D. V. Medovnikova1, A. S. Ytuzh1, M. G. Soykher2, I. K. Pisarenko2 and A. S. Onyanova1
and A. S. Onyanova1
1I. M. Sechenov First Moscow State Medical University, Moscow, Russian Federation.
2University of Biotechnology and Interdisciplinary Dentistry, Moscow, Russian Federation.
Corresponding Author E-mail: daria.medovnikova.70@bk.ru
DOI : https://dx.doi.org/10.13005/bpj/1582
Abstract
The study assessed stress and brux activity among dental students during exam (stress) and non-examination (non-stress) periods. The study was initiated as a single group design with the total number of participants 36 (25 females and 11 males). All the participants were examined twice (once in a stress period and once in a non-stress period) according to “Clinical Functional Analysis”, which includes questions about students’ medical and dental history, as well as muscle palpation results. Two «BruxCheckers» (BCs) were applied, one for the upper jaw, the other for the lower jaw, two times for examination and non-examination periods. After the use, the «BCs» were photographed according to the research protocol and the abraded facets area on «BCs» was calculated in square millimeters. The research showed that during a stress period students may have headaches, cramps and pain in shoulder and neck muscles. The research also revealed that during the stress situation the abraded area shifts from frontal teeth to chewing teeth and brux episodes can occur more frequently and with a higher load. Chewing teeth (premolars in our study) are more adapted and more useful for such a condition. Accordingly, our students shifted their brux behavior from teeth 33 and 31 to teeth 15 and 24. Therefore, exams are a strong stress factor for dental students. In turn, prolongated stress can be an indicator of risk factor and have a negative effect for health of the craniomandibular system.
Keywords
Bruxism; Chewing Muscles; Stress Management
Download this article as:| Copy the following to cite this article: Medovnikova D. V, Ytuzh A. S, Soykher M. G, Pisarenko I. K, Onyanova A. S. The Influence of Exams Stress on Brux Activity in Russian Dental Students. Biomed Pharmacol J 2018;11(4). |
| Copy the following to cite this URL: Medovnikova D. V, Ytuzh A. S, Soykher M. G, Pisarenko I. K, Onyanova A. S. The Influence of Exams Stress on Brux Activity in Russian Dental Students. Biomed Pharmacol J 2018;11(4). Available from: http://biomedpharmajournal.org/?p=23882 |
Introduction
The phenomenon of sleep bruxism (SB) remains a debated issue till nowadays. A PubMed search shows that more than 1000 articles devoted to this problem were published over the last 10 years.
What is SB? According to the American Academy of Sleep Medicine, bruxism is a parasomnia, a sleep disorder that is not an abnormality of the processes responsible for sleep and wakeful states.1 The American Academy of Orofacial Pain states that SB can refer to a diurnal or nocturnal parafunctional activity that includes unconscious clenching, grinding or bracing of the teeth.2 Kato et al., Lavigne et al. describe it as a parasomnia and a parafunctional activity during sleep that is characterized by clenching (tonic activity) and/or repetition of phases of muscle activity (phasic activity) which causes the grinding of the teeth.3,4 The International Statistical Classification of Diseases and Related Health Problems defines SB among mental and behavioral disorders Class V, code F45.8: other somatoform disorders.5
Following Slavicek and Sato’s viewpoint on this issue, our research defines SB as a function of the masticatory organ to cope with stress. The chewing organ secures contact between the organism and environment. One of its most important functions is stress management, which is closely related to psyche and environment. Unique individual factors of environment affect each person differently forming a person’s attitude to reality. Therefore, the masticatory organ is a kind of somatic platform for the decrease of stress level.6
It is only natural that students who constantly suffer from stress during their studies may also develop SB. Dental students are no exception. Moreover, according to Cooper, dentistry is one of the most stressful health professions.7-10 Different studies related to stress among dental students have been carried out in many countries worldwide mostly with the help of Dental Environment Stress Questionnaire. It was found that examinations and grades appear to be the most stressful elements, along with limited time for relaxation or outside activities.11 Therefore all these factors can provoke brux activity. During SB strong forces can develop. If these forces do not provoke craniomandibular disorders, we speak about normal brux-activity as a mechanism to deal with stress management. But when the functional stability of the system is low for such strong forces, signs and symptoms of craniomandibular disorders may appear causing tissue damage.12 These disorders are characterized by pain and phonation in the temporomandibular joint, pain in the masticatory and cervical muscles, headache (especially in the temporal zone when the patient wakes up in the morning), hypersensitive teeth and occasionally restriction of mouth opening.1 The identification of active bruxers at an early stage can prevent the development of craniomandibular disorders.13-17
