Manuscript accepted on :28-Sep-2019
Published online on: 30-09-2019
Plagiarism Check: Yes
Reviewed by: Dr Balram Ji Omar
Second Review by: Sadhna Sodani
Final Approval by: Dr. Ian James Martin
Rajaseger Nirmal Kumar1 , Preetha Selva2*
, Preetha Selva2*
1Saveetha Medical College and Hospital, SIMATS, Chennai, India
2Department of Pharmacology, Saveetha Medical College and Hospital, SIMATS, Chennai, India
Corresponding Author E- Mail: drpreethaselva@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/1790
Abstract
Respiratory tract infections are very common in developing countries like India. The main objective of the present study is to analyze prescription pattern of antibiotics given to outpatients with respiratory tract infections visiting our Hospital and to assess the rationality of these prescriptions given, using World Health Organisation core drug prescribing indicators. A total of 423 prescriptions were analysed after screening for inclusion and exclusion criteria. The number of males were 271 (64%) and females 152 (36%). 232 (54.84%) patients belonged to >60 years age group. Among the various respiratory tract infections, 148 patients (34.98%) were diagnosed to have Chronic Obstructive Pulmonary Disease (COPD), 141 patients (33.33%) Pulmonary Tuberculosis, 71 patients (16.78%) Bronchial Asthma, 34 patients (8.03%) Pneumonia and 29 patients (6.85%) had Upper Respiratory Tract Infections (URTIs). The total number of drugs prescribed were 2368 out of which 447 (18.87%) were mucolytics/expectorants, 433 (18.28%) antibiotics, 350 (14.78%) bronchodilators, 332 (14.02%) corticosteroids, 295 (12.45%) Antitubercular Treatment Category (ATT CAT) drugs, 209 (8.82%) antacids, 112 (4.72 %) anti histamines, 98 ( 4.13%) vitamin tablets, and 92 (3.88) miscellaneous drugs. The most commonly used mucolytic/ expectorant was a fixed dose combination of acebrophylline+ acetylcysteine (327). The most common corticosteroid prescribed was Prednisolone (217). The antibiotics that were commonly prescribed were azithromycin (122), doxycycline (84), ciprofloxacin (82), cefpodoxime + clavulanic acid (61), ceftriaxone (32), amoxicillin + clavulanic acid (27) and piperacillin+ tazobactam (8). Ranitidine (184), levocetrizine (68) or fexofenadine (36), vitamin b complex (79) were the most commonly prescribed antacid, antihistamine and vitamin tablet respectively. The drug formulations prescribed were oral 1842 (77.78%) , inhalations 375 (15.83%), injections 55 (2.32%), syrup 37 (1.56%), gel 36 (1.52%), powder 23 (0.97%). An average of 5.59 drugs was prescribed per prescription. Percentage of drugs prescribed by generic name was 456 (19.3%). Percentage of encounter with antibiotics prescribed was 94%. Percentage of encounters with injection was 9.25%. Percentage of drugs from NLEM was 40.09%. Percentage of fixed dose combinations prescribed were 13.38% . In our study it is observed that more number of drugs can be prescribed from National List of Essential Medicines. Prescription of drugs by generic name also needs improvement. Since the study is done on outpatient setting , culture and sensitivity reports might not be readily available. So choosing an antibiotic might be a dilemma for the physician. There is hence a need for educational programmes in order to facilitate rational use of antibiotics and promote sensible use of available resources. Every hospital should also follow standard treatment guidelines taking into consideration the sensitivity pattern of the organisms in the locality to promote rational prescribing. This study serves to spotlight the current prescribing trends in patients with respiratory tract infectons visiting our hospital.
