Manuscript accepted on :March 09, 2018
Published online on: --
Plagiarism Check: Yes
Zahraa S. Abed Karkosh1, Basima M. A. Hussein2 and Wifaq M. Ali AL-Wattar3
1Master Student of Prosthodontics at University of Baghdad.
2Head of Prosthodontic Department at University of Baghdad.
3medicine Micro Biology at University of Baghdad.
DOI : https://dx.doi.org/10.13005/bpj/1360
Abstract
The aim of this study was to evaluate the effect of modified heat cured polymethyl methacrylate denture base (PMMA) or varnish coating of the denture base on candida albicans adhesion and porosity. First experimental group was prepared by addition of 15% phosphoric acid 2-hydroxyethyl methacrylate ester with polymethyl methacrylate monomer. While second experimental group prepared by varnish layer coating after material processing, these groups were compared with the control one. Three groups of vertex acrylic resin used as control, mPMMA and varnish coated group (PPH Cerkamed Wojciech Pawlowski, Poland). The inverted light microscope was used to measure the candida albicans adherence after one week and one month of processing. Two-way ANOVA, LSD test, T- test and Dunnett T3 were performed on data. Modified Acrylic resin showed highly significant reduction in candida albicans adhesion and porosity, also for varnish coating group showed highly significant reduction in candida albicans adhesion and porosity test.
Keywords
Candida Albicans and Porosity Dental Varnish; Phosphoric Acid 2-Hydroxyethyl Methacrylate Ester;
Download this article as:| Copy the following to cite this article: Karkosh Z. S. A, Hussein B. M. A, AL-Wattar W. M. A. Effect of Phosphoric Containing and Varnish-Coated Groups on Candida Albicans Adhesion and Porosity of Heat Cure Acrylic Denture Base Material. Biomed Pharmacol J 2018;11(1). |
| Copy the following to cite this URL: Karkosh Z. S. A, Hussein B. M. A, AL-Wattar W. M. A. Effect of Phosphoric Containing and Varnish-Coated Groups on Candida Albicans Adhesion and Porosity of Heat Cure Acrylic Denture Base Material. Biomed Pharmacol J 2018;11(1). Available from: http://biomedpharmajournal.org/?p=19452 |
Introduction
Denture stomatitis define as a widely occur benign disorder in denture wearers. Also define as a chronic infection; with redness of the oral mucosa, that support removable denture1 Denture stomatitis has other names like (chronic denture palatitis, chronic atrophic candidiasis, denture sore mouth and denture-induced candidiasis). The incidence of denture stomatitis is 25- 67% of complete denture wearers and more occurrence in old age women.2 It considered as common mucosal lesion associated with removable dentures that occurred one in every three complete denture wearers. 3 The causes of denture stomatitis considered multifactorial.4-6 Acrylic resin proved to be convenience for yeast colonization, giving acceptable conditions for adhesion and growth of yeast because of its high porosity.7,8 Furthermore, Denture stomatitis may result from attraction forces between candida albicans (negatively charged) and positively charged PMMA, therefore attempting to reduce candida adhesion by creation of electrostatic repulsion forces with negatively charged polymers. The aim of this study was to evaluate the effect of phosphoric acid 2-hydroxyethyl methacrylate ester containing PMMA and varnish-coated group on adherence of candida albicans and porosity.
Material and method
Modified PMMA (mPMMA) polymer was prepared by addition phosphoric acid 2-hydroxyethyl methacrylate ester (Sigma Aldrich) to methyl methacrylate monomer in 15% ratio then mixed with powder (vertex) according to manufactures instruction. Three groups were prepared in this study, they divided into group A control (vertex dental BV), B varnish coated acrylic resin group (PPH Cerkamed Wojciech Pawlowski, Poland) and C phosphoric acid 2- hydroxyethyl methacrylate ester containing group. Ten disc shape acrylic resin samples (for each group) were prepared for candida albicans adherence test with dimensions 10mm x3mm (diameter x thickness).9 Ten disc shape samples (for each group) were prepared for porosity test with dimension 30 mm diameter x 3 mm thickness.10-12 For isolation of candida albicans, swabs were taken from ten patients attended to college of dentistry / university of Baghdad, diagnosed clinically with candida due to D. stomatitis. All patients had extensive verbal informed consent and the trial was approved by college of dentistry/ university of Baghdad. Identification of candida albicans was done through microscopic appearance, macroscopic appearance and biomedical test (API), Candida albicans preparation done by taking the isolated Candida albicans plated on sterile Sabouraud dextrose agar media, incubated for 24- 48 hours at 37c. Then a moderate size colony was taken with microbiological loop and transferred to 20 ml of Sabouraud dextrose broth in the autoclavable tube,13,14 five folds dilution made in SDB from original solution using microtiter plate and micropipette. In a pilot study, results indicated that dilution four was suitable to test inhibitory property. the dilution process done inside hood to prevent contamination, the disks put inside broth and incubated them for 1 hour at 37c, after that the disks washed with Phosphate Buffer Saline for 1 min with help of vortex mixer, the samples fixed with methanol (80%) for 30 sec then stained with crystal violet for 30 sec. The samples were examined under inverted light microscope, the adherent yeast cells enumerated in four fields of view of each samples.