The only way to diagnose the presence of current SB with absolute certainty is using Polysomnography (PSG) in a sleep laboratory.18 The greatest disadvantages of PSG are its high cost and its modification of the patient’s habitual sleeping environment, which means that sometimes the patient’s normal activity cycle is disrupted. For these reasons PSG is usually restricted to the diagnosis of complex cases (epilepsy, complex disorders of movement during sleep) and research purposes.4,19-20
In their daily practice dentists need simpler and more practical devices for SB diagnosis. Bruxcheckers (BCs) may become such devices (Figure 1). The BC is a polyvinyl chloride foil coated with red food colorant on one side (0,1 mm thickness). BC are fabricated in a vacuum press, where 0,1 mm thickness foil is heated at 230 C for 15 seconds and pressed over cast of the lower jaw using a vacuum forming device (e.g. Biostar from Scheu-Dental, Germany). Then the device is trimmed along the gingival margins. BC do not affect the activity of masticatory muscles as found in the electromyography test with BC and without them. In both cases muscle activity is the same.21 Combining descriptive and quantitative analysis of BC dental abrasion facets could help us to answer different questions: Do the dental abrasion facets increase in the stress period or not? Are they different in males and females? Is there a connection between the size of the dental abrasion facets and muscle pain? Answers to all these questions could help gain a better understanding of SB nature in individual cases, especially in stress situations.
 |
Figure 1: Brux Checkers.
|
Methods
The study was conducted in Sechenov First Moscow State Medical University, after the ethic vote was approved. Participation in the study was voluntary and demanded a written agreement of participants (informed consent). Ethical approval for performing the study was obtained from the ethical committee of I. M. Sechenov First Moscow State Medical University (proсess number 12). The study was initiated as a single group design. The same investigator performed all the examinations.
Participants
All the participants were third- and four-year students chosen at random. The total number of participants was 36 (25 females and 11 males). The inclusion criteria were: third and four-year dental students, males and females, signed informed consent, age range: ≥ 19 years, ≤ 26 years.
Participants have been rejected, if one of the following exclusion criteria was met: students undergoing dental treatment, more than 2 missing molars (excluding third molars), myorelaxation therapy in previous six months (e.g. myorelaxation splint or botulinum toxin injection), severe psychological disorders and/or the use of antipsychotic drugs, central or peripheral nervous system disorders.
Procedure
All the participants were examined according to Clinical Functional Analysis (CFA) 2 times in stress and non-stress periods. There were several visits during the research project. During PreStudy Visit the candidates for the participation in the research project received information about the study design, the purpose of the study and the conditions of participation. If a candidate decided to take part in the research, the informed consent was signed in two copies by the participant and the investigator. One copy stayed in the medical records in the dental clinic, the other one was given to the participant. In addition the candidates were checked according to the inclusion and exclusion criteria. One week after the participants were invited to Study Visit 1. During Study Visit 1 the first investigator filled the form about the participant’s (anonymous) identification, age and sex, then collected the information according to CFA (these were participants’ medical records, dental records, occlusion index (OI), muscle and jaw joint palpation results). Later portrait and intraoral photos were made, alginate impression was taken. After a clinical examination in dental laboratory, the dental technician made cast models and BC. 2-5 days after Study Visit 1 the participants were invited to Study Visit 2. During this appointment the investigator gave a set of two BC to each participant providing instructions. The participants were supposed to wear their BC one night for the upper jaw and next night for the lower jaw.
3 days after Study Visit 2 the participants were invited to Study Visit 3. After their use, the BC were placed into a special box with the participant’s name on it and the participants gave them back to the dental clinic. The investigator made the calculation of abraded facets area on BC. Study Visit 4 took place during the participants’ examination period (in the middle of the exam period at university). The investigator carried out the same examination using the same protocol. The participants also received a set of two BC, which were made in the dental lab previously. The participants were supposed to wear their «BCs» one night for the upper jaw and the next night for lower jaw. 3 days after Study Visit 4 the participants were invited to Study Visit 5 to give the BC back to the dental clinic where the investigator made the calculation of abraded facets area on BC.