Keywords
Drug Utilization; Prescription Pattern; Respiratory Tract Infections
Download this article as:| Copy the following to cite this article: Kumar R. N. Selva P. Analysis of Prescription Pattern of Antibiotics Among Patients with Respiratory Tract Infections at A Tertiary Care Hospital. Biomed Pharmacol J 2019;12(3). |
| Copy the following to cite this URL: Kumar R. N. Selva P. Analysis of Prescription Pattern of Antibiotics Among Patients with Respiratory Tract Infections at A Tertiary Care Hospital. Biomed Pharmacol J 2019;12(3). Available from: http://biomedpharmajournal.org/?p=28877 |
Introduction
Respiratory tract infection (RTI) is defined as the Infection of the upper or lower respiratory tract.[1] The most common upper respiratory tract infections (URTI) include- common cold, laryngitis, pharyngitis, otitis media, tonsillitis, acute rhinitis, acute rhino- sinusitis etc..[2] Lower respiratory tract infection (LRTI) mostly includes pneumonia, bronchiolitis and bronchitis.[2] Both upper and lower respiratory tract infections are very common in developing countries like India.[3] According to previous studies, respiratory tract infections are one of the most common causes of physician consultation in our country.[4] The widely used drugs for treatment of any respiratory tract infection is antibiotics.[5] Most of the respiratory infections are viral in origin and therefore does not require antibiotic prescription. However there is inadvertent prescription of antibiotics in many patients with respiratory tract infections irrespective of the underlying aetiology.[6] Antibiotics are also being prescribed for non specific symptoms like common cold, running nose and sore throat for which there is no therapeutic benefit.[7,8] Broad spectrum antibiotics are being prescribed to adult patients with respiratory tract infections which is also on a rise.[9,10] According to Centre for Disease Control and Prevention Guidelines (CDC), acute upper respiratory tract infections resolve spontaneously without the need for anti microbial therapy. The treatment with antibiotics is indicated only when the patient have symptoms sustained for at least 10- 14 days without showing any improvement. The inappropriate and over use of antibiotics leads to increased emergence of antimicrobial resistance in the community apart from increased expenditure on health care, adverse effects and poorer outcomes.[11,12] Hence good prescribing practises should be followed to provide maximum clinical benefit and minimum risks to the patient.
The study of prescription pattern is one of components of medical audit which evaluates the prescribing patterns of health care practioners as well as recommends necessary changes in the prescribing pattern to provide best medicine to the patient. Thereby prescription pattern studies are an important indicator to judge the quality and standard of clinical practice among health care professionals.
The current study is aimed to analyze the prescription pattern of antimicrobials used in patients with upper and lower respiratory tract infections visiting our hospital. This will help us gain knowledge on prevalence of respiratory tract infections in our locality, the most common respiratory tract infection, current prescribing trends of antimicrobials and finally assessing the rationality of the prescriptions.
Objectives
To evaluate the prescription pattern of antibiotics given to patients with respiratory tract infections visiting General Medicine and Pulmonary Medicine Out Patient Department of our Hospital
To assess the rationality of these prescriptions given, in our hospital using WHO core drug prescribing indicators.
Methodology
Study Design
Prospective Observational Study.
Study Duration
The study was conducted for a period of 4 months starting from December 2018 to March 2019.
Study Place
The study was conducted in General Medicine and Pulmonary Medicine Outpatient Department of Saveetha Medical College and Hospital
Sample size
The appropriate sample size required for the study was determined using the statistical formula based on confidence interval, margin of error and population proportion.[13]
Study Population
Inclusion criteria
All patients attending General Medicine and Pulmonary Medicine Out Patient Department diagnosed with upper or lower respiratory tract infection
Exclusion criteria
All the in-patients of concerned Department were excluded from the study
Illegible prescriptions were excluded.
Incomplete data were excluded
Procedure
The study was carried out after getting approval from the Institutional Ethics Committee. Permission to carry out the study was also obtained from Head of General Medicine and Pulmonary Medicine Departments before starting the study.
Data of all patients attending General Medicine and Pulmonary Medicine Department diagnosed with respiratory tract infection during the study period was collected. Detailed information on age, gender, diagnosis, drugs used including name of the drug, dosage schedule (form, route, and frequency), and duration of treatment was recorded from the prescriptions given to the patients. The brand names of the drugs prescribed was decoded to generic names using latest version of standard Current Index of Medical Specialities (CIMS) India- (October 2018- January 2019)
Rationality of prescribing the drugs was evaluated by using the WHO core drug prescribing indicators.
