Vinishdharma Thenarasu1, Deepa Gurunathan2 and Kathiravan Selvarasu3
1Saveetha Dental College, Saveetha Institute of Medical and Technical Science (SIMATS) Saveetha University, Chennai, India.
2Department of Pedodontics Saveetha Dental College, Saveetha Institute of Medical and Technical Science (SIMATS) Saveetha University, Chennai, India.
3Department of Oral and Maxillofacial Surgery Saveetha Dental College, Saveetha Institute of Medical and Technical Science(SIMATS) Saveetha University, Chennai, India.
Corresponding Author E-mail: drgdeepa@yahoo.co.in
DOI : https://dx.doi.org/10.13005/bpj/1539
Abstract
Extraction of teeth has been a common, routine dental procedure done in clinics which may lead to moderate to severe pain postoperatively. Any pain postoperatively may cause a discomfort in particpants and affects their routine lifestyle. Preemptive analgesics plays an important role in reducing postoperative pain and distress associated with painful dental procedures. Nonsteroidal anti-inflammatory drugs are one of the treatment options to be used as pain relief for surgical teeth extraction. Wherelse, another commonly prescribed drug over-the-counter is Paracetamol. The purpose of this study is to evaluate the analgesic effect of both the drug as an preemptive analgesia. This study is a double blind , clinical trial. Twenty particpants were randomised into two group. Group A receiving Paracetamol (500mg) and Group B receiving Diclofenac (100mg) orally, 30 minute before the extraction is done. The pain intensity and the duration of the analgesia is evaluated using the Visual Analog Scale (VAS). Patient who were given Diclofenac (100mg) show a higher analgesic effect compare to Paracetamol (500mg).However, the analgesic effect in patient received Diclofenac is much more longer then patient received Paracetemol. Two different drug has been used in this study to evaluate their efficacy as an preemptive analgesic and it can be concluded that Diclofenac is more effective then Paracetamol as an preemptive analgesia.
Keywords
Dental Pain; Diclofenac; Extraction; Paracetamol; Preemptive Analgesia
Download this article as:| Copy the following to cite this article: Thenarasu V, Gurunathan D, Selvarasu K. Comparison of Efficacy of Diclofenac And Paracetamol as Preemptive Analgesic Agent. Biomed Pharmacol J 2018;11(3). |
| Copy the following to cite this URL: Thenarasu V, Gurunathan D, Selvarasu K. Comparison of Efficacy of Diclofenac And Paracetamol as Preemptive Analgesic Agent. Biomed Pharmacol J 2018;11(3). Available from: http://biomedpharmajournal.org/?p=22304 |
Introduction
Preemptive analgesia also called preoperative analgesia is a way of reducing or preventing the production of mediators responsible for nervous stimulation.1 It is characterized as an antinociceptive treatment for the prevention of central changes induced by afferent sensitization due to tissue injury caused by surgical procedures. Various method of achieving preemptive analgesia have been employed, this includes the infiltration of long acting local anaesthesia, nerve block, epidural block, intravenous analgesics and anti inflammatory drugs.2
Surgical extraction of tooth is a procedure which is usually relatively straight forward, and the vast majority of the extraction can be performed quickly while the individual is awake by using local anaesthesia injections to eliminate painful sensations. However, patient starts experiencing pain once the effect of local anesthesia fades off within few hours after extraction in which the pain is controlled by prescribed medication. Pain associated with surgical removal of tooth is experienced between moderate and severe during the first twenty four hours after surgery, with pain raising in 3 to 6 hours following conventional local anesthetic is used.3 Surgical dental extraction are usually associated with a trauma to both the soft and hard tissues. This trauma is often accompanied with pain and swelling.4 Tissue injury leads to the release of chemical mediators like histamine, serotonin, kinins, and prostaglandins, directly related to the inception and evolution of algic and inflammatory processes. Though inflammatory response is intrinsic to the tissue repairing process. its influence can be negative when the response is too intense. Hence it is essential to keep inflammatory response intensity under control to promote rapid healing and with less discomfort to the patient.
