Praveen Panchaksharimath1 , Praveen A. N2
, Praveen A. N2 and Manjunath R3
and Manjunath R3
1Department of Pharmacology, Bangalore Medical College and Research Institute (BMC and RI), Bengaluru, India.
2Department of Pharmacology, BMC and RI, Bengaluru, India.
3Department of Cardiology, Super speciality hospital (PMSSY) BMC and RI, Bengaluru, India.
Corresponding Author E-mail: praveengowdadr@yahoo.com
DOI : https://dx.doi.org/10.13005/bpj/1570
Abstract
Drug utilization study is a powerful exploratory tool to evaluate the present trends of drug prescribing and appropriateness of prescription. To analyse the age and gender related differences in utilization of different classes of drugs in patients for Ischemic heart disease (IHD) management. This cross-sectional observational study was conducted from August 2017 to March 2018 in Cardiology department, PMSSY, BMC&RI, Bengaluru. The demographic, and drug prescription data of IHD patients were analyzed according to age group (18–59 years versus ≥ 60 years) and gender wise. Out of 520 patients diagnosed with IHD, 68% were male patients and 60% were aged ≥ 60 years. The most common co-morbid condition was Hypertension (66%) and was significant in patients aged ≥ 60 years (P= 0.0033). Anti-platelet drugs (100%) followed by Lipid lowering drugs (96%) were most commonly prescribed. The average number of drugs per prescription was found to be 6.44. Prescription of Dual anti-platelet therapy was found to be significant among men (<0.0001). Prescription of Diuretics (p = 0.045) and Pregabalin (p = 0.031) were significantly higher among females and Prescription of Angiotensin receptor blockers (ARBs) was significantly higher among those aged 18–59 years. Hypertension and Diabetes Mellitus were the most common co-morbidities observed with IHD. ARBs, Diuretics, Proton pump inhibitors, Anti Diabetic Agents and Pregabalin showed significant differences in the drug utilization with respect to age and gender. Dual anti-platelet therapy was observed to be significantly higher among males. This study has been registered in CTRI (CTRI/2018/05/013949).
Keywords
Angiotensin Receptor Blockers; Anti-Platelets; Drug Utilization; Hypertension; Ischemic Heart Disease
Download this article as:| Copy the following to cite this article: Panchaksharimath P, Praveen A. N, Manjunath R. A Cross-Sectional Study to Evaluate Age and Gender Related Differences in Drug Utilization in Ischemic Heart Disease at A Tertiary Care Hospital. Biomed Pharmacol J 2018;11(4). |
| Copy the following to cite this URL: Panchaksharimath P, Praveen A. N, Manjunath R. A Cross-Sectional Study to Evaluate Age and Gender Related Differences in Drug Utilization in Ischemic Heart Disease at A Tertiary Care Hospital. Biomed Pharmacol J 2018;11(4). Available from: http://biomedpharmajournal.org/?p=23569 |
Introduction
World Health Organization (WHO) defines Drug utilization research as the marketing, distribution, prescription and use of drugs in a society, with special emphasis on the resulting medical, social and economic consequences.1 It is a powerful exploratory tool to evaluate the present prescribing trends of drug use and to check the appropriateness of prescription. It helps in the management of drug specific problems thereby improving medication quality and patient safety.
Ischemic heart disease (IHD) is a condition in which there is an inadequate supply of blood and oxygen to a portion of the myocardium; it occurs due to an imbalance between myocardial oxygen supply and demand.2 IHD causes about 7.4 million global deaths every year. Changing life style in developing countries like India has enormously increased the statistical figures of diseases. In India, IHD caused 306.3 & 372.8 deaths per 1 lakh population in males & females respectively.3
Men are more likely to suffer from angina pectoris and myocardial infarction at an early age as compared to women.4,5 Co-morbidities associated with IHD and prescription of Hypolipidemics and Anti-hypertensives are observed to be more among men as compared to women.6
Aims and Objectives
To analyze the age and gender related differences in utilization of different classes of drugs in out-patients for Ischemic heart disease management.
