Aditya Prabawa and Ketut Surya Negara
Department of Obstetrics and Gynecology Faculty of Medicine University of Udayana/ Sanglah General Hospital Denpasar, Bali-Indonesia.
Corresponding Author E-mail: tutsuryanegara@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/1495
Abstract
Thyroid crisis is an emergency in Endocrinology which is characterized by acute hypermetabolic with rapid deterioration which is one of non-obstetric maternal death cause. This condition is rare serious complication, affect about 1-2% of patients with hyperthyroidism. Unrecognized and untreated thyroid storm causing life threatening condition. Management of thyroid storm in pregnancy is aimed to reduce the synthesis and secretion of thyroid hormone and pregnancy management. Explain about optimal diagnostic and treatment strategies of pregnancy with thyroid storm. A 28 years woman admitted to Obstetrics Emergency Room, third pregnancy with 36 weeks 2 weeks gestation was complained of shortness of breath since 3 days ago. History of hyperthyroid since 1 year ago, often palpitate, sweating and tremor. History of consumption PTU 3x100 mg oral but lack of obey. History of hypertension since 27 weeks gestation. Physical examination found that blood pressure was 170/110 mmHg, pulse rate 130 bpm, respiratory rate bpm, 84% oxygen saturation, 38.5°C temperature. Diffuse tiroid gland was palpable with size 1 x 2 cm, ronkhi in whole lung field. Obstetric examination was found breech presentation with FHB: 131 bpm. Laboratory result were TSHs / FT4: 0.24 / 1.72, T4 Total: 104. Thyroid storm diagnostic based on Burch Wartofsky score: 55. Initial treatment performed with oxygen administration, loop diuretics, chest X-ray examination and echocardiography. Followed by PTU therapy, lugolization and corticosteroids. After 48 hours of stabilization, we performed cesarean section and postoperative care at Intensive Care Unit. Thyroid storm is rare pregnancy complication. Diagnostic criteria using Burch and Wartofsky score. Management of thyroid storm in pregnancy includes anti thyroid drugs, lugol solution, corticosteroids and pregnancy management. Diuretic therapy is given due to fluid overload, besides that screening of thyroid hormone profile is important during antenatal care.
Keywords
Burch and Wartofsky; Pregnancy; Thyroid Storm
Download this article as:| Copy the following to cite this article: Prabawa A, Negara K. S. Diagnosis and Comprehensive Management of Thyroid Storm in Pregnancy : A Case Report. Biomed Pharmacol J 2018;11(3). |
| Copy the following to cite this URL: Prabawa A, Negara K. S. Diagnosis and Comprehensive Management of Thyroid Storm in Pregnancy : A Case Report. Biomed Pharmacol J 2018;11(3). Available from: http://biomedpharmajournal.org/?p=22045 |
Introduction
Thyroid storm is an Endocrinology emergency which characterized by acute hypermetabolic with rapid deterioration which is one of non-obstetric maternal death cause. Thyroid storm is a rare serious complication in hyperthyroidism patients (1-2% of cases of hyperthyroidism). The incidence of hyperthyroidism in pregnancy is about 0.2% and mostly subclinical. Approximately 90-95% of pregnant women with hyperthyroidism are manifestations of Grave’s disease. The adult mortality rate in the thyroid storm is 10-20% due to the late diagnostic and treatment.1,2,3
Principle of thyroid storm management in pregnancy are reducing the synthesis and secretion of thyroid hormones, decreasing the peripheral effects of thyroid hormone, inhibiting the conversion of T4 to T3, therapy to prevent systemic decompensation, trigger disease therapy, pregnancy management and supportive therapy.3
Case
A 28 years women, Referred from Secondary Hospital with third pregnancy with 36 weeks 2 days pregnancy, Acute Decompensated Heart Failure (ADHF), acute pulmonary edema and severe preeclampsia. Patients complain of shortness of breath since 3 days ago, weighing since 1 day ago accompanied by cough, no signs of labor, baby motion felt good. Patients previously had a history of hyperthyroidism since 1 years ago. Patients said often palpitation, sweating and tremor. History of taking PTU 3×100 mg orally, but patients do not obedient medication. Patients also have a history of hypertension since 27-28 weeks in midwife (blood pressure 140/90 mmHg). Known breech position since 33-34 weeks.Physical examination found the patient admitted with weak general condition, blood pressure was 170/110 mmHg, pulse rate 130 bpm, respiration rate 40 bpm, 84% oxygen saturation, 38.5 °C temperature. Diffuse tiroid size 1 x 2 cm was palpable, ronkhi in whole lung field. Obstetric examination found that no uterine contraction, breech presentation, DJJ: 131 bpm. From laboratory examination we found that TSHs: 0.24, FT4: 1.72, T4 total: 104, urinalysis : Protein +4, LDH: 625. From ultrasonography found single fetus, life, breech presentation, fetal heart rate and good fetal movement. Fetal biometry appropiate to gestational age, with an estimated fetal weight of 2490 grams. Placenta corpus posterior grade II with enough amniotic fluid. EKG results obtained sinus tachycardia. An anteroposterior thoracic image was found to suggest pulmonary edema, pneumonia and bilateral pleural effusionTemporary diagnosis at Sanglah Hospital Obstetrics Emergency Room were G3P2002 36 weeks 2 days Single / Life, Breech Presentation, Severe Preeclampsia (Partial HELLP Syndrome), Impending Respiratory failure Lung Edema, Bilateral pleural effusion, hyperthyroidism, suspected cardiac abnormalities.