Results
Diagnosed cases of respiratory tract infection visiting the General Medicine and Pulmonary Medicine OPD during the study period were identified and enrolled in the study. The treatment received by these patients were noted from the prescriptions given to them. Totally 423 prescriptions were included in the study after screening for inclusion and exclusion criteria. Out of 423 patients, the number of males were 271 (64%) and females were 152 (36%). The male female ratio was 1.78:1. Out of 423 patients, 232 (54.84%) patients belonged to >60 years age group. (Table- 1)
Table 1: demographic details
| Parameters | Number | |
| Male: Female Ratio | 1.78:1
|
|
| Age (years) | 18-30 | 34 (8.03%) |
| 30-45 | 89 (21.04%) | |
| 45-60 | 68(16.07%) | |
| >60 | 232 (54.8%) | |
Among the various respiratory tract infections, 148 patients (34.98%) were diagnosed to have Chronic Obstructive Pulmonary Disease (COPD), 141 patients (33.33%) Pulmonary Tuberculosis, 71 patients (16.78%) Bronchial Asthma, 34 patients (8.03%) Pneumonia and 29 patients (6.85%) had Upper Respiratory Tract Infections (URTIs). (Figure-1)
 |
Figure 1: Prevalence of various respiratory tract infections |
The total number of drugs prescribed were 2368 out of which 447 (18.87%) were mucolytics/expectorants, 433 (18.28%) antibiotics, 350 (14.78%) bronchodilators, 332 (14.02%) corticosteroids, 295 (12.45%) ATT CAT drugs, 209 (8.82%) antacids, 112 (4.72 %) anti histamines, 98 ( 4.13%) vitamin tablets, and 92 (3.88) miscellaneous drugs.(Figure-2)
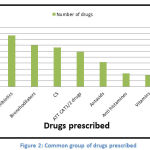 |
Figure 2: Common group of drugs prescribed |
The most commonly used mucolytic/ expectorant was a fixed dose combination of acebrophylline+ acetylcysteine (327). The most common corticosteroid prescribed was Prednisolone (217). The antibiotics that were commonly prescribed were azithromycin (122), doxycycline (84), ciprofloxacin (82), cefpodoxime + clavulanic acid (61), ceftriaxone (32), amoxicillin + clavulanic acid (27) and piperacillin+ tazobactam (8). Ranitidine (184), levocetrizine (68) or fexofenadine (36), vitamin B complex (79) were the most commonly prescribed antacid, antihistamine and vitamin tablet respectively. (Figure 3)
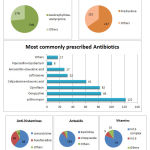 |
Figure 3: Commonly prescribed drugs in each group |
The drug formulations prescribed were oral 1842 (77.78%) , inhalations 375 (15.83%), injections 55 (2.32%), syrup 37 (1.56%), gel 36 (1.52%), powder 23 (0.97%). (Table- 2)
Table 2: Drug formulations given
| Drug formulations | Number of drugs |
| Oral | 1842(77.78%) |
| Injections | 55(2.32%) |
| Inhalables | 375(15.83%) |
| Gel | 36(1.52%) |
| Syrup | 37(1.56%) |
| Powder | 23(0.97%) |
An average of 5.59 drugs was prescribed per prescription. Percentage of drugs prescribed by generic name was 456 (19.3%). Percentage of encounter with antibiotics prescribed was 94%. Percentage of encounters with injection was 9.25%. Percentage of drugs from NLEM was 40.09%. Percentage of fixed dose combinations prescribed were 13.38% (Table- 3).