Materials and Methods
The study was conducted between August 2017 to March 2018 at Cardiology department, Super-speciality hospital (PMSSY) attached to BMC&RI, Bengaluru among 520 out-patients diagnosed with IHD.
Study design – Cross-sectional observational study.
After obtaining clearance and approval from the Institutional Ethics Committee, the out-patients diagnosed with IHD by the cardiologist, of either gender aged >18 years and willing to give written informed consent were included and patients diagnosed with other than IHD as their primary diagnosis were excluded from the study.
Their demographic data, history, clinical examination findings and reports of various investigations of every out-patient with IHD were recorded. The relevant data on drug prescription like number of drugs, dosage form, dose, route, time of administration, duration and frequency of drugs prescribed to each patient was recorded.
Drugs were classified based on WHO’s Anatomic Therapeutic Chemical (ATC) classification system. They were divided into groups based on Anatomical main group (1st level), Therapeutic, Pharmacological and Chemical characteristics (2nd, 3rd and 4th levels). The total number of drugs, cardiovascular drugs and non-cardiovascular drugs prescribed per person was noted. The age and gender related differences were analyzed based on the prescription of cardiovascular drugs and non-cardiovascular drugs. The characteristics of IHD patients was analysed to identify potential factors affecting utilization of cardiovascular drug classes.
Data was analysed according to Age (18–59 years versus ≥ 60 years) and Gender (male versus female) and stratified according to age in gender (male [18–59 years versus ≥ 60 years] and female [18–59 years versus ≥ 60 years]). Number of drugs prescribed (≤ 5 drugs and > 5 drugs) and duration of treatment (< 1 year, 1 – 5 years and > 5 years) was also analysed.
Statistical Analysis
The descriptive data in this study was analysed using mean, Standard deviation, percentage and proportions. Chi square test and Mann-Whitney U test was appropriately used to compare characteristics between the genders (male versus female), and between the age groups (18 – 59 years versus ≥ 60 years). A p-value of < 0.05 was considered to be statistically significant.
Results
Out of 520 patients diagnosed with IHD, 354 (68%) were males and 166 (32%) were females, 259 (50%) were of the age group of 18 – 59 years and 261 (50%) were of ≥ 60 years. Among 354 males, 182 (51.4%) were between 18 – 59 years and 172 (48.5%) were ≥ 60 years. Among 166 females, 77 (46.3%) were 18 – 59 years and 89 (53.6%) were ≥ 60 years old. The average age of patients was 57.7 ± 11.6 years. The average number of drugs per prescription was found to be 6.44. The average duration of treatment was 3.87±4.07 years. (Table 1).
Table 1: Baseline characteristics.
| Total number of patients with IHD | 520 |
| Age (Years) | 57.7±11.6 |
| Males | 354 (68%) |
| Females | 166 (32%) |
| 18 – 59 years | 259 (50%) |
| ≥ 60 years | 261 (50%) |
| Hypertension | 344(66%) |
| Type 2 Diabetes Mellitus | 182 (35%) |
| Total number of drugs prescribed | 3349 |
| Average number of drugs per patient | 6.44±1.63 |
| Average duration of treatment (years) | 3.87±4.07 |
The most common co-morbid conditions were Hypertension (HTN) observed in 344(66%) patients followed by Type 2 Diabetes Mellitus (T2DM) observed in 182 (35%) patients and were significantly higher among patients aged ≥ 60 years (p = 0.0001) and among males aged ≥ 60 years (p = 0.01). (Table 2).