Nonsteroidal anti-inflammatory drugs are one of the treatment options to be used as pain relief for surgical teeth extraction. By administering the pre-operative analgesics, the postoperative pain intensity can be subsided and delayed as a result of the reduction in the amount of pain triggers (prostaglandins) discharged into the site of the injuries.5 Accumulation of prostaglandins released from the injured tissues increased by the time leading to the amplification of the pain intensity.6 Since dental pain is largely inflammatory, nonsteroidal anti-inflammatory drugs (NSAIDs) are the best analgesics for dental pain.7 The analgesic, anti-inflammatory, and antipyretic effects of NSAIDs are a result of their ability to inhibit cyclo-oxygenase (COX) enzymes, which catalyze the conversion of arachidonic acid to prostaglandins, that cause of pain, increase in temperature, and inflammation.8
One of the commonly prescribed NSAID is diclofenac that possesses analgesic, anti-inflammatory, and antipyretic properties. Diclofenac is effective in treating acute, chronic pain and inflammatory conditions It shows good pain control and has good analgesic effectiveness after extraction.9 The name diclofenac is derived from its chemical name ‘Dichloronilino phenylacetic acid. Diclofenac was first synthesized as Voltaren by Ciba-Geigy in 1973 that causes an inhibition of prostaglandin synthesis by inhibiting COX-1 and COX-2 with relative equipotency.10,11
Another commonly prescribed drug over-the-counter is Paracetamol which is also known as acetaminophenol. The chemical name for paracetamol is N-acetyl-p-aminophenol. Paracetamol is usually used for pain reliever and for treating fever as it has both analgesic (pain reliever) and antipyretic (fever reducer) effect.12 Though paracetamol is used to treat inflammatory pain, because it exhibits only weak anti-inflammatory activity ,it is not generally classified as an NSAID as it is classified as a mild analgesic. The mechanism of action involved is the inhibition of cyclooxygenase (COX) in the brain, which is highly selective for COX-2.13 Due to the raise of peroxides present in inflammatory lesion, the peripheral anti-inflammatory activity is lesser. However Paracetamol has analgesic and antipyretic properties similar to those of other NSAIDs.
The aim of the present study is to evaluate the efficacy of diclofenal compare to paracetamol as an preemptive analgesia after extraction of tooth.
Materials and Methods
Interventions
This study was conducted in Saveetha Dental College following approval from Institutional Ethical Board. 20 particpants were randomly included in the study who had to undergo extraction of teeth without any surgical complication. The selection criteria of particpants for this study included patient who are systemically healthy and willing to participate in this study. Particpants with known systemic illness, recent antibiotic or analgesic treatment history, allergy to NSAIDs, pregnant particpants and particpants with peptic ulcers are excluded from these study as it can effect the result of the study. Benefits and risks of the research was explained to the particpants and written informed consent was obtained .These 20 particpants are selected and randomized into two treatment group with 10 patient in each group (Group A and Group B).
Group A particpants were given Paracatemol (500mg) and group B particpants were given Diclofenac (100mg). The doses of Paracatemol and Diclofenac were based on their use in literature following extraction. The patient was administered with either of the drug orally 30 minutes prior to the extraction. Anesthesia was obtained by using 2mL cartridges of 2% lignoocaine containing 1:200,000 adrenaline. Additional local anesthesia was used when particpants had pain during surgery. Once local anesthesia was obtained, surgery was started and the tooth was extracted.
Assessments
The duration of analgesia of the administered drugs before surgery was evaluated as the time from the end of the surgery until the intake of the first rescue analgesic medication became necessary for the patient. A 10-mm visual analog scale (VAS) was used to asesss pain. The VAS consisted of an interval scale ranging from 0, representing no pain or discomfort, to 10, representing maximum pain or discomfort. Clinical assessments were done using the VAS at 10 minutes, 1 hour, 3 hours, and 6 hours after surgery. The patient were given a copy of VAS for the assessment of pain for 1 hour, 3 hours and 6 hours. The patient were instructed to take the rescue analgesic medication at least 6 hours apart. The duration of which the rescue analgesic medication taken is recorded. Their pain intensity and the intake of rescue medication is recorded and analysed to evaluate the analgesic effect of each drug. The data collected were extracted and tabulated in MS excel. Data management and statistical analysis were performed using the Statistical Package for Social Sciences (SPSS) software. Frequencies and percentages were calculated and result is obtained.
