Syeda Nazia Kulsum1, T. Andra Chadha2 and Nawaz Umar1
1K.B.N. Institute of Medical Sciences, Gulbarga - 585 104 India. 2S.N. Institute of Medical Sciences, Eranakulum - 682 026, India.
DOI : https://dx.doi.org/10.13005/bpj/421
Abstract
Parasitic infections cause human suffering and economic loss worldwide but the burden is greatest in under developed countries. Among the effects associated with these parasites are growth retardation, intestinal obstruction, hepatic and biliary diseases, impaired cognitive development and nutritional effects such as iron deficiency anemia. Children because of their habits and opportunity for exposure easily acquire these infestations and are likely to manifest acute syndromes due to ill developed immunity and lack of tolerance against these worms. In the view of above facts, the present study was under taken. A total of 700 stool samples were examined by Gross examination, direct microscopic examination by saline and iodine preparations, to increase sensitivity of microscopic detection Formalin – Ethyl acetate sedimentation technique was employed. An attempt was made to identify Cryptosporidium species by using modified acid fast stain and sheather’s sugar floatation technique. 5)700 blood samples were examined by cell counter to detect Hb and blood indices to know presence of anaemia. The incidence of intestinal parasitic infestation was 173 (24.71%) cases. The most common parasite found was H. nana 49 (7.0%) followed by Ascaris 42 (6.0%), E. histolytica 36 (5.1%), Trichuris 34 (4.9%), Giardia 5 (0.7%), hookworm 3 (0.4%) and Taenia species and E. vermicularis 2 (0.3%) cases respectively. Formalin – ethyl acetate concentration technique has increased sensitivity of intestinal parasite detection from 148 (21.14%) by routine method to 173 (24.71%) cases. Majority of children (122) positive for intestinal parasitic infestation were having anaemia. No sample was found to have Cryptosporidium species. Thus public health education, routine periodic screening, early detection, prompt therapy and interruption of transmission of the pathogens may help mitigate the impact of childhood intestinal parasitosis.
Keywords
Intestinal parasitosis; Formalin Ethyl Acetate; Sedimentation; Hymenolepis nana; Entamoeba histolytica; Enterobius vermicularis
Download this article as:| Copy the following to cite this article: Syeda Nazia Kulsum S. N, Chadha T. A, Umar N. Study of Incidence and Spectrum of Intestinal Parasitic Infestation using Formalin Ethyl Acetate Sedimentation Technique among Children and Its Correlation with Anaemia. Biomed Pharmacol J 2013;6(2) |
| Copy the following to cite this URL: Syeda Nazia Kulsum S. N, Chadha T. A, Umar N. Study of Incidence and Spectrum of Intestinal Parasitic Infestation using Formalin Ethyl Acetate Sedimentation Technique among Children and Its Correlation with Anaemia. Biomed Pharmacol J 2013;6(2). Available from: http://biomedpharmajournal.org/?p=2741 |
Introduction
Strictly speaking any infectious agent can be described as a parasite but the term is usually restricted to the protozoa and helminth worms. These are highly evolved and opportunistic organisms that can be found as parasites in all classes of the animal kingdom. It is not surprising that humans should harbor some parasites but what is remarkable is the number of different species that can infect us, nearly 300 helminth worms and about 100 protozoa1. Intestinal parasitic infestations are globally endemic and have been described as constituting the greatest single worldwide cause of illness and disease2. Although most infections occur in developing countries, developed ones are also affected by migrants and travelers3.
In 1947, Norman Stoll published a landmark paper entitled “this wormy world” in which he set out to estimate the number of people infected with helminthes worldwide. Over the last 60 years several estimates have confirmed Stoll’s initial observation that hundreds of millions of people harbor parasitic worms4.
About one third of the world, more than 2 billion people are infected with intestinal parasites. Approximately 300 million people are severely ill with these worms and of those, at least 50% are school age children2.
According to W.H.O estimate globally there are 800-1000 million cases of Ascariasis, 700 – 900 million cases of Trichuriasis, 200 million cases of Giardiasis and 500 million cases of Amoebiasis5. Among the intestinal parasitic infections, helminthic infections are the most common on the Indian sub-continent5,6.
The extent of the disease depends on the parasitic burden and stage of infestation, the type of tissue response and host immunity. Patients suffering from immunodeficient syndromes may develop severe and fatal forms of parasitic disease3.