Table 2: Distribution of Hypertension and Diabetes according to Age and Gender.
| Comorbidity | Gender | Age (years) | Male | Female | ||||
| Male (354) | Female (166) | 18–59 (259) | ≥ 60 (261) | 18–59 (182) | ≥ 60 (172) | 18–59 (77) | ≥ 60 (89) | |
| Hypertension | 231
(65.2%) |
113
(68%) |
155*
(59.8%) |
189 *
(72.4%) |
103*
(56.5%) |
128*
(74.4%) |
52
(67.5%) |
61
(68.5%) |
| p value | 0.59 | 0.0033 | 0.0006 | 0.88 | ||||
| Diabetes Mellitus | 117
(33%) |
65
(39.1%) |
69*
(26.6%) |
113*
(43.2%) |
40*
(21.9%) |
77*
(44.7%) |
29
(37.6%) |
36
(40.4%) |
| p value | 0.20 | <0.0001 | <0.0001 | 0.84 |
Chi square test was used for analysis
* Statistically significant
Anti-platelet drugs were prescribed to all patients followed by Lipid modifying agents (96%), Beta Blockers (84%), Angiotensin Converting Enzyme Inhibitors (ACE-I) (46%), Diuretics (40%), Angiotensin Receptor Blockers (ARBs) (34%), Anti-Diabetic Agents (28%), Calcium Channel Blockers (CCBs) (25%), Proton pump inhibitors (PPIs) (22%) and Anti-anginal drugs (20%). (Figure 1) (Table 3).
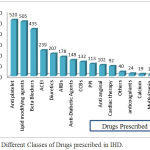 |
Figure 1: Different Classes of Drugs prescribed in IHD.
|
Table 3: Drug Utilization patterns, according to Age and Gender.
| Drug prescribed | ATC code | Gender | Age (years) | Male | Female | |||||
| Male
354 (%) |
Female
166 (%) |
18–59
259 (%) |
≥ 60
261 (%) |
18–59
182 (%) |
≥ 60
172 (%) |
18–59
77 (%) |
≥ 60
89 (%) |
|||
| Cardiovascular Drugs | ||||||||||
| Antiplatelets | B01 | 354 (100) | 166 (100) | 259 (100) | 261 (100) | 182 (100) | 172 (100) | 77 (100) | 89 (100) | |
| Lipid modifying agents | C10 | 342 (96.6) | 163 (98.1) | 250 (96.5) | 255 (97.7) | 176 (96.7) | 166 (96.5) | 74 (96.1) | 89 (100) | |
| Beta blockers | C07 | 294
(83.0) |
141
(84.9) |
221
(85.3) |
214
(81.9) |
156
(85.7) |
138
(80.2) |
65
(84.4) |
76
(85.3) |
|
| CCBs | C08 | 83(23.4) | 49(29.5) | 59(22.7) | 73(27.1) | 35(19.2) | 48(27.9) | 24(31.1) | 25(28) | |
| ACE-I | C09 | 163(46) | 76(45.7) | 119 (45.9) | 120 (45.9) | 89(48.9) | 74(43) | 30(38.9) | 46(51.6) | |
| ARBs | C09 | 116
(32.7) |
62
(37.3) |
87
(33.5)* |
61
(23.3)* |
54(29.6) | 62(86.1) | 33(42.8) | 29(32.5) | |
| Anti anginal | C01 | 71(20) | 31(18.6) | 47(18.1) | 55(21) | 35(19.2) | 36(20.9) | 12(15.5) | 19(21.3) | |
| Diuretics | C03 | 130
(36.7)* |
77
(46.3)* |
101
(38.9) |
106
(40.6) |
62(34.0) | 68(39.5) | 39(50.6) | 38(42.6) | |
| Non Cardiovascular Drugs | ||||||||||
| PPI | A02 | 77(21.7) | 36(21.6) | 55(21.2) | 58(22.2) | 44(24.1) | 33(19.1) | 11 (14.2)* | 25(28)* | |
| Anti Diabetic agents | A10 | 97(27.4) | 51(30.7) | 55(21.2)* | 93(35.6)* | 33(18.1)* | 64(37.2)* | 22(28.5) | 29(32.5) | |
| Nutraceuticals | A12 | 19(5.3) | 15(9) | 19(7.3) | 15(5.7) | 11(6) | 8(4.6) | 8(10.3) | 7(7.8) | |
| Pregabalin | N03 | 14(3.9)* | 15(9)* | 13(5) | 16(6.1) | 5(2.7) | 9(5.23) | 7(9) | 8(8.9) | |
Chi square test was used for analysis. * Statistically significant ( p < 0.05)
ATC – Anatomic Therapeutic Chemical classification system, CCBs – Calcium Channel Blockers, ACE-I – Angiotensin Converting Enzyme Inhibitors, ARBs -Angiotensin Receptor Blockers, PPI – Proton pump inhibitors
Number of drugs prescribed (≤ 5 drugs and > 5 drugs) was analyzed according to age and gender but no significant difference was observed. (Table 4) Duration of treatment of IHD (< 1 year, 1 – 5 years and > 5 years) showed a significant difference among the age groups (p = 0.0066). (Table 5).