Collection of Data
CFA
The protocol for CFA included
10 questions about the students’ current dental status (Figure 2)
 |
Figure 2: CFA – current status (OI questions) of the patient.
|
Students answered these questions and if the answer was positive – «Yes», they marked it from 1 to 3 depending on how concerned they were about this problem, with 1 being the minimum and 3 being the maximum. It the end we could calculate OI, which is the ratio of the number of questions to the number of positive answers. We analyzed both each question separately and the occlusal index in general.
12 questions about the students’ general medical status (Figure 3)
 |
Figure 3: CFA – medical history of the patient.
|
5 questions the students’ dental history and the psychic status (Figure 4)
 |
Figure 4: CFA – dental history and psychic status of the patient.
|
map of muscle and joint palpation (Figure 5)
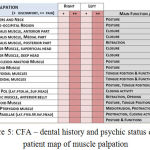 |
Figure 5: CFA – dental history and psychic status of the patient map of muscle palpation.
|
Muscle palpation was carried out bimanualy and symmetrically marking discomfort with + and pain with ++.
BCs
The research projects included two BC; one for the upper jaw, the other for the lower jaw. They were made twice for examination and non-examination periods. After they were used, there were photographed according to the protocol (Figure 6). For counting the abraded facets area the program “Universal desctopruler.exe” was used (Figure 7).
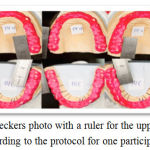 |
Figure 6: Brux Checkers photo with a ruler for the upper and lower jaw according to the protocol for one participant.
|
 |
Figure 7: Abrading facets counting process with the program «Adobe photoshop» and «Universal desctopruler.exe»
|
Statistical Analysis
All the data were included in the tables: the results from the non-stressed period were mentioned in Table 1, and the results from the stress period – in Table 2. Then all the data were processed with the help of the program “Statistica 8.0”
To determine the occlusal index and sensitivity during muscle palpation we need to use the ordinal scale, therefore for subsequent statistical processing, we applied the nonparametric Wilcoxon test to check for the presence of differences in coherent samples (in paired measurements).
Teeth abraded facets areas were measured against metric scale (mm²). However, the check of the normality distribution of the obtained results using graphical estimation methods and the Kolmogorov-Smirnov test revealed significant deviations in the distribution from the normal one. As a result, we refused to use Student’s parametric t-test for connected samples in favor of the nonparametric T-Wilcoxon test.
Results
OI
The first parameter we compared in the stress and non-stress period was the OI. The students showed a higher value of OI in the stress period than in the non-stress period, a=0,02 (Table 1). The difference was brought about by the dissimilarity in the evaluation given to OI Question 8 (OIQ8), a=0,007 and OI Question 9 (OIQ9), a=0,05.
Question 8: Do you suffer from headaches?
Question 9: Are there cramps in head/neck muscles?
There was no significant difference in the other questions.
Muscle Palpation
The next parameter compared was muscle palpation (Table 2). Significant differences were noted in case of the following indicators: shoulder and neck muscles on the right side and much less acute for temporalis muscle medial portion on the left side (3.3bL), a=0,01, temporalis muscle posterior portion on the right side (3.3cR),a=0,04, temporalis muscle posterior portion on the left side (3.3cL) a=0,04, masseter muscle deep head on the left side (3.4bL) a=0,03, lateral pole static on the left side (3.15aL), a=0,04.
Dental Measuring
The last parameter was dental measuring where we compared the square of abraded facets in the stress and non-stress period (Table 3). We supposed that the square of the facets on BC will increase in all teeth in the stress period. However, there only was a significant difference for abraded areas for teeth 15 (a=0,005), 34, 31 (a=0,05) and some tendencies for the abraded facets areas for teeth 24 and 33 (a=0,07).