Result
A total number of 20 patient were selected randomly for this study. Patient who were given Diclofenac (100mg) show a higher analgesic effect compare to Paracetamol (500mg). Patient taking 1st rescue analgesic at the time interval of 3 hour is more in patient received paracatemol. Wherelse the number of patient took 1st rescue analgesic at 6 hours is more in patient received Diclofenac. This shows that the analgesic effect in patient received Diclofenac is much more longer then patient received Paracetemol.
Besides that, the pain intensity after the surgery was recorded using the Visual Analog System (VAS). The pain intensity after surgery was significantly more in patient received Paracetemol. At the time interval of 10 minutes and 1 hour there was no significant difference of pain intensity in both drugs. At the time interval from 3 to 5 hours, the pain intensity is higher in patient given Paracetamol compare to patient given Diclofenac (Figure 1). Table 1 and 2 shows the statistical result obtained for pain experienced following Paracetamol and Diclofenac. by using Visual Analogue Scale.
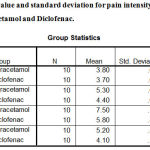 |
Table 1: Mean value and standard deviation for pain intensity of particpants following Paracetamol and Diclofenac.
|
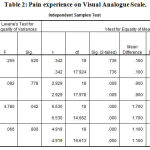 |
Table 2: Pain experience on Visual Analogue Scale.
|
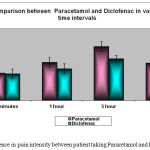 |
Figure 1: Difference in pain intensity between patient taking Paracetamol and Diclofenac.
|
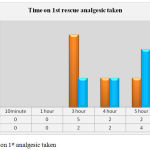 |
Figure 2: Time on 1st analgesic taken.
|
Discussion
This study shows that the preemptive administration of Diclofenac is more effective than Paracetamol in the control of pain after extraction. The mean duration of analgesia obtained by the preemptive administration was longer in particpants who received Diclofenac compared with those who received Paracetamol. Furthermore, the number of particpants requiring an analgesic at interval of 6 hours was less in the diclofenac group, thus showing the benefits of longer duration analgesia. According to the VAS scores, pain intensity was also seen to be lower in the diclofenac group in comparison with particpants who received paracetamol. It was also noticed that the diclofenac group had lower pain intensities throughout the evaluation period.
Non-steroidal analgesic drugs acts by inhibiting the same chain reactions that degrade phospholipids of injured cell membranes, responsible for the analgesic and inflammatory response.14,15 This eventually leads to the formation of pain and inflammation which are the consequences of the release of chemical mediators produced after tissue trauma. It would be reasonable to conclude that preemptive medication contributes to lowering the concentration of these mediators in tissue, considering that the presence of the drug in the blood stream inhibits their initial production. As a result, the lower the tissue concentration of these mediators, the weaker the algic and inflammatory response.16,17
Diclofenac being classified under NSAIDs is efficiently absorbed from the gastrointestinal tract; peak plasma concentrations occur 1.5 to 2 hours after ingestion and has a relatively short elimination half-life in plasma (1.5 hours), it persists in synovial fluid. The drug is metabolized in the liver and is eliminated by urinary and biliary excretion.18
There are 2 possible mechanisms for the efficacy of NSAIDs when administered prior to surgical trauma. The first mechanism involved is due to the pharmacokinetic advantage where administering the NSAIDs prior to pain onset, drug absorption would have begun and therapeutic blood level will be present at the time of pain onset.19 Second, diclofenac works by blocking the chemical substances called cyclo-oxygenase (COX) enzymes. These enzymes trigger the information of prostaglandins in the body. Sites of injury or harm are considered the normal place for production of the prostaglandins, which cause pain and inflammation. By obstructing the influence of COX enzymes, a smaller amount of prostaglandins are formed and as a consequence less pain and inflammation are felt. The reduction of biosynthesis of prostaglandins by inhibition of the cyclo-oxygenase enzyme system is considered an important mechanism of action of NSAIDs. When administered preoperatively, NSAIDs have been shown to be particularly effective in combating postoperative pain and edema.20
In a recent study, it has been identified that, diclofenac does not only inhibit COX but a number of other molecular targets of diclofenac also contributing to its pain relieving actions.21 These includes: voltage dependent sodium channel blockage by diclofenac, acid sensing ion channel blockage and allosteric modulation of potassium channel (hyperpolarization of the cell membrane caused by opening of potassium channel by diclofenac).