Table 4: Differences in number of drug prescription, according to Age and Gender.
| Parameter | All | ≤5 Drugs | >5 Drugs | p – value |
| Gender | Male | 112 | 242 | 0.42 |
| Female | 46 | 120 | ||
| Age | 18–59 yrs | 85 | 188 | 0.76 |
| ≥ 60 yrs | 73 | 174 | ||
| Gender by age | ||||
| Male | 18–59 yrs | 62 | 120 | 0.37 |
| ≥ 60 yrs | 50 | 122 | ||
| Female | 18–59 yrs | 23 | 54 | 0.68 |
| ≥ 60 yrs | 23 | 66 |
Chi square test was used for analysis
Table 5. Duration of IHD according to Age and Gender.
| Duration of IHD | Patients (520) | Male (354) | Female (166) | 18–59 (259) | ≥ 60 (261) |
| ≤ 1 year | 142 | 108 | 36 | 99 | 45 |
| 1-5 years | 266 | 174 | 92 | 139 | 127 |
| >5 years | 110 | 72 | 38 | 21 | 89 |
| p – value | 0.11 | 0.0066* |
Chi square test was used for analysis. * Statistically significant (p < 0.05).
Out of 3349 (6.44±1.63) drugs prescribed, 2878 (5.53±1.31) were cardiovascular drugs and 471 (0.9±1.03) were non-cardiovascular drugs (Table 6) and we observed a significant difference in prescription of Cardiovascular and non-cardiovascular drugs with respect to age and gender (p < 0.0001).
Table 6: Differences in the prescription of cardiovascular and non-cardiovascular drugs, according to Age and Gender.
| Cardiovascular Drugs | p value | Non-Cardiovascular Drugs | p value | |
| n = 2878 | n = 471 | |||
| Mean± SD | Mean± SD | |||
| Gender | ||||
| Male (354) | 5.53±1.31 | 0.8336 # | 0.90±1.03 | 0.3575 $ |
| Female (166) | 5.53±1.30 | 0.89±1.03 | ||
| Age | ||||
| 18–59 yrs (259) | 5.52±1.31 | 0.6599 # | 0.89±1.03 | 0.0278 *$ |
| ≥ 60 yrs (261) | 5.53±1.31 | 0.90±1.03 | ||
| Age by Gender | ||||
| Male | ||||
| 18–59 yrs | 5.59±1.40 | 0.3734 # | 0.78±1.00 | 0.0574 $ |
| ≥ 60 yrs | 5.44±1.24 | 0.97±1.02 | ||
| Female | ||||
| 18–59 yrs | 5.50±1.27 | 0.61 # | 0.93±1.18 | 0.3125 $ |
| ≥ 60 yrs | 5.60±1.32 | 1.01±0.98 |
* Statistically significant (p < 0.05). # Chi square test was used for analysis. $ Mann-Whitney U test was used for analysis.