 |
Figure 1: Electrocardiography result.
|
 |
Figure 2: Thorax AP examination.
|
Initial treatment with non-rebreathing mask (NRM) 15 lpm, Magnesium Sulphate 40% 4 grams iv followed by 6 grams in Ringer Lactate 500 mL 28 dpm for 24 hours, Nifedipine 10 mg every 8 hours when MAP ≥ 125 mmHg , Furosemide 80 mg iv, Morphine 2 mg iv (1 mg / hour) and ISDN 2 mg / hour iv continued by Consultation to Cardiology, Pulmonology and Internal Medicine Endocrinology Division.
Cardiology performed bed-side echocardiography with moderate-severe mitral regurgitation due to suspect anterior mitral leaflets prolaps and ICCU (Intensive Cardiovascular Care unit treatment. Administration of furosemide 80 mg iv, ISDN 2mg /hours and O2 NRM 15 lpm was continued.
Internal Medicine Department using Burch-Wartofsky score (BW) as diagnostic tools of thyroid crisis with values are 55. The following criteria were temperature (38.2°C): 10 points, tachycardia (130 bpm): 20 points, Congestive heart failure : 15 points, no gastrointestinal dysfunction : 0 poin, no central nervous system dysfunction: 0 poin, triggering factor (Pneumonia + preeclampsia): 10 points. Main treatment by administration of PTU 200 mg every 6 hours orally, Lugol 6 drops every 8 hours given 1 hour post PTU and Dexamethasone 2 mg each 6 hours iv.
Additional diagnosis of Pulmonology Departement was Community Acquired Pneumonia based on clinical finding of cough, fever, ronkhi in both lung suspected of triggering a thyroid storm. Principle treatment with Ceftriaxone 1 x 2 gram iv and Azithromycin 1 x 500 mg orally.
Team meeting performed and the result were termination of pregnancy with cesarean section and tubectomy after optimizing the general condition for 48 hours with back up from Anesthesia, Pediatrics, Cardiology, Pulmonology and Internal Medicine Endocrinology Division. Postoperative care at ICCU, maternal and baby thyroid hormone levels examination were performed at 3 months after cesarean section.
After stabilization was achieved by administration of diuretics, PTU, lugolization, corticosteroids and intravenous antibiotics, score of BW: 20 was indicated optimal condition for termination of pregnancy. Cesarean section and tubectomy performed at Central Operating Room. Postoperative care, PTU was reduced to 3 x 100 mg orally, dexhametasone and lugolization were discontinued, cefixime was given 2 x 200 mg orally.