Intestinal parasites are transmitted through the contamination of water, soil and food by feces a direct consequence of poor hygienic and living conditions. According to WHO, the level of helminth infection can be viewed as an index of a community’s progress towards a desirable level of sanitation. With the prevalence of such infections being an excellent indicator of socio-economic status5.
In India malnutrition, unhygienic conditions improper disposal of sewage, non availability of portable water supply in rural and urban areas, coupled with low literacy rates of parents particularly the mothers are the main causes of this prevalent malady7. . In children parasitic infestations either present as primary condition for which treatment is sought or incidentally detected when stool examination is done during health surveys or as routine when suffering from other disease. Asymptomatic cases pose a constant threat to the community by perpetuating the chain of transmission to others8
Many of the viral and bacterial infections of gastrointestinal tract have been efficiently controlled by anti microbial drugs and vaccines but no concrete achievement has been made in the field of immunization against intestinal parasitic infestations. Furthermore, because of the maverick ways used by parasites to reach their destination, it is difficult to offer prophylactic therapy against them. Hence even today intestinal parasitic infestations top the list of all intestinal disorders9.
These infestations inspite of their considerable morbidity are often ignored and considered neglected tropical diseases probably due to relatively low incidence of serious morbidity due to such infestations10 and the study of these diseases receives less than 1% of global research dollars4.
Low cost interventions can control parasitic infestations or at least decrease the incidence of these infestations11. It is thus important to know disease burden of parasitic infestations in the communities.
In the view of above facts, the present study was under taken to know the incidence and spectrum of intestinal parasitic infestations among children attending tertiary care hospital Navodaya Medical College, Raichur.
Objectives
To evaluate the incidence and spectrum of intestinal parasitic infestation in children consulting Navodaya hospital and research center, Raichur.
To increase the sensitivity of microscopic detection by Formalin ethyl acetate sedimentation concentration method.
An attempt will be made to identify Cryptosporidium species by using modified acid fast stain and Sheathers sugar floatation technique.
To evaluate the role of worm infestation in children with respect to anaemia
Materials And Methods
The parents of children were provided with clean wide mouthed, dry, screw capped and properly labelled plastic containers for collection of stool samples. The received samples in the lab were examined freshly and processed.
Methods
Stool examination was carried out both macroscopically and microscopically.
Macroscopic examination
The consistency, colour, and nature of feces was recorded. Stools were checked for the presence of bloody – mucous discharge, worms like Ascaris, Enterobious vermicularis, proglottids of Taenia, adult hookworm and Trichuris trichura, either with naked eye or with aid of hand lens.
Direct microscopic examination
With each stool sample, two cover glass preparations were made on one microscopic glass slide12.
Saline preparation
On left hand side a minute portion of the faeces was diluted with a drop of normal saline (0.9 %) on a clean microscopic glass slide. A cover slip (No. 1) was then gently put over it, so as to spread out the emulsion into a thin, fairly uniform and transparent layer.
Iodine preparation
On right hand side, a minute portion of the faeces was emulsified with a drop of iodine solution on microscopic glass slide and cover slip was then put over it. Care was taken to see that the preparations were free of air bubble and macroscopic debris. The preparation was adequate for examination, yet so thin that ordinary news print could be read through it. The unstained saline film was particularly valuable for study of motile protozoan trophozoites, helminth eggs and nematode larvae. The iodine film was useful for detecting the cystic forms of the parasite, when the nuclear character can easily be distinguished12.
Concentration technique
The concentration of stool allows the detection of small number of parasites present in the stool specimens. The concentration procedure allows the increased recovery of eggs and larvae of helminths and cysts of protozoa.
The technique is based on the principle of separating parasites from faecal debris and other faecal materials by their differences in the specific gravity. The concentration method employed was formalin ethyl acetate sedimentation, as it is well known fact that ether is extremely flammable and highly volatile, produces anaesthetic vapours. Unlike that of ether, ethyl acetate is less flammable and also less expensive and safe as it does not produce any anaesthetic vapour13.
Procedure for formalin-ethyl acetate sedimentation
About 1/4 to 1/2 teaspoon of fresh stool was transferred into 10 ml of 5 – 10% formalin in a 15 ml test tube and comminuted thoroughly. It was kept for 30 minutes to stand for adequate fixation.
This material was filtered in a funnel through 2 layers of gauze into a 15 ml centrifuge tube.
Then 10% formalin was added to within 1.5 cm of the top and centrifuged for 10 minutes at 500 xg.