In our study, age and gender related differences was not observed in β-blockers, ACEIs and CCBs. Prescription of Diuretics (p = 0.045) and Pregabalin (p = 0.031) were significantly higher among females. Prescription of ARBs were significantly higher among those aged 18–59 years (p = 0.012) and PPIs was significantly higher among those aged ≥ 60 years (p = 0.049). Anti Diabetic agents prescription was significantly higher among those aged ≥ 60 years (p = 0.033) and in male patients aged ≥ 60 years. Among the anti-platelets prescribed, dual anti-platelet therapy was found to be significantly higher among males (p < 0.0001). (Table 7).
Table 7. Anti-platelets prescription according to Age and Gender.
| Antiplatelet (n = 520) | Male (354) | Female (166) | 18–59 (259) | ≥ 60 (261) | Male | Female | ||
| 18–59 (182) | ≥ 60 (172) | 18–59 (77) | ≥ 60 (89) | |||||
| Single | 138 | 99 | 113 | 124 | 63 | 75 | 50 | 49 |
| Dual | 217 | 66 | 146 | 137 | 120 | 97 | 26 | 40 |
| p | <0.0001* | 0.423 | 0.096 | 0.21 | ||||
Chi square test test was used for analysis. * Statistically significant (p < 0.05).
There was a significant difference in prescription of Cardiovascular drugs when compared to non-cardiovascular drugs with respect to age and gender (p < 0.0001) (Table 8).
Table 8: Prescription of Cardiovascular and non-cardiovascular drugs according to Age and Gender.
| Patients (520) | 18–59 years (259) | ≥ 60 years (261) | Male (354) | Female (166) | |
| CV Drugs (n = 2878) | 5.53 | 5.53 | 5.53 | 5.53 | 5.53 |
| Non CV Drugs (n = 471) | 0.91 | 0.90 | 0.90 | 0.91 | 0.89 |
| p value | <0.0001* | <0.0001* | <0.0001* | 0.0088* | 0.0088* |
Unpaired t-test test was used for analysis. * Statistically significant (p < 0.05).
Discussion
This study was aimed at identifying age and gender related differences in drug use among patients with IHD along with co-morbid illness. Drug prescribing practices will aid in drug procurement and provide feedback to treating physician in rational prescribing.
During the study period, among 520 prescriptions, male preponderance (60%) was observed and was in accordance with other studies,3,7,8,9 indicating that IHD is slightly more prevalent in males. Higher incidence of HTN and T2DM among men, may have contributed to higher prevalence of IHD in our study.
Among the co-morbid illness, age and gender differences were noted in the prevalence of HTN and T2DM as it was significantly greater among males patients aged ≥ 60 years. Therefore utilization of Anti-diabetics followed the same trend as Anti-hypertensives.
In our study we observed that HTN was the most common co-morbidity and significantly higher among patients aged ≥ 60 years (p = 0.0003) and males aged ≥ 60 years (p = 0.0006) which was in accordance with previous studies.3,7,8,9
Shruthi D et al3 in her study observed Type 2 Diabetes Mellitus in 38% patients with IHD similar to our study (38%). Hence Anti Diabetic agents prescription was significantly higher among those aged ≥ 60 years (p = 0.033) and in male patients aged ≥ 60 years.
The mean age was 57.7 years similar to study conducted by Zachariah et al.9 with 56.9 years. Very little difference in the two age groups was noted which was similar to study conducted by Kunnoor N et al.7
In our study, for the treatment of IHD, various cardiovascular drugs namely Anti-platelet drugs, Anticoagulants, Anti-anginal drugs, Lipid modifying agents, β -blockers, Angiotensin converting enzyme inhibitors (ACEIs), Angiotensin II receptor blockers (ARBs), Calcium channel blockers (CCBs), Diuretics, and non – cardiovascular drugs – Anti Diabetic agents, Proton Pump Inhibitors, calcium, Pregabalin, Iron preparations, Nutraceuticals were prescribed.