Table 3: WHO Prescribing indicators assessed
| S.No | WHO prescribing indicators | Number |
| 1 | Average drugs per encounter | 5.59 |
| 2 | Percentage of drugs prescribed by generic name | 19.3% |
| 3 | Percentage of encounter with antibiotics prescribed | 94% |
| 4 | Percentage of encounters with injection prescribed | 9.25% |
| 5 | Percentage of drugs from NLEM | 40.09% |
Discussion
Drug utilization studies have become a special tool to evaluate the health care systems specially in developing countries like India. These studies will help us analyze different aspects of use of drugs and will also be beneficial in improvising the quality and standards of treatment given. A total of 423 prescriptions given to patients with respiratory tract infections were included in our study, out of which 64% were males and 36% were females. This is similar to the studies conducted by S. Ganesh kumar et al and Jadhav et al who also reported increased number of males when compared to females in their study.[14,15]
The most commonly affected patients belonged to > 60 yrs age group which is similar to studies conducted by Mirza A. Beg et al and Mahajan HM et al. This shows that elderly patients are more at risk of developing respiratory tract infections when compared to other age groups.[16,17]
The most common respiratory tract infections for which the patient came to the hospital were chronic obstructive pulmonary disease 148 (34.98%), pulmonary tuberculosis 141 (33.33%), bronchial asthma 71 (16.78%), lower respiratory tract infections 34 (8.03%) and upper respiratory tract infections 29 (6.85%). These findings are in accordance with the other previous studies done on respiratory tract infections.[16,17,18]
Mucolytics / expectorants 447 (18.87%) were the most commonly prescribed group of drugs followed by antibiotics 433 (18.28%), bronchodilators 350 (14.78%), corticosteroids 332 (14.02%) and others. In study done by Sujata Jadhav et al antipyretics (98.3%) were the most commonly given group of drugs.[15] This might be because the study was done in children of one to five years, whose most common presenting symptom for respiratory tract infection is fever. Since adult patients were included in the present study mucolytics and expectorants would have been given to bring symptomatic relief in the patient. In a study done by Mirza et al, antibiotics were most commonly prescribed drugs which covered about 56.56% of the total prescribed drugs.[16] This is quite high and inadvertent prescription of antibiotics can lead to antimicrobial resistance. A few vitamin and mineral supplements like Iron, Vitamin B complex, Vitamin D and Calcium tablets were also given in our study. These must have been prescribed to improve appetite, generalized fatigue and weakness associated with the illness.
Among the mucolytics, fixed dose combination of acebrophylline and acetylcysteine were most commonly prescribed which does not match with any study conducted till date. Prednisolone was the most commonly used steroid which is similar to study done by Mirza A. Beg et al.[16] The most commonly prescribed antibiotic was azithromycin in our study which was similar to the study done by Pramil et al.[19] This is comparable to study done by Mirza et al , Pandit PR et al , Errabelly P et al who reported levofloxacin, amoxicillin and cephalosporins as the most commonly used antibiotics respectively.[16,18,20] This shows that a wide variety of antibiotics are being prescribed by practioners for respiratory tract infections irrespective of origin of infection whether bacterial or viral . The choice of antibiotic depends on the clinician prescribing the drug. However, if Respiratory tract infection is very severe after investigation antiviral therapy may be given. Antimicrobial stewardship can be followed to avoid antibiotic overuse and antimicrobial resistance. It will also decrease unnecessary costs in a developing country like India and improve patient outcomes as well.
Among the antibiotics which are available as fixed dose combinations, cefpodoxime+ clavulanic acid was the most frequently prescribed in our study whereas in studies conducted by Mirza. A et al and Mahajan et al it was piperacillin+ tazobactam and amoxicillin + clavulanic acid respectively.[16,17] All these fixed dose combinations of antibiotics are penicillin and cephalosporin group of antibiotics. With this we come to a conclusion that B-Lactam antibiotics are the most commonly prescribed fixed dose combinations of antibiotics for treatment of respiratory tract infections.
Among the drug formulations, oral form was the most commonly given followed by inhalations and injectables in our study. This is similar to the study done by Tiwari et al; however slightly different from the study by Mirza et al which showed higher use of injectables than inhalations though the most commonly prescribed drug formulation was oral route.[16,21] Oral route is the most common drug formulation in the present study since the study was conducted in outpatient adult patients who are less sick compared to children and in patients who might require more of inhalations and injectables for quick relief of symptoms.
In the present study, an average of 5.59 drugs was prescribed per prescription. In other similar studies, the average number of drugs prescribed was 2.24, 2.81 and 3.4 which is quiet less than our study.[19,22,23] This might be because these studies were done on paediatric patients with only acute upper respiratory tract infections. Whereas in our study, both acute and chronic respiratory tract infections were included which might contribute to more number of drugs when taken as average. However, in previous studies conducted on both acute and chronic respiratory tract infections by Mirza A. Beg et al and Gogoi S et al the average number of drugs per prescription was 8.32 and 6.62 respectively which is higher than the present study.[16,24] Higher number of fixed dose combinations used might be possible explanation for lower number of drugs prescribed in our study.
Percentage of drugs prescribed by generic name was 456 (19.3%). This is more than the findings by Sujata Jadhav et al, Mungrue K et al and Pal et al where the percentage of drugs prescribed by generic name was 0%, 0% and 0.56% respectively.[15,25,26] The number of generic drugs prescribed were less in the previous studies possibly because prescription of drugs by generic name was made mandatory only after September 2016. However, the percentage of drugs prescribed by generic name in the presnt study is still low and has to be improved.