Unlike NSAIDs, paracetamol does not appear to inhibit the function of any cyclooxygenase (COX) enzyme outside the central nervous system and this is appears to be the reason why it is not useful as an anti inflammatory.22 However, paracetamol appear to selectively inhibit COX activity in the brain, which may contribute to its ability to treat fever and pain. These drug gets metabolized in the liver similar to diclofenac. The peak plasma level for paracetamol is about 40 to 60 minutes and it has a longer plasma half life compare to diclofenac which is 2 to 3 hours. The mechanism of action for paracetamol is not clearly established.23 It raises pain threshold, but has weak peripheral anti-inflammatory component. Its a good and promptly acting antipyretic but has a negligible anti-inflammatory action. Paracetamol is a poor inhibitor of PG synthesis in peripheral tissues, but more active on COX in the brain. Paracetamol could not inhibit COX in the peripheral tissue due to the presence of peroxides which are generated at the sites of inflammation. This explains the discrepency between its analgesic, antipyretic and anti-inflammatory actions.24
Based on the study done, it shows that patient from both the drug group shows no significant difference in pain intensity at the time interval between 10 minutes and 1 hour. However , from the time interval of 3 hours apart, patient from paracetamol shows an increase in pain intensity compare to patient who were given diclofenac drug. Besides that, none of the patient took rescue analgesic at the time interval between 10 minutes to 3 hour. At the peak of 3 hours it has been recorded that 5 out of 7 patient who took rescue analgesic are from the paracetamol group, which proves that paracetamol as a weak analgesic and anti inflammatory drug. A similar study is done by G Gazal by comparing paracetamol, diclofenac and ibuprofen for their efficacy as an preemptive analgesic. The result obtained by the study also shows a similar result in which diclofenac shows a better and prolonged analgesic effect compare to the other 2 drugs. There was no significant difference in the pain intesity at the time interval of 10 minutes and 1 hour in all the three comparitive drug. This could be due to the effect of local anaesthesia which persist up to few hours after extraction.25
Besides that, the study also shows that, particpants in diclofenac group had less pain at 4 hours to 6 hours postoperatively, and required less rescue analgesic than particpants in the paracetamol group. Differences between diclofenac and paracetamol in reducing postoperative pain intensity due to their mode of actions. There is considerable evidence that the antipyretic effect of paracetamol is centrally by inhibiting of prostaglandin E synthesis within the hypothalamus.26 However, the analgesic effect of diclofenac is peripherally by blocking impulse generation within the bradykinin sensitive chemoreceptors.27 Hence, paracetamol shows minimal anti inflammatory and analgesic action compare to diclofenac. The findings of this study are consistent with the results of another 2 studies. El Batawi administered one hour preoperatively a paracetamol and diclofenac sodium for children with traumatic dental treatments under general anesthesia and found that diclofenac sodium was more effective than paracetamol for pain relief as a preemptive analgesic.28 Another study carried out by Eslampour et al, who compared 3 analgesic drugs for their effectiveness as a preemptive analgesic, in which the drugs were administrated preoperatively for reducing postoperative pain associated with photorefractive keratectomy. Their findings revealed that the particpants in diclofenac group reported less pain than particpants in paracetamol and ibuprofen groups.29 Besides that, another similar study was done by Hyllested M and Jones to compare the analgesic effect of paracetamol with those of other NSAIDs. As a result, NSAID’s shows greater analgesic effect in postoperative management compare to Paracetamol.30 Based on the result obtain in these studies , it can be clearly noted that diclofenac has a better anti inflammatory and analgesic effect compare to paracetamol.