Discussion
We expected the dental students to show an increase in the OI in Question 9 (OIQ9) in the stress period. SB can increase the risk of appearance of episodic migraine and episodic tension-type headache. We noted deep differences in the value of the following indicators: OI (sum), OI Q8, OI Q9. OI is defined as a sum of positive responses to OI questions. The students showed a higher value of OI (sum) in the stress period than in the non-stress period due to dissimilarity in the evaluation given to OI Question 8 (OIQ8) and OI Question 9 (OIQ9).
In our analysis we see that the stress situation can be a predisposing factor for headaches. Our findings about headaches are in line with G. Fernandes’s investigation. These are so called “stress headaches” (tension headache); they feel like a tightness in the forehead or back of the neck.22 Moreover, we see that our students also complain of cramps in head/neck muscles in the stress period. These findings correlate with the nature of stress, because as is known, stress and tension headaches go hand in hand. High mental stress provokes muscle tension and this is especially true of the neck muscles and shoulder muscles. There is no significant difference in the other questions.
Muscle pain in a stress situation is much more intense for several muscles. As follows from the research, the stress situation provokes muscle tension especially in the neck and shoulder region. T. Kampe described a strong correlation between bruxers and high values in the muscular tension scale and headache. Subjects with bruxism reported the aching neck, back, throat or shoulders.23
Nevertheless, in this analysis, despite our expectations there was no difference in the muscles which are responsible for grinding and clenching movements.
The last parameter was dental measuring where we compared the square of abraded facets in the stress and non-stress period. Contrary to our expectations, we did not see great differences in the size of the abraded facets during and without stress. But it was found that in the researched group of people the abraded area in the stress situation is much bigger for teeth 15 and 34 and much smaller for tooth 31. Besides, in the stress situation the abraded area of tooth 24 tends to increase, while the abraded area of tooth 33 tends to decrease.
There were no significant differences in the total area of the abraded facets in men and women in the studied sample. Differences in the total values of the abraded facets for the right and left side, and for the upper and lower jaw were not found.
As can be seen from the analysis, during the stress situation the abraded area shifted from frontal teeth to chewing teeth. So we can suppose that during the stress period brux episodes can occur more frequently and with a higher load. We suppose that grinding decreases, while clenching increases in a stress period, i.e. clenching pattern becomes more pronounced during the brux activity. Chewing teeth (premolars in our study) are more adapted and more useful for such a condition. That is why our students shift their brux behavior from 33 and 31 to 15 and 24.
Conclusion
In the study during the stress period the dental students demonstrated:
Significantly higher headaches in relation to the non-stress period;
Significantly higher cramps in head/neck muscles versus to the non-stress period;
Significantly much more intense muscle pain for the shoulder and neck muscles;
Significant shift of abraded facets from frontal teeth to chewing teeth in the stress situation.
In the future, more follow-up studies are needed for exploration of students’ brux behavior in the stress period. It may be interesting to use a professional questionnaire for stress assessment, such as Spilberger’s anxiety scale, which can help to define trait anxiety for each subject and state anxiety for the whole group. It will be helpful to divide students into different classes depending on trait anxiety and compare brux behavior in various trait anxiety groups.
Also to detail muscle activity, frequency and duration of brux episodes and correlation of the above-listed parameters with abraded facets, it will be interesting to use PSG records in combination with BC.
Acknowledgement
This research was conducted out without funding.
Conflict of Interest
The authors have stated explicitly that there no conflict of interests exists in connection with this article.
Funding Source
This research was conducted out without funding.
References
- American Academy of Sleep Medicine: International Classification of Sleep Disorders, Revised: Diagnostic and coding manual. American Academy of Sleep Medicine, Westchester. 2001.
- Leeuw R. D. Orofacial Pain. Guidelines for Assessment, Diagnosis and Management. Quintessence Publishing, Chicago. 2008.
- Kato T., Thie N. M., Huynh N., Miyawaki S., Lavigne G. J. Topical review sleep bruxism and the role of peripheral sensory influences. Journal of Orofacial Pain. 2003;17(3):191-213
- Lavigne G. J., Khoury S., Abe S., Yamaguchi T., Raphael K. Bruxism physiology and pathology: an overview for clinicians. Journal of Oral Rehabilitation. 2008;35:476-494.
CrossRef - International Statistical Classification of Diseases and Related Health Problems. World Health Organization, Geneva. 2008.