Percentage of encounter with antibiotics prescribed was 94% which is similar to studies done previously.[15,27] Hence, it is evident that clinicians mainly want to focus on the treatment of infection and bring about symptomatic relief in the patient. But awareness have to be created among them for judicial use of antibiotics.
Percentage of encounters with injection was 9.25%. This finding is less than the findings done by Vandana Badar et al where it was 23.2% as the later study was done on children with acute respiratory tract infections and obviously require more drugs through parenteral route.[28]
Percentage of drugs from NLEM was 49.09%. This is similar to the findings done by Mirza A. Beg et al.[16] However in studies done by Sujata Jadhav et al and Pal et al it was 97.32% and 67.07% respectively.[15,26] There is a scope for improvement in prescribing drugs from National List of Essential Medicines.
Percentage of fixed dose combinations prescribed was 13.38%. This is similar to study done by Mirza et al 13.24%.[16] The advantages of prescribing fixed dose combinations are increased patient compliance, synergy, reduced side effects and reduced cost. But it also has few disadvantages like inflexible fixed dose ratio, increased toxicity and ignorance of the physician with respect to the constituents of the combination.
Conclusion
Prescription pattern studies have become a potential tool for evaluating the health care systems. In our study it is observed that more number of drugs can be prescribed from National List of Essential Medicines. Prescription of drugs by generic name also needs improvement. Since the study is done on outpatient setting , culture and sensitivity reports might not be readily available. So choosing an antibiotic might be a dilemma for the physician. There is hence a need for educational programmes in order to facilitate rational use of antibiotics and promote sensible use of available resources. Every hospital should also follow standard treatment guidelines taking into consideration the sensitivity pattern of the organisms in the locality to promote rational prescribing. This study serves to spotlight the current prescribing trends in patients with respiratory tract infectons visiting our hospital.
Acknowledgement
We are thankful to the faculty members of General Medicine and Pulmonary Medicine for granting us the permission and for their guidance throughout the study. We also express our heartfelt thankfulness to the patients who participated and co-operated to help us complete the study.
Conflict of interest
None declared
Funding source
No funding sources
References
- Prescribing of antibiotic for self limiting respiratory tract infections in adults and children in primary care; Nice Clinical Guidelines in UK. 2008; 8: 69.
- Mlynarczyk G, Mlynarczyk A, Jeljaszewicz J. Epidemiological aspects of antibiotic resistance in respiratory pathogens. International journal of antimicrobial agents. 2001 Dec 1;18(6):497-502.
- Jain N, Lodha R, Kabra SK. Upper respiratory tract infections. The Indian Journal of Pediatrics. 2001 Dec 1;68(12):1135-8.
- Nandimath MK, Ahuja S. Drug prescribing pattern in upper respiratory tract infection in children aged 1-14 years. Int J Pharm Bio Sci. 2012;3:299-308.
- Butt AA, Navasero CS, Thomas B, Al Marri S, Al Katheeri H, Al Thani A, Al Khal A, Khan T, Abou-Samra AB. Antibiotic prescription patterns for upper respiratory tract infections in the outpatient Qatari population in the private sector. International Journal of Infectious Diseases. 2017 Feb 1;55:20-3.
- Straand J, Rokstad KS, Sandvik H. Prescribing systemic antibiotics in general practice. A report from the More & Romsdal Prescription Study. Scand J Prim Health Care. 1998;16:121–7
- Sun Q, Dyar OJ, Zhao L, Tomson G, Nilsson LE, Grape M, et al. Overuse of antibiotics for common cold-attitudes and behaviors among doctors in rural areas of Shandong Province, China. BMC Pharmacol Toxicol. 2015;16:6.
- Kamikawa J,Hernandes Granato CF, Bellei N. Viral aetiology of common colds of outpatient children at primary care level and the use of antibiotics. Mem Inst Oswaldo Cruz. 2015;110:884–9.
- Kuehn BM. Excessive Antibiotic Prescribing for Sore Throat and Acute Bronchitis Remains Common. 2013;310(20):2135–2136.
- Steinman MA, Landefeld CS, Gonzales R. Predictors of broad-spectrum antibiotic prescribing for acute respiratory tract infections in adult primary care. Jama. 2003 Feb 12;289(6):719-25.