Discussion
In this case, the diagnosis of hyperthyroidism is established when the patient comes to Obstetrics Emergency Room. Clinically patients complain shortness of breath and palpitation. Objectively physical examination found high pulse rate and respiratory rate, enlarged diffuse thyroid gland size of 1 cm x 2 cm followed when swallowing. CAP are the triggers of thyroid storm. The problem of diagnosis in these patients is actually diagnosis of thyroid storm not immediately enforced at secondary hospitals due to the disguised of thyroid crisis diagnostic by ADHF symptoms, acute pulmonary edema and severe preeclampsia. Theoretical pregnancy will lead to increased concentration of Thyroid binding globulin (TBG) resulting in the production of thyroid hormone outside the thyroid gland increases resulting in total increase of T4 and T3.4,5 T4 metabolism increases in the second and third trimesters, due to increased deiodination of placenta type II and type III, which increases the conversion of T4 metabolism. In this case analyzed, the pregnancy exacerbates hyperthyroid conditions in patients in addition to other trigger factors such as hypertension and infection. In theory the diagnostic flow of thyroid crisis is based on clinical findings of fever, tachycardia, signs and symptoms of heart failure, decreased awareness or seizures, gastrointestinal disorders, history of lack hyperthyroid medication, family history with hyperthyroidism, precipitating factors such as infection, hypertension, trauma, history of surgery and signs of hyperthyroidism such as: exopthalmus, goiter, bruit on the thyroid gland and tremors. Thyroid storm diagnostic criteria using BW scores, involving several clinical components such as thermoregulation, central nervous system, gastrointestinal, and cardiovascular6
 |
Figure 3: Tyhroid storm diagnostic algorithm7
|
Patient have been through the diagnostic flow procedure as mentioned above and have BW score: 55, where if a score> 45 apppropiate for thyroid crisis diagnostic. The components of these scores are fever, tachycardia, trigger factors and cardiovascular dysfunction characterized by congestive heart failure. Laboratory tests support the diagnosis by increase of FT4 (1.72), T4 (104.1) and decrease TSHs (0.24). Fast and precise diagnosis in this case build the early treatment of thyroid strom and prognosis will be better.8,9
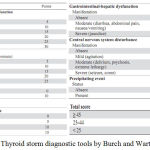 |
Figure 4: Thyroid storm diagnostic tools by Burch and Wartofsky Score7
|
Treatment of hyperthyroidism during pregnancy should consider understanding of treatment, the choice of therapy for pregnant women and the goal of therapy. Aim of treatment is to maintain persistent hyperthyroidism in the mother’s mild limit to prevent fetal hypothyroidism. From the beginning of the diagnosis, the patient has been receiving PTU 3 x 100 mg orally. This dose appropiate with the recommendation by the American Thyroid Association, which is 100-600 mg per day. Other drugs such as methimazol have not been proven safe enough, whereas beta-blockers such as propanolol are contraindicated for pregnancy.10,11
For management of thyroid storm in this patient, which includes PTU 200 mg every 6 hours orally, 6 drops of lugol solution every 8 hours was given 1 hour after PTU and Dexamethasone 2 mg every 6 hours iv. PTU can inhibit thyroid hormone synthesis and has the effect of increasing the peripheral conversion of T4 to T3. The lugol liquid was a saturated potassium iodide liquid, where with a high iodine-containing preparation, uptake of iodine in the thyroid gland can be decreased and then thyroid hormone secretion can be inhibited. The use of glucocorticoids such as dexamethasone is known to decrease the conversion of T4 to T3 and has a direct effect on the autoimmune process on Graves’ disease.12,13
Heart failure treatment by given diuretic therapy to decrease fluid overload in the lung parenchym. Patient had impending respiratory failure, then performed a resus call, immediate treatment with oxygenation then Furosemide 80 mg iv which acts as a diuretic. Morphine 2 mg/hours and intravenous ISDN is used to lower blood pressure, relieve pain and as a vasodilator agent.14 In addition, when patients are admitted to the hospital, preeclampsia management involves administering Magnesium Sulphate and Nifedipine when MAP ≥ 125mmHg. For the treatment of CAP as recommended by American Family Physician were given combination of antibiotic like Cephalosporin and Macrolide group. With the various therapies given, the clinical and laboratory conditions of the patient generally improve. Patient had well therapy respons and after optimizing the patient’s condition, performed C-section and tubectomy.
If thyroid storm occur in preterm pregnancy with not viable fetus, conservative treatment will be considered after perform immediate treatment of thyroid storm. Clinical improvement was achieved, thyroid hormone profile levels improved and fetus well being was good.
In this case the maternal prognosis was good, after following for 1 year where the patient routinely undergo treatment with PTU 3 x 100 mg orally and clinically patient in good condition. No more symptoms of hyperthyroidism such as palpitations anxiety, tremors, fatigue, diarrhea, sweating, and weight loss. Three months after treatment at the Sanglah General Hospital, TSHs and FT4 levels examination were performed on the mother and normal thyroid function was obtained. TSH values was 0.953 (N: 0.27-4.92 uIU / mL) and FT4 1.05 (N: 0.93-1.70 mg / dL).