Approximately 3 ml of ethyl acetate was added to the centrifuged material, stoppered and shaked vigorously for 30 seconds.
Then again it was centrifuged for 10 minutes at 500 xg. Four layers were formed, a small amount of sediment in bottom of tube containing the parasites, a layer of formalin, a plug of faecal debris on top of formalin layer and a layer of ethyl acetate at the top.
The plug of debris was freed off by ringing with an applicator stick and decanted top 3 layers leaving sediment. Then the sediment was examined by wet mount preparation13.
Detection of cryptosporidium species
Modified acid fast stain procedure
A faecal smear was made on the glass side. It was fixed by heat at 70oC for 10 minutes.
The heat fixed slide was kept on the staining rack. The slide was then flooded with carbol fuschin. The slide was then heated till carbol fuschin starts steaming. The slide was allowed to stain for 9 minutes.
The smear was washed with tap water.
The smear was decolourised with 5% aqueous sulphuric acid for 30 seconds.
The smear was washed with tap water and counter stained with methylene blue for 1 minute.
Finally smear was washed with tap water, water drained off and slide air dried and was examined microscopically14.
Sheather’s floatation technique
Routine haematological investigations and blood indices
By cell counter (Micro 60), various blood indices were tested in blood samples like Hb, TC, DC, MCV, MCH, and MCHC to know the presence of anaemic conditions.
Haemoglobin (Hb) level than 11 gm/dl in children between 6 months to 6 years old or below 12 gm/dl in older children is suggestive of anaemia, while those between 5 – 10 gm/dl suggest moderate anaemia15.
Anal swab for Enterobiaisis detection
Cellophane tape preparation:
A piece of cellophane tape was looped over a tongue depressor to expose the adhesive surface.
The adhesive surface of the tape was firmly pressed against the right and left perianal folds at several places and
The tape was then removed and spread on the glass slide with adhesive surface sticking to the slide. A drop of xylene was added between the tape and slide to clear the preparation. Then the slide was examined microscopically13.
Results
Statistical Analysis
Data were analyzed by using Microsoft excel for windows. Descriptive statistics such as proportions and graph are used to present the data. Associations between variables were conducted applying Chi-square test. Comparison of two techniques was done by chi – square test or Fisher’s exact test if sample size is small. A two-tailed P-value < 0.05 was considered statistically significant.
Observations & Results
The study was conducted from Dec.2008 to Nov 2009 over a period of one year. A total of 700 stool samples were examined for intestinal parasites.
Out of total 700 samples examined, 173(24.71%) samples were detected to have intestinal parasite.
The overall incidence of intestinal parasite infection observed in the present study was:
No. of stool sample examined – 700
No. in which presence of IP was found – 173
Percentage – 24.71 %
The spectrum of intestinal parasitic infestation was as follows.
Out of 700 children 132(18.9%) were infested with helminths. H. nana was found to be the most common helminth 49 (7.0%).
Out of 700 children 41(5.8%) were infested with protozoa. E. histolytica 36(5.1%) was most common protozoa found.
The remaining infestations were: Trichuris trichura in 34 (4.9 %) cases, Giardia lamblia in 5 (0.7%) cases, Hook worm in 3 (0.4%) cases, E. vermicularis in 2 (0.3 %) cases, Taenia species in 2 (0.3 %) cases. Overall the incidence of intestinal helminthes was more common as compared to intestinal protozoa H. nana was found to be the most common parasite infesting children in present study.
Result of cellophane tape technique in 100 children apart from the above 700 children was,
No. examined – 100
No. positive – 9
Percentage – 9
To know the true incidence of E. vermicularis, cellophane tape technique was employed. Out of 100 children, 9 (9%) showed the presence of E. vermicularis..
Out of the 700 stool samples examined, 148 (21.14 %) samples were positive by routine direct microscopic method and 173 (24.71%) samples were positive by routine direct microscopy plus concentration method.
There is statistically significant difference between routine method alone and routine plus concentration method (P < 0.0001). Therefore concentration of stool samples by Formalin Ethyl Acetate sedimentation method has increased the sensitivity of microscopic detection from 148 (21.14%) to 173 (24.71%) respectively.
Among 399 anaemic cases majority of children 312 belonging to Hb 5-10g/dl category harboured highest number of IP 101 (32.37%) as compared to 87 children belonging to Hb <5g/dl category harbouring 21 (24.14%) IP.