Most of the drugs prescribed in our study were in accordance with AHA/ACC guidelines for treatment of stable IHD. In our study the commonly prescribed drugs were Aspirin among Anti-platelet drugs, Atorvastatin among Lipid lowering drugs, Ramipril among ACEIs, Telmisartan among ARBs, Metoprolol among β-blockers and Amlodipine among CCBs and these drugs were freely available in our hospital pharmacy.
In our study higher rates of utilization of Anti-platelet drugs and Lipid lowering drugs were observed irrespective of age and gender which was similar to previous studies.3,10
Dual Anti-platelet Therapy (DAPT) prescription was found to be significantly higher among males (<0.0001) which was contradictory to results obtained by Jyothi et al in a retrospective study conducted among IHD patients and observed that females were more commonly prescribed.11 DAPT was more effective than aspirin monotherapy in reducing ischemic events (7.3% DAPT vs. 8.8% aspirin, p = 0.01) among IHD patients, at the cost of increased bleeding (2.0% DAPT patients vs. 1.3% aspirin patients, p=0.004) which was observed in a study conducted by Bhatt DL et al.12
There was a significant difference in prescription of Cardiovascular and non-cardiovascular drugs with respect to age and gender (p < 0.0001) this difference was not observed in study conducted by Kunnoor N et al.7
Prescription of Diuretics (P=0.045) was significantly higher among females, but this observation did not correlate with the study done by Kunnoor N et al.7 In our study, higher rates of utilization of Diuretics may be due to higher rates of heart failure among females but this data was not recorded and it was one of the limitations of our study.
The utilization of ACEIs and ARBs in male patients was not significantly different from their use in female patients (46% vs. 45.7%; p = 1 and 32.7 vs. 37.5; p = 0.35 respectively) similar to the study done by Kunnoor N et al. (7) Prescription of Angiotensin receptor blockers was significantly higher among those aged 18–59 years (p = 0.012). Use of ACEIs has beneficial effects against Fibrosis and cardiac remodelling thereby decreasing morbidity and mortality in IHD.
In our study there was no significant difference in Utilization of β-blockers with respect to age and gender. Metoprolol was the most commonly prescribed beta blocker followed by Carvedilol. Kunnoor N et al.7 observed a significant higher prescription of β-blockers (p = 0.015) among patients aged 18 – 59 years and those aged ≥ 60 years.
Kunnoor N et al. observed a significantly higher use of CCBs in male patients aged ≥ 60 years similar difference was observed in our study but it was not statistically significant (p = 0.07 ). The 2011 NICE guidelines recommend use of CCBs in patients aged ≥ 55 years and ACE-Is in patients aged < 55 years.13
In our study there were no age and gender differences in Utilization of Anti-anginal drugs (Vasodilators) similar to the study done by Kunnoor N et al.7
Differences in number of drugs per prescription (≤ 5 and > 5) were analyzed according to age and gender but the difference was not statistically significant.
No differences in the prescription of cardiovascular drugs were observed with respect to age and gender. A significant difference in the prescription of Non – Cardiovascular drugs was observed between patients aged 18 – 59 years and groups similar to study by Kunnoor N et al.7
Patients were stratified into 3 groups based on the duration of IHD i.e., < 1 year , 1 – 5 years and > 5 years and we observed a significant differences between the groups (p = 0.0066) among patient aged > 60 years.
Strengths – This is one of the few studies conducted to analyze age and gender related differences in IHD. The findings of the present study clearly highlight the need for patient age to be taken into consideration when initiating pharmacotherapy for IHD, especially among outpatients who consume drugs for life long.