- Sato S., Slavicek R. Bruxism as a stress management function of the masticatory organ. The Bulletin of the Kanagawa Dental College. 2001;29:101-110.
- Cooper C. L. Job satisfaction, mental health, and job stressors among general dental practitioners in the UK. British Dental Journal. 1987;162(2):77-81.
CrossRef - Acharya S. Factors affecting stress among Indian dental students. Journal of Dental Education. 2003;67(10):1140-1148.
- Naeem A., Kiblawi M. A., Ahmad E., Samad S. A., Samad A. A., Naeem A., Chandershekhar S., Begum S., Kumar J. Comparison of daytime sleepiness in medical university students using the Epworth Sleepiness Scale (ESS). Psychology and Social Behavior Research. 2014;2(2):58-62.
CrossRef - Bahammam A. S., Alaseem A. M., Alzakri A. A., Almeneessier A. S., Sharif M. The relationship between sleep and wake habits and academic performance in medical students: a cross-sectional study. BMC Medical Education. 2012;1:61.
CrossRef - Alzaheml A. M., der Molen H. T. V., Alaujan A. H., Schmidt H. G., Zamakhshary M. H. Stress amongst dental students: a systematic review. European Journal of Dental Education. 2011;15:12-14.
- Lobbezoo F., Lavigne G. J. Do bruxism and temporomandibular disorders have a cause-and-effect relationship? Journal of Orofacial Pain. 1997;11:15-23.
- Negra J. M. S., Scarpelli A. C., Tersa-Costa D., Guimaraes F. H., Pordeus I. A., Paiva S. M. Sleep bruxism awake bruxism and sleep quality among Brazilian dental students: A cross sectional study. Brazilian Dental Journal. 2014;25(3):241-247.
CrossRef - selms M. K. A. V., Visscher C. M., Naeije M., Lobbezoo F. Bruxism and associated factors among dutch adolescents. Community Dentistry and Oral Epidemiology. 2013;41(4):353-363.
CrossRef - Molina O. F., Santos J. J., Mazzetto M. O., Nelson S. J., Nowlin T. A., Maineri ET: Oral jaw behaviors in TMD and bruxism a comparison study by severity of bruxism. Cranio the journal of craniomandibular practice. 2001;19(2):114-122.
CrossRef - Molina O. F., Santos J. J., Nelson S. J., Grossman E. Prevalence of modalities of headaches and bruxism among patients with craniomandibular disorders. Cranio: the journal of craniomandibular practice. 1997;15(4):14-25.
CrossRef - Molina O. F., Santos J. J., Nelson S. J., Nowlin T. A clinical study of specific signs and symptoms of CMD in bruxers classified by the degree of severity. Cranio: the journal of craniomandibular practice. 1997;17(4):268-279.
CrossRef - Koyano K., Tsukiyama Y., Ichiki R., Kuwata T. Assessment of bruxism in the clinic. Journal of Oral Rehabilitation. 2008;35(7):495-508.
CrossRef - Velly-Miguel A. M., Montplaisir J., Rompre P. H., Lund J. P., Lavigne G. L. Bruxism and other orofacial movements during sleep. Journal of Craniomandibular Disorders: Facial & Oral Pain. 1992;6:71-81.
- Lavigne G. J., Khoury S., Abe S., Yamaguchi T., Raphael K. Drugs and bruxism: a critical review. Journal of Orofacial Pain. 2003;17:99-111.
- Onodera K., Kawagoe T., Sasaguri K., Protacio-Quismundo C., Sato S. The use of a BruxChecker in the evaluation of different grinding patterns during sleep bruxism. Cranio: the journal of craniomandibular practice. 2006;24(4):292-299.
CrossRef - Fernandes G., Franco A. L., Gonçalves D. A., Speciali J. G., Bigal M. E., Camparis C. M. Temporomandibular disorders, sleep bruxism, and primary headaches are mutually associated. Journal of Orofacial Pain. 2013;27(1):14-20
- Kampe T., Edman G., Bader G., Tagdae T., Karlsson S. Personality traits in a group of subjects with long-standing bruxing behaviour. Journal of Oral Rehabilitation. 1997;24:588-593.
CrossRef