From blood picture among anaemic cases majority of children showing IP positivity were categorized to typical microcytic hypochromic (52.0%) followed by normocytic hypochromic (21.67%) and then normocytic normochromic (13.95%) category.
Cryptosporidium species
An attempt was made to identify Cryptosporidium species by examining 100 samples out of 700 stool samples by using Modified acid fast stain and Sheathers sugar floatation technique. No sample was found positive for Cryptosporidium species.
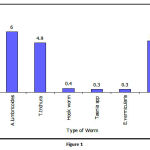 |
Figure 1:
|
Discussion and Conclusion
Of the 700 children attending tertiary care hospital Navodaya medical college, Raichur, 173 children were infested with one or the other parasites, giving an overall incidence of 24.71%.
Even though the western world is on the verge of eradicating helminthiases, developing countries like India still has to do a lot towards this problem. WHO report states that 1 out of 4 persons in the world is suffering from one or the other worm infestation16.
The incidence observed in the present study goes with the report given by Ali haghighi et al (27.3%)17, Boonchai wongstitwilairoong et al(22.7%)18, S. Awasthi et al (17.5%)19,.
Comparatively higher incidence was reported by Anand kumar H et al(71.73%) from Gulbarga20. The prevalence rate reported in India by different workers varies from 14.98 to 63.50% from different areas8.
The prevalence of intestinal worm infestation in India varies from 5% to 76% which is similar to that in other developing countries.
The widely variable incidence reported by many workers is due to many factors. It varies with geographical conditions, the environment, temperature, habits, cast, creed, race, political situation, literacy and most significant the economic condition of the society21.
Most of the workers have conducted the surveys in the general population, but the present study includes children of 6 months to 13 years in the hospital population. Hence the incidence is lower compared to the studies by other workers.
Cellophane tape technique in 100 children apart from the 700 cases revealed the presence of ova of E. vermicularis in 9 children, the incidence being 9%.
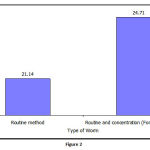 |
Figure 2:
|
Spectrum of IPI
Table 1: Incidence and Spectrum of intestinal helminthes in 700 children
| Type of worm | No. of +ve cases | Percentage |
| Hymenolepis nana | 49 | 7.0 |
| Ascaris lumbricoides | 42 | 6.0 |
| Trichuris trichura | 34 | 4.9 |
| Hook worm | 3 | 0.4 |
| Taenia spp | 2 | 0.3 |
| Enterobius vermicularis | 2 | 0.3 |
| Total | 132 | 18.9 |
Table 2: Incidence and Spectrum of intestinal protozoa in 700 children
| Type | No. of +ve cases | Percentage |
| Entamoeba histolytica | 36 | 5.1 |
| Giardia lamblia | 5 | 0.7 |
| Total | 41 | 5.8 |
Out of 700 children 132 (18.9%) were infested with helminths. The most common helminth was found to be H. nana 49(7.0%)cases next common Ascaris lumbricoides 42(6%) .
41 (5.8%) were infested with Protozoa, E. Histolytica was most common protozoa found 36 ( 5.1%), The incidence of other parasites in descending order was Trichuris trichura 34 (4,9 %), Giardia 5 ( 0.7%),Hook worm 3 (0.4%), Taenia and E. vermicularis 2 ( 0.3%) respectively.
Finding of this study is comparable to study by VG Rao et al reporting H. nana was one of the most common forms of parasitosis observed from Madhya Pradesh10, Anand Kumar H reports 16.36% prevalence of H, nana in their study at Gulbarga20.
The next most common infestation was of Ascaris lumbricoides 42 (6%) cases. Studies by other workers indicates prevalence of Ascaris to be highest, Showkat Ahmed Wani et al (71.18%)5, SA Wani et al (69.84%)6, from Kashmir.
Histolytica was 36(5.1%) the most common Protozoa found in present study. This is in consonance with the study by Hedge GR et al reporting E. Histolytica was the commonest Protozoa found22, Saifi MA et al E. Histolytica exhibited highest rate (14.98%).
Overall in the present study the incidence of Helminthic infestation was higher 132 (18.9%) as compared to Protozoal 41 (5.8%).This is comparable to finding by K.D.Ajwani et al reports helminthic infestation are far more frequent in children than protozoal23,
Hookworm incidence was 3(0.4%) in the present study. It is less as compared to study by V.G Rao reporting hookworm species as one of the commonest form of parasitosis observed from Madhya pradesh10. The environmental sanitation survey there showed open air defaecation was the rule in this villages. Majority of them either did not used footwear or used it occasionally. This could be the reason for higher percentage of hookworm infestation there. The low incidence in present study could be attributable to use of latrines, practice of shoe wearing among the population.