Limitations – Associated indications like Heart failure and Left ventricular dysfunction was not considered. Other modifiable risk factors like smoking, obesity, lifestyle and lipid profile of the patient was also not taken into consideration during assessment in our study. A prospective study with larger sample sizes among inpatients and adequate data on Adverse Drug Reactions monitoring is recommended to accurately estimate the age and gender-related differences in drug use in IHD at a tertiary care setting. The result of this study cannot be generalized since the study was conducted in a super-specialty set up of a tertiary care hospital among homogenous population.
Conclusion
HTN and DM were the most common co- morbidities observed with IHD. ARBs, Diuretics, PPI, ADAs and Pregabalin showed significant differences in the drug utilisation with respect to age and gender. Dual anti-platelet therapy was observed to be significantly higher among males.
Conflict of Interest
There is no conflict of interest
Funding Source
There is no funding source
Acknowledgment
Informed consent was taken from all the patients who were part of this study.
References
- Introduction to Drug Utilization Research: Chapter 1: What is drug utilization research and why is it needed?: 1.1. Definition and domains [Internet]. WHO.int. [cited 3 September 2016]. Available from: http://who.int/medicinedocs/en/d/Js4876e/2. 2016
- Elliott M. A., Loscalzo J . Ischemic Heart Disease. In Fauci S. A., Bruanwald E., Kasper L. D., Hauser L. S., Longo L. D., Jameson L. J et al., editors. Harrison’s principles of internal medicine . New York: The McGraw-Hill companies. Inc. 2015;2:1578.
- Dawalji S., Venkateshwarlu K., Thota S., Venisetty P. K., Venisetty R. K. Prescribing Pattern in Coronary Artery Disease: A Prospective Study. Intl Journal of Pharma Research & Review. 2014;3(3):24-33.
- Anand S. S., Islam S., Rosengren A., Franzosi M. G., Steyn K., Yusufali A. H., et al. Risk factors for myocardial infarction in women and men: insights from the INTERHEART study. European Heart Journal. 200819;29(7):932–40.
- Towfighi A., Zheng L., Ovbiagele B. Sex-specific trends in midlife coronary heart disease risk and prevalence. Archives of Internal Medicine. 2009;169(19):1762–1766.
CrossRef - Cardiovascular diseases (CVDs) [Internet]. World Health Organization. 2016 [cited 3 September 2016]. Available from: http://www.who.int/mediacentre/factsheets/fs317/en.
- Kunnoor N., Devi P., Kamath D., Anthony N., George J. Age- and gender-related differences in drug utilisation and adverse drug reaction patterns among patients in a coronary care unit. Singapore Med J. 2014;55(4): 221-228.
CrossRef - Narwane D. S. P. Prescription Pattern in Patients of Acute Coronary Syndrome in a Rural Tertiary Care Centre of Maharashtra. Journal of Medical Science And Clinical Research [Internet]. 2017;5(10):31 [cited 2018 Mar 2] CrossRef
- Zachariah T. G. K. S., Kempaller M. P. V. J. Drug utilization study in Ischaemic Heart Disease in a tertiary care hospital Mangalore India. International Journal of Basic & Clinical Pharmacology. 2017;6(7):1799.
CrossRef - Ruijter D. W., Waal D. M. W., Gussekloo J., Assendelft W. J., Blom J. W. Time trends in preventive drug treatment after myocardial infarction in older patients. British Journal of General Practice. 2010;60(570):47–9.
CrossRef - Jyothi K., Saleem T. M., Vineela L., Gopinath C., Reddy K. Y. A Retrospective Drug Utilization Study of Antiplatelet Drugs in Patients with Ischemic Heart Disease. age. 2015;60:80.
- Bhatt D. L., Flather M. D., Hacke W., et al. Patients with prior myocardial infarction, stroke or symptomatic peripheral arterial disease in the CHARISMA trial. J Am Coll Cardiol. 2007;49(1)1982-8.
CrossRef - Sulthan M. A., Mohammed M., Farhat F., Aziz S. A. Pharmacy Practice & Drug Research. 2007;140(159):90–99. hypertension.








