;11(6):826-30.
- Najaf yarandi a, Tanourifard m, Nikpour s, Haghani h. The effects of Endotracheal suctioning with normal saline on arterial blood gases Iranian Journal of Nursing and Midwifery. 2000;28:39-46.
- Halm MA, Krisko-Hagel K. Instilling normal saline with suctioning: beneficial technique or potentially harmful sacred cow? American Journal of Critical Care. 2008;17(5):469-72.
- Puchalski ML. Should Normal Saline be Used When Suctioning the Endotracheal Tube of the Neonate? Medscape Nurses2007 [updated March 14, 2007; cited 2014]. Available from: http://www.medscape.com/viewarticle/552862.
- Caruso P, Denari S, Ruiz SA, Demarzo SE, Deheinzelin D. Saline instillation before tracheal suctioning decreases the incidence of ventilator-associated pneumonia*. Critical care medicine. 2009;37(1):32-8.
- Celik SA, Kanan N. A current conflict: use of isotonic sodium chloride solution on endotracheal suctioning in critically ill patients. Dimensions of critical care nursing. 2006;25(1):11-4.
- Arroyo-Novoa CM, Figueroa-Ramos MI, Puntillo KA, Stanik-Hutt J, Thompson CL, White C, et al. Pain related to tracheal suctioning in awake acutely and critically ill adults: A descriptive study. Intensive and Critical Care Nursing. 2008;24(1):20-7.
- Zaman B, shoaaee A. The effects of Endotracheal suctioning on hemodynamic and arterial blood gases journal of iranian society of Anaesthesiology & Intensive care. 2001;35:38- 44.
- Zahran EM, El-Razik AA. Tracheal suctioning with versus without saline instillation. Journal of American Science. 2011;7(8):23-32.
- Pattie S, Twome B. Endotracheal Tube Suction of Ventilated Neonates: Royal Children’s Hospital melbourne; 2009 [cited 2014 28 may]. Clinical Guidelines (Nursing)]. Available from: http://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Endotracheal_Tube_Suction_of_Ventilated_Neonates/.
- Rafiee Hossein Is, Sabzevari S. Comparison Of The Endotracheal Tube Suctioning With And Without Normal Saline Solution On Heart Rate And Oxygen Saturation. Iranian Journal Of Critical Care Nursing (Ijccn). 2011.
- Overend TJ, Anderson CM, Brooks D, Cicutto L, Keim M, McAuslan D, et al. Updating the evidence base for suctioning adult patients: A systematic review. Canadian respiratory journal: journal of the Canadian Thoracic Society. 2009;16(3):e6.
- Gray J, MacIntyre N, Kronenberger W. The effects of bolus normal-saline instillation in conjunction with endotracheal suctioning. Respir Care. 1990;35(8):785-90.