Giardia 5(0.7%) was found in present study , Cellophane tape technique revealed higher incidence of E .vermicularis (9%) as compared to routine stool examination which showed only 2(0.3%).This contrast clearly points out the importance of cellophane tape technique.
Formalin ethyl acetate sedimentation concentration technique
Table-3: Showing the incidence of IP obtained with routine (Saline & Iodine preparation) and routine plus concentration technique
| Technique used | Positive for parasites | Percentage |
| Routine method | 148 | 21.14 |
| Routine and concentration (Formalin Ethyl Acetate) method | 173 | 24.71 |
The concentration of stool samples by Formalin ethyl acetate sedimentation technique has increased the sensitivity of microscopic parasitic detection from 148 (21.14%) by routine (Saline + Iodine) preparation alone to 173(24.71%) respectively. Thus concentration technique will prove useful in diagnosis of additional cases of IPI which would otherwise be missed by routine method alone
Incidence of Anaemia
Out of 700 blood samples examined 399 (57%) were anaemic and 301 (43%) were non-anaemic.
Among 399 anaemic children 122 (30.58%) were positive for IPI and among 301 non-anaemic children 51 (16.94%) were positive for IPI.
Apart from IPI there may be other causes for the present incidence of anaemia.
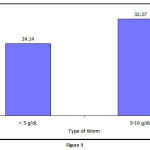 |
Figure 3:
|
Correlation of anaemia and IPI
Table 4: Co-relation of anaemia and intestinal parasitic infestation.
| No. of aneamic cases (n=399) | Positive cases (n=122) | % | |
| 1. Hb % | |||
| < 5 g/dl | 87 | 21 | 24.14 |
| 5-10 g/dl | 312 | 101 | 32.37 |
| 2. Blood picture | |||
| Microcytic hypochromic | 150 | 78 | 52.0 |
| Normocytic hypochromic | 120 | 26 | 21.67 |
| Normocytic normochromic | 129 | 18 | 13.95 |
Among 399 anaemic cases majority of children 312 belonging to Hb 5-10g/dl category harboured highest number of IP 101(32.37%) as compared to 87 children belonging to Hb <5g/dl category harbouring 21(24.14%) IP.
From blood picture among anaemic cases majority of children showing IP positivity were categorized to typical microcytic hypochromic (52.0%) followed by normocytic hypochromic (21.67%) and then normocytic normochromic (13.95%) category.
The study shows that majority of children 122 positive for IPI were having anaemia and the most common type of anaemia found was microcytic hypochromic type.
Amara E. Ezaemama et al in a study states low intensity poly parasite infection were associated with increased odds of having anaemia24.
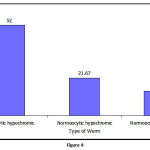 |
Figure 4:
|
Cryptosporidium species
An attempt was made to identify Cryptosporidium species by examining 100 samples out of 700 stool samples by using Modified acid fast stain and Sheathers sugar floatation technique. No sample was found positive for Cryptosporidium species.
Thus childhood intestinal parasitosis still remain a major public health problem worldwide contributing to morbidities and mortality. It is essential to evaluate the incidence of IPI among children not only in symptomatic cases but also among apparently healthy children to know the true burden of the condition.
While public education on improved personal and environmental hygiene are cardinal in the control, additional routine periodic screening of children and possibly the care givers will guarantee early detection, prompt therapy and interruption of transmission of the pathogens. This may help mitigate the impact of childhood intestinal parasitosis in the community.
References
- Francis E.G. Cox. History of human parasitic diseases. Infectious disease clinic of North America. June 2004; 18(2)
- Mehraj V, Hatcher J, Akhtar S, Rafique G, Beg MA. Prevalence and factors associated with intestinal parasitic infection among children in an urban slum of Karachi. PLoS one 2008;3(11): e 3680.
- Mohamed AE, Al Karawi MA, Ghandour Z. Parasitic diseases of the liver and biliary tree. Saudi J Gastroenterol [Serial online] 2008 Sep 14; 3:22-8.