while the process of dental varnish application was done by drooling 1 microliter of dental varnish with micropipette, dropped in the center of sample, the varnish was spreaded evenly from center toward periphery using brush supplied by the manufacture, gentle steam of air was applied for 5 sec then allowed to dry for 30 sec then applied another layer and cured with light for 30 sec according to manufacture instruction, Samples were immersed in permanent black ink solution for half an hour, then washed for 10 seconds, then allowed to dry with absorbent paper porosity was measured under inverted light microscope with 400 X magnification. Also porosity was measured with stereomicroscope.
Counting of candida albicans cells was done on both polished and unpolished surfaces after two duration (after one week and after one month which in meanwhile the samples kept in artificial saliva). Statistical analysis. The mean, standard deviation, two – way ANOVA test and LSD test and Dunnett T3 used to compare between groups.
Results
The PMMA and modified PMMA polymers were examined by FTIR and showed a changes occurred in area of 3010 cm-1 for Alkenyl C-H stretch, at 1720 cm-1 appeared Ester C=O stretch ( all types of C=O bonds either aldehyde or ketone bonds have approximately same area of absorption. Ester bond is predominant in the product), at 1350cm-1 organic phosphate P=O stretch appeared, at 1050cm-1 aliphatic phosphates P-O-C stretch appeared ( this bond id predominant in ester compound), alkyl substituted ether C-O-C appeared at 1140cm-1 and O=C=O appeared at 2400cm-1 (this from atmosphere or produced with product) as in figure (1).
 |
Figure 1: FTIR analysis for mPMMA
|
Candida Adherence Test Results
Candida albicans adherence counts: The results found highly significant reduction in the number of the adherent candida albicans cells for both of PA2HEME group and varnish coated groups comparing to the control group, however; the PA2HEME group showed the lowest number of candida albicans among groups as in figures (2), (3) and (4).
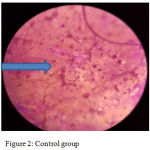 |
Figure 2: Control group
|
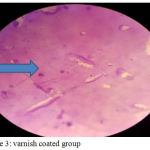 |
Figure 3: varnish coated group
|
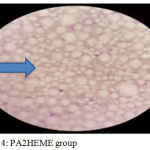 |
Figure 4: PA2HEME group
|
Number of candida albicans cells counted on every polished and unpolished surfaces in each group regarding testing period (one week and one month) showed highly significant reduction in number of cells between groups with least number in PA2HEME group. While polished surfaces showed lower number when compared with unpolished in all groups regarding testing periods as in figure (5).
 |
Figure 5: mean of candida cell count groups and surfaces A after one week B after one month
|
Statistical analysis showed significant differences between tested groups when means of candida albican cells of polished or unpolished surfaces were compared after one week. These results was repeated when test was done after one month. Furthermore, LSD analysis was done to compare between groups for polished or unpolished surfaces after one week. The results showed significant differences between groups. LSD analysis was done also after one month showed significant differences between groups and surfaces as shown in table (1)
Table 1: descriptive and statistical test of candida adherence among groups within surfaces and times.
| Surfaces | Time | Group | N | Mean | SD | F | p-value | Multiple comparisons Using LSD |
| Polished | 1week | Control | 10 | 71.600 | 1.955 | 3333.495 | .000 | Control X Varnish=0.000 |
| Varnish | 10 | 21.200 | 1.814 | Control X PA2HEME=0.000 | ||||
| PA2HEME | 10 | 9.700 | 1.567 | Varnish X PA2HEME=0.000 | ||||
| 1month | Control | 10 | 67.600 | 1.838 | 1863.259 | .000 | Control X Varnish=0.000 | |
| Varnish | 10 | 26.600 | 1.578 | Control X PA2HEME=0.000 | ||||
| PA2HEME | 10 | 11.200 | 1.619 | Varnish X PA2HEME=0.000 | ||||
| Unpolished | 1week | Control | 10 | 98.500 | 1.900 | 5740.032 | .000 | Control X Varnish=0.000 |
| Varnish | 10 | 29.900 | 1.792 | Control X PA2HEME=0.000 | ||||
| PA2HEME | 10 | 18.700 | 1.767 | Varnish X PA2HEME=0.000 | ||||
| 1month | Control | 10 | 80.100 | 2.923 | 2278.948 | .000 | Control X Varnish=0.000 | |
| Varnish | 10 | 36.700 | 2.751 | Control X PA2EME=0.000 | ||||
| PA2HEME | 10 | 17.100 | 1.663 | Varnish X PA2HEME=0.000 |
Porosity test: number of pores showed highly significant reduction for both experimental groups, however; the PA2HEME containing group had the lowest number of pores as in figures (6), (7), (8) and (9).