In this case the prognosis of the baby was good, after being followed for one year clinically there is no sign of hyperthyroidism in the baby such as high fever, tachycardia or fetal goiter. No growth and development disturbance. Laboratory evaluations were performed at 3 months of age with normal range value of TSH (2.23 uIU / mL) and FT4 (1.24 mg / dL).
Conclusion
Thyroid storm is Endocrinology emergency characterized by acute hypermetabolic with rapid deterioration of life-threatening condition. The criteria for thyroid storm diagnosis by using BW scores, involving several components such as thermoregulation, central nervous system, gastrointestinal, and cardiovascular. Management of thyroid storm includes PTU, lugol solution given 1 hour after PTU and dexamethasone whereas heart failure treatment can be given diuretics to reduce fluid overload in other hand CAP treatement can be given antibiotic combination like cefalosporin and macrolide group. In this case, the patient had good therapeutic response. After optimizing the patient’s condition C-section and Tubectomy were performed.
To reduce the incidence rate of thyroid storm in pregnancy, required thyroid hormone profile screening at antenatal care. The appropriate contraceptive methods in hyperthyroid patients by using non-hormonal contraceptives such as condoms, IUDs (intrauterine contraceptives) or tubectomy.
Acknowledgement
The author(s) received no specific funding for this work.
References
- Swee du S, Chang C.L, Lim A. Clinical characteristics and outcome of thyroid storm: a case series and review of neuropsychiatric derangements in thyrotoxicosis. Journal of American College of Endocrinology and American Association of Clinical Endocrinologist. 2015;21(2):182-9.
CrossRef - Garmendia M.A, Santos P.S, Guillén-Grima F, Galofré J.C. The incidence and prevalence of thyroid dysfunction in Europe: a meta-analysis. J Clin Endocrinol Metab. 2014;99:923–31.
CrossRef - Satoh T, Isozaki O, Suzuki A, Wakino S. Guidelines for the management of thyroid storm from the japan thyroid association and japan end ocine society. Endocrine Journal. 2016;63(12):1025-64.
CrossRef - McKenzie J.M, Zakarija M. Fetal and neonatal hyperthyroidism and hypothyroidism due to maternal TSH receptor antibodies. Thyroid. 2002;2(2):155–9.
CrossRef - Hamada N, Momotani N, Ishikawa N. Persistent high TRAb values during pregnancy predict increased risk of neonatal hyperthyroidism following radioiodine therapy for refractory hyperthyroidism. Endocr J. 2011;58(1):55–8.
CrossRef - Kádár A, Sánchez E, Wittmann G. Distribution of hypophysiotropic thyrotropin releasing hormone (TRH) synthesizing neurons in the hypothalamic paraventricular nucleus of the mouse. J Comp Neurol. 2010;518:3948–61.
CrossRef - Wartofsky L. Clinical criteria for the diagnosis of thyroid storm. Thyroid. 2012;22:659-660.
CrossRef - Nader S. Thyroid disease in pregnancy. In : Creasy R.K, Resnik R, Iams J.D, Lockwood C.J, Moore T.R, Greene M.F. Creasy & Resnik’s maternal fetal medicine : principles and practice. 7th Edition. Philadelphia : Elsevier Saunders. 2014;1009-20.
- Akamizu T, Satoh T, Isozaki O, Suzuki A, Wakino S, Iburi T. Diagnostic criteria, clinical features, and incidence of thyroid storm based on nationwide surveys. Thyroid. official journal of the American Thyroid Association. 2012;22(7):661-79.
CrossRef - Stagnaro-Green A, Abalovich M, Alexander E. Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and postpartum. Thyroid. 2011;21:1081–125.
CrossRef - Groot D.L, Abalovich M, Alexander E.K. Management of thyroid dysfunction during pregnancy and postpartum: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2012;97:2543–65.
CrossRef - Bahn R.S, Burch H.B, Cooper D.S. Hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists. Endocr Pract. 2011;17(3):157–65.
CrossRef - Isozaki O, Satoh T, Wakino S, Suzuki A, Iburi T. Treatment and management of thyroid storm: Analysis of the nationwide surveys. Clin Endocrinol. 2016;84:912-18.
CrossRef - Ross S.D. Hyperthyroidism during pregnancy treatment. Up to date topic. 2017;7784.