Conclusion
Extraction of teeth has been a common, routine dental procedure done in clinics which may lead to moderate to severe pain postoperatively. Any pain post operatively may cause a discomfort in particpants and affects the routine lifestyle. Hence, Preemptive analgesics play an important role in reducing postoperative pain and distress associated with painful dental procedures. The underlying principle is that the therapeutic intervention be made prior to the onset of pain, rather than a reaction to it. Two different drug has been used in this study to evaluate their efficacy as an preemptive analgesic and it can be concluded that Diclofenac is more effective then Paracetamol as an preemptive analgesia.
Reference
- Simone J. L., Jorge W. A., Horliana A. C., Canaval T. G., Tortamano I. P. Comparative analysis of preemptive analgesic effect of dexamethasone and diclofenac following third molar surgery. Brazilian oral research. 2013;27(3):266-71.
CrossRef - Gottschalk A., Smith D. S. New concepts in acute pain therapy: preemptive analgesia. American family physician. 2001;63(10):1979-84.
- Orozco-Solís M., García-Ávalos Y., Pichardo-Ramírez C., Tobías-Azúa F., Zapata-Morales J. R, Aragon-Martínez O. H, Isiordia-Espinoza M. A. Single dose of diclofenac or meloxicam for control of pain, facial swelling, and trismus in oral surgery. Medicina oral, patologia oral y cirugia bucal. 2016;21(1):e127.
CrossRef - Velasquez G., Cruz S. L, Espinoza M. Ketoprofen is more effective than diclofenac after oral surgery when used as a preemptive analgesic: a pilot study. J Oral Facial Pain Headache. 2014;28:153–158.
CrossRef - Grösch S., Niederberger E., Geisslinger G. Investigational drugs targeting the prostaglandin E2 signaling pathway for the treatment of inflammatory pain. Expert Opin Investig Drugs. 2016;20:1–11.
- Huang J., Wu J., Yang H. Z, Hong Y. Inhibition of prostaglandins synthesis in the inflamed site results in opioid-mediated hypoalgesia in rats. Sheng Li Xue Bao. 2016;68:241–248.
- Ong C. K., Lirk P., Tan C. H., Seymour R. A. An evidence-based update on nonsteroidal anti-inflammatory drugs. Clinical medicine & research. 2007;5(1):19-34.
CrossRef - Rahman M. M., Alam M. B., Islam M. A., Haque A. A. Non steroidal anti inflammatory drugs-an overview. Journal of Medicine. 2006;7(1):20-31.
- Takayama K., Hirose A., Suda I., Miyazaki A., Oguchi M., Onotogi M., Fotopoulos G. Comparison of the anti-inflammatory and analgesic effects in rats of diclofenac-sodium, felbinac and indomethacin patches. International journal of biomedical science: IJBS. 2011;7(3):222.
- Altman R., Bosch B., Brune K., Patrignani P., Young C. Advances in NSAID development: evolution of diclofenac products using pharmaceutical technology. Drugs. 2015;75(8):859-77.
CrossRef - Gan T. J. Diclofenac: an update on its mechanism of action and safety profile. Current medical research and opinion. 2010;26(7):1715-31.
CrossRef - Raffaeli G., Orenti A., Gambino M., Rios P. W., Bosis S., Bianchini S. Fever and pain management in childhood: Healthcare providers’ and parents’ adherence to current recommendations. Int J Environ Res Public Health. 2016;13:499.
CrossRe3f - Zarghi A., Arfaei S. Selective COX-2 inhibitors: a review of their structure-activity relationships. Iranian journal of pharmaceutical research: IJPR. 2011;10(4):655.