 |
Figure 6: Control group
|
 |
Figure 7: Varnish coated group
|
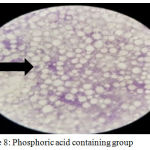 |
Figure 8: Phosphoric acid containing group
|
ANOVA test between all groups for each surfaces showed high significant differences. Further analysis between every two groups indicated high significant differences as shown in table (2)
Table 2: multiple comparisons of No. of pores by Dunnett’s T3
| Surface | Group | Mean | SD | F | Sig. | Multiple comparisons by Dunnett’s T3 |
| Polished | Control | 31.700 | 2.003 |
991.013 |
0.000 |
Control X Varnish=0.000 |
| Varnish | 10.900 | 1.663 | Control X PA2HEME=0.000 | |||
| PA2HEME | 4.500 | .527 | Varnish X PA2HEME=0.000 | |||
| Unpolished | Control | 51.100 | 1.524 |
2528.559 |
0.000 |
Control X Varnish=0.000 |
| Varnish | 19.900 | 1.524 | Control X PA2HEME=0.000 | |||
| PA2HEME | 6.900 | .738 | Varnish X PA2HEME=0.000 |
Results of stereomicroscope for topography: the results obtained with stereomicroscope, which read the topography of samples in which the porosity appeared as white, small voids as in figures (10), (11) and (12).
 |
Figure 9: Topography of Control group
|
 |
Figure 10: Topography of varnish coated group
|
 |
Figure 11: Topography of phosphoric acid containing group
|
Discussion
Denture stomatitis consider multifactorial condition that closely related to acrylic denture wearers.15 This study intended for production of new modified PMMA denture base material and coating the surface of PMMA with dental varnish in order to reduce candida albicans adherence to the denture base, which is the main causative factor for denture stomatitis. In the present study 15% of PA2HEME added to monomer then mixed with acrylic resin powder to produce a new modified PMMA and this used to measure the candida albicans adherence test, the result showed highly significant reduction in the candida albicans isolate adherence comparing to the control group and varnish coated group, this probably due to production of new polymer that give free hydroxyl group which give a negative charge to structure of the new PMMA within physiological PH and this negative net of new structure can create a repulsion forces with the candida albicans. In addition the significant effect of physiochemical forces like electrostatic force and hydrophobic interaction.16 The results go in agreement with Sang E. et al, 2009 that found a significant reduction in the candida albicans adhesion by using modified PMMA with methacrylic acid. Since there were two surfaces, the polished surface showed lower number of candida albicans cells comparing to unpolished surfaces which is due to surfaces roughness or surfaces energy as it is increase with grinding surface.17 For varnish-coated group results showed highly significant reduction in the adherence of candida albicans isolates comparing to control group, this could be due to coating the PMMA with isolated environment and create a barrier against candida albicans which is thin, chemical stable coating that alter the surface chemistry of surfaces to which it apply without mechanical protection19 that reduce roughness and enhance smoothness. The results go in agreement with Sang et al., 2007, which found a decrease in candida albicans attachment to mPMMA and PMMA coated with self- bonding polymer. While for porosity test, the results showed highly significant reduction for both PA2HEME and varnish-coated groups comparing to control group, however; the PA2HEME had the lowest No. of pores among the three groups, for varnish-coated group, this could be due to coating the surface with dental varnish and made effective seal for majority of pores on the surfaces of PMMA, which also may enhance the reduction of candida albican cells by reducing the niches for aggregation of candida cells. The results goes in agreement with Sang et al., 2007 who coated the acrylic specimens with self-bonding polymer to produced effective seal against staining restorative resins. While for phosphoric acid containing group, the No. of pores showed highly significant reduction and this could be due to PA2HEME crystalized the PMMA molecules with tightly packed together and this idea supported by the results obtained with stereo microscope which read the topography of samples.
Conclusion
The negatively charged PMMA and varnish coated PMMA can considered to be therapeutic way for preventing denture stomatitis through reduction the candida albicans colonization and porosity. The results of present study suggest that modification of PMMA with PA2HEME can reduce the porosity of mPMMA. In addition, the varnish-coated group suggest highly reduction in both candida albicans adhesion and porosity of surface treated acrylic resin.