- Peter J. Hotez, Paul J. Brindly, Jeffrey M. Bethony, Charles H. King, Edward J. Pearce and Julie Jacobson. Helminth infections: the great neglected tropical diseases. J Clin Invest. 2008 April 1 ; 118(4): 1311 – 1321.
- Wani SA, Ahmed F, Zargar SA, Amin A, Darza, Dar PA. Intestinal helmenthiasis in children of Gurez valley of Jammu and Kashmir state, India. J Global Infect Dis 2010; 2: 91–4.
- Wani SA, Ahmed F. Intestinal helminths and associated risk factors in children of district Pulwama, Kashmir, India. Indian J Med microbial [Serial online] 2010 may 13; 27: 81–2.
- Ahmed AK, Malik B, Shaheen B, Yasmeen G, Dar JB, Mona AK, et al. Frequency of intestinal parasitic infestation in children of 5–12 years of age in Abbottabad. J Ayub Med Coll Abbottabad. 2003 Apr : Jun; 15(2): 28–30.
- Bhandari, G.P. Gupta and S.L. Mandowara. Prevalence of intestinal parasites in Udaipur. Indian J Pediatr 1985; 52: 299–302.
- Sengupta J and Bhattacharya K. “Distribution of parasitic infestation among hospital patients in Bankura. In. J. Pub. Health. 1962–1969; XIX. 2: 69.
- VG Rao, MC, Aggrawal, R Yadav, SK, Das, L K Sahare, MK Bondley et al. Intestinal parasitic infections, Anaemia and Under nutrition among tribal Adolescent of Madhya Pradesh. Indian Journal of Community Medicine. (2003) Jan–March; 28(1).
- DAP Bundy, MS Chan, GF Medley, D Jamison, L. Savioli. “Intestinal Nematode Infections”. Global Epidemiology of Infectious Diseases. Page 243.
- D. Chatterjee. Parasitology. Protozoalogy and Helminthology. 13th ed. Satish K. Jain and Vinod K. Jain : CBS Publishers and Distributors: Sep 2009.
- Subhash Chandra Parija. Medical parasitology. Protozoalogy and Helminthology. 3rd All India Publishers and Distributors; Reprint 2009.
- Betty A. Forbes, Daniel F. Sahm, Alice S. Weissfeld. Bailey and Seott’s Diagnostic microbiology. 12th Andrew Allen; MOSBY ELSEVIER: 2007.
- P. Ghai, Piyush Gupta, V.K. Paul. Essential Pediatrics. 6th Ed. Rev. 2005.
- H.O Technical report series No. 42.1969.
- Ali Haghighi, Alireza Salimi Khorashad, Ehsan Nazemal hosseini Mojarad, Bahram Ka Zemi, Mohammad Rostami Nejad and Sima Rasti. “Frequency of enteric protozoan parasites among patients with gastrointestinal complaints in medical centers of Zahedan, Iran. Trans R Soc Trop Med Hyg. May 2009; 103(5): 452 – 454.
- Boonchai Wongstitwilairoong, Apichai Srijan, Oralak Secichantalergs, Caroline D.Fukuda, Philip Mc Daniel, Ladaporn Bodhidatta et al. “Intestinal parasitic infections among pre-school children in Sangkhlaburi, Thailand. Am.J. Trop. Med. Hyg. 2007; 76(2): 345–350.
- Awasthi S and Pande VK. Prevalence of malnutrition and intestinal parasites in pre – school children in Lucknow. Indian Pediatr. 1997 July; 34: 599–605.
- Vinod Kumar CS, Anand Kumar H, Sunita V, Indu Kapur. Prevalence of anaemia and Worm infestation in school going girls at Gulbarga, Karnataka. Indian Pediatrics. 2003; 40: 70-72.
- Patel J.C. “Ankylostomaiasis in India: A review with suggestion for future research”. Ind. Med. Res. 1954; 42: 279.
- Hegde GR, Patel TC. Prevalence of intestinal parasitic infestation in rural area. J Postgrad Med. 1986; 32: 225.
- D. Ajwani, H.Saxena and A. kumar. “A Coprological survey of parasitism in children in Kanpur. Indian J. Pediat. 1974; 41: 209.
- Amara E. Ezeamama, Jennifer F. Friedman, Remiglo M. Olveda, Luz P. Acosta, Jonathan D. Kurtis, Vincent Mor et al. “Functional significance of low intensity polyparasite helminth infections in anaemia. JID 2005: 192. 2160 – 2170.