- Harris AM, Hicks LA, Qaseem A. Appropriate antibiotic use for acute respiratory tract infection in adults: advice for high-value care from the american college of physicians and the centers for disease control and prevention. Ann Intern Med. 2016;164(6):425–34.
- Gill JM, Fleischut P, Haas S, Pellini B, Crawford A, Nash DB. Use of antibiotics for adult upper respiratory infections in outpatient settings: a national ambulatory network study. Fam Med. 2006;38(5):349–54.
- Arya R, Antonisamy B, Kumar S. Sample size estimation in prevalence studies. The Indian Journal of Pediatrics. 2012 Nov 1;79(11):1482-8.
- Kumar SG, Majumdar A, Kumar V, Naik BN, Selvaraj K, Balajee K. Prevalence of acute respiratory infection among under-five children in urban and rural areas of Puducherry, India. Journal of natural science, biology, and medicine. 2015 Jan;6(1):3.
- Jadhav S, Khanwelkar C. Prescribing Pattern of Drugs in Acute Respiratory Tract Infection in Children Aged 1 To 5 Years At Tertiary Care Teaching Hospital. Biomedical and Pharmacology Journal. 2018 Dec 25;11(4):1903-11.
- Beg A. M., Dutta B. S.,Bawa S., Kaur A.,Vishal S., Kumar U. Prescribing trends in respiratory tract infections in a tertiary care teaching hospital. International Journal of Research in Medical Sciences. 2017;5(6):2588-91.
- Mahajan HM, Date AP, Badwaik RT, Borkar AS, Wanmali SS, Gohad GV. Analysis of Pattern of Antimicrobial use in Respiratory Tract Infections in a Tertiary Care Hospital of Central India-A Drug Utilization Study. J Cont Med A Dent 2014; 2 (3):59-64.
- Errabelly P, Ramavath V, Afreen A, Sanaboina A. Analysis of the prescribing pattern of antibiotics in respiratory tract infections at department of medicine at a tertiary care teaching hospital. IJPSR. 2015;6(7):2693-97.
- Pramil T., Rajiv A., Gaurav G. Prescription practice in patients of upper respiratory tract infection at a pediatric outpatient clinic in Punjab.Indian Journal of Pharmacy Practice. 2014;7(2):26-32.
- Pandit PR, Kokanii V, Bhave KA. Prescribing pattern of antimicrobials used for the treatment of acute respiratory tract infections in children. IJARSAT. 2016;18(1):171-75
- Tiwari P, Ahlawat R, Gupta G. Prescription patients of upper respiratory tract infection at a pediatric outpatient clinic in Punjab. Indian J Pharm Pract. 2014;7(2):26-32.
- Joshi U., Hishikar R., Agrawal S., Halwai A., Kirtania L.,Kurrey K. Study of drug use in outdoor pediatric patients of upper respiratory tract infections in a tertiary care hospital. International Journal of Basic & Clinical Pharmacology. 2015;4(5):1009-12.
- Das B., Sarkar C., Majumder A. G. Medication use for pediatric upper respiratory tract infections.Fundamental & Clinical Pharmacology. 2006;20(4):385-90.
- Gogoi S, Saikia PP. A study on prescribing pattern of antibiotics for upper respiratory tract infections by general practitioners in rural areas of Assam. IJSR. 2015;4(5):60-2.
- Mungrue K, Brown T, Hayes I Ramroop S, Thurston P, Pereira LP. Drugs in upper respiratory tract infections in pediatric patients in north Trinidad. Pharm Pract. 2009;7(1):29-33.
- Pal P., Bhattacharyya D., Kokila B. N., Herle M., Ghosh A., Sen S. Drug utilization pattern in out-patients with respiratory tract infections in a rural teaching hospital: a prospective observational study. International Journal of Basic & Clinical Pharmacology. 2017;6(12):2894–99.
- Alkahtani A. S. Drug utilization pattern of upper respiratory tract infections in pediatric at Najran university hospital, KSA. Biomedical Research. 2017;28(20):8981-86.
- Badar, Vandana & Parulekar, Vidisha & Garate, Priti .A prescription pattern study of respiratory tract infections in paediatric indoor patients in a tertiary care teaching hospital – A prospective observational study. Asian Journal of Pharmaceutical and Clinical Research. 2018; 11(7):251