Acknowledgement
This work was based to thesis submitted to the council of college of dentistry / Baghdad University as a partial fulfillment for the requirement for the degree of Master of Science in prosthodontics, 2017.
References
- Puryer J. Denture Stomatitis – A Clinical Update. Dental Update. 2016;43(6):529-535.
CrossRef - Naik A. V and Pai R. C. A study of factors contributing to denture stomatitis in a North Indian community. Int J Dent. 2011;4. doi:10.1155/2011/589064, Article ID 589064.
CrossRef - Emami E., Kabawat M., Rompre P. H., Feine J. S. Linking evidence to treatment for denture stomatitis: A meta-analysis of randomized controlled trials. J Dentist. 2014;42:99–106.
CrossRef - Shulman J. D., Rivera-Hidalgo F., Beach M. M. Risk factors associated with denture stomatitis in the United States. J Oral Pathol Med. 2005;34(6):340-346.
CrossRef - Gendreau L., Loewy Z. G. Epidemiology and etiology of denture stomatitis. J Prosthodont. 2011;20(4):251-60.
CrossRef - Arendorf T. M., Walker D. M. Denture stomatitis a review. J Oral Rehabil. 1987;14(3):217-227.
CrossRef - Martori E. Risk factors for denture-related oral mucosal lesions in a geriatric population. Journal of Prosthetic Dentistry. 2014;111(4):273-279.
CrossRef - Pinelli L. A., Montandon A. A., Moraes T. A., Fais L. G. A. Ricinus communis treatment of denture stomatitis in institutionalised elderly. J Oral Rehabil. 2013;40(5):375-380.
CrossRef - Douglas R. M. MSc, Luiz Fernando Group, MSc, Aline Satie Takamiya, MSc, Emerson Rodrigues de Camargo, DDS, PhD, Adhemar Colla Ruvolo Filho , DDS, PhD, and Debora Barros Barbosa, DDS, PhD, Sliver Distribution and Release from an Antimicrobial Denture Base Resin Containing Sliver Colloidal Nanoparticles. journal of prosthodontics. 2012;217-15.
- Reits P. V., Sandres J. L and Levin B. The curing of denture acrylic resin by micro wave energy . physical properties. Quintessence International. 1985;6:547.
- Garcia R and Bel D. A. Relining of denture base: conventional and micro wave methods. Revista da faculdad de Odontologia da Universidade de Sao Paulo. 1996;10:295.
- AL-Fahdawi I. H. The effect of polyvinyl pyrrolidine (PVP) addition on some properties of heat- cure acrylic resin denture base materials. A Ph.D. thesis Department of prosthodontic, College of Dentistry, University of Baghdad. 2009.
- Kohanteb J., Sadeghi E. Penicillin-resistant Streptococcus pneumoniae in Iran. Med Princ Pract. 2007;16:29-33.
CrossRef - Fani M. M., Kohanteb J. Inhibitory activity of Aloe vera gel on some clinically isolated cariogenic and periodontopathic bacteria. J Oral Sci. 2012;54:15-21.
CrossRef - Hasan S. Denture Stomatitis: A Literature Review. Journal of Orofacial and Health Sciences. 2015;10:5958. /2229-3264.00013.1
- Sang E. P., Chao M and Raj P. A. Mechanical Properties of Surface-Charged Poly(MethylMethacrylate) as Denture Resins. International Journal of Dentistry. 2009;6. Article ID 841431.
- Puri G.,David W. B., Virendra B. D., Periathamby A. R., Sameer K. R., Dhi G . f and Andrew R. D. 2008, “Effect of phosphate group addition on the properties of denture base resins. J Prosthet Dent. 2008;100:302-308.
CrossRef - Park E., Periathamby A. R and Loza J. C. Effect of surface-charged poly (methyl methacrylate) on the adhesion of Candida albicans. Journal of Prosthodontics. 2003;12(4):249–254.
CrossRef - Park S. E., Weber H. P., Ishikawa-Nagai S. Self-bonding polymers as surface-coatings of restorative resins to prevent staining. J Clin Dent. 2006;17:134-137.
- Sang E. P. DDS, MMSc, Ryan Blissett, DMD, Srinivas M. Susarla, DMD & Hans-Peter Weber DMD, Dr Med Dent ,Candida albicans Adherence to Surface-Modified Denture Resin Surfaces, Department of Restorative Dentistry and Biomaterials Sciences, Harvard School of Dental Medicine, Boston. 2007. MA, doi: 10.1111/j.1532-849X. 00292.x.