- Benetello V., Sakamoto F. C., Giglio F. P., Sakai V. T, Calvo A. M., Modena K. C. The selective and non-selective cyclooxy-genaseinhibitors valdecoxib andpiroxicam induce the same postoperative analgesia and control of trismus andswelling after lower third molar removal. Braz J Med Biol Res. 2007 Aug;40(8):1133-40.
CrossRef - Savage M. G., Henry M. A. Preoperative nonsteroidal anti-inflammatory agents: review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98(2):146-52.
CrossRef - Joshi A., Parara E., Macfarlane T. V. A double-blind randomized controlled clinical trial of the effect of preoperative ibuprofen, diclofenac, paracetamol with codeine and placebo tablets for relief of postoperative pain after removal of impacted third molars. Br J Oral Maxillofac Surg. 2004;42(4):299-306.
CrossRef - Jung Y. S., Kim M. K., Um Y. J., Park H. S., Lee E. W., Kang J. W. The effects on postoperative oral surgery pain by varying NSAID administration times: comparison on effect of preemptive analgesia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100(5):559-63.
CrossRef - Shruthi A. R., Kedarnath N. S., Srikanthan R. Preemptive Analgesic Efficacy of Diclofenac Sodium for Surgical Removal of Impacted Third Molars. Journal of Health Sciences & Research. 2016;72(10):5005. /jp-journals-10042-1033.
- Slater D., Kunnathil S., McBride J., Koppala R. Pharmacology of nonsteroidal antiinflammatory drugs and opioids. In.Seminars in interventional radiology. 2010;27(4):400-411. © Thie me Medical Publishers.
- Nazar M. N & Puthiriraj V. Analgesics following mandibular third molar surgery. International Journal of Pharmaceutical and Clinical Research. 6:13-19.
- Voilley N., de Weille J., Mamet J., Lazdunski M. Nonsteroid anti-inflammatory drugs inhibit both the activity and the inflammation-induced expression of acid-sensing ion channels in nociceptors. J Neurosci. 2001;21(20):8026-33.
CrossRef - Simmons D. L., Wagner D., Westover K. Nonsteroidal anti-inflammatory drugs, acetaminophen, cyclooxygenase 2, and fever. Clinical infectious diseases. 2000;31(5):211-8.
CrossRef - Anderson B. J. Paracetamol (Acetaminophen): mechanisms of action. Pediatric Anesthesia. 2008;18(10):915-21.
CrossRef - Ashok K., Nazar M. N. Efficacy of oral tramadol versus diclofenac sodium in post operative pain relief following mandibular third molar surgery.A double blind, randomized controlled trial. Journal of Pain Management. 2014;137-145.
- Gazal G., Al-Samadani K. H. Comparison of paracetamol, ibuprofen, and diclofenac potassium for pain relief following dental extractions and deep cavity preparations. Saudi medical journal. 2017;38(3):284.
CrossRef - Raffaeli G., Orenti A., Gambino M., Rios P. W., Bosis S., Bianchini S. Fever and pain management in childhood: Healthcare providers’ and parents’ adherence to current recommendations. Int J Environ Res Public Health. 2016;13:499.
CrossRef - Schwartz J. I., Musser B. J., Tanaka W. K., Taggart W. V., Mehta A., Gottesdiener K. M. Inhibition of prostacyclin and thromboxane biosynthesis in healthy volunteers by single and multiple doses of acetaminophen and indomethacin. Clin Pharm Drug Develop. 2015;4:337–345.
CrossRef - Batawi E. H. Effect of intraoperative analgesia on children’s pain perception during recovery after painful dental procedures performed under general anaesthesia. European Archives of Paediatric Dentistry. 2015;16:35–41.
CrossRef - Eslampour A., Malaekeh-Nikouei B., Abrishami M., Bayani R. Efficacy of extended-release oral diclofenac in postoperative pain management after photorefractive keratectomy. J Ocular Pharm Therapeut. 2013;29:670–673.
CrossRef - Hyllested M., Jones S., Pedersen J. L., Kehlet H. Comparative effect of paracetamol, NSAIDs or their combination in postoperative pain management: a qualitative review. British journal of anaesthesia. 2002;88(2):199-214.
CrossRef







