Ramya Rachamanti1 , V. Prem kumar1
, V. Prem kumar1 , M. C. Das1
, M. C. Das1 , Manam Mani Srikanth2
, Manam Mani Srikanth2 and M. Lakshmi Shravanthi2
and M. Lakshmi Shravanthi2
1Department of Pharmacology, NRI academy of medical sciences, Guntur.
2NRI academy of medical sciences, Guntur.
Corresponding Author E-mail: ramz599@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/1357
Abstract
To identify the utilization pattern of antimicrobials in patients with suspected wound infections and skin and soft tissue infections (SSTI) according to WHO (World Health Organization) drug utilization indicators.This is a cross-sectional, record based study conducted in a tertiary care hospital after obtaining Institutional Ethical Committee approval. Patients of all ages admitted into N.R.I hospital between June to October 2017 suspected of wound and SSTIs were included in this study. Data of patients was collected from Medical records Department of the hospital. Analysis was done on 100 patients basing on inclusion criteria. Wound infections and SSTIs were found to be more common in males and in age group below 35 yrs. The major co-morbid conditions associated were diabetes and hypertension. Evaluation of prescriptions based on WHO drug utilization indicators showed that a total 201 antimicrobials were prescribed for 100 patients irrespective of positive or negative culture. Among antimicrobials, 31.8% were prescribed by their generic name.42.78 % were in the form of injections. 94.51 % of antimicrobials were in the National list of essential medicines 2015. Average duration of treatment given was for 7±3 days in the hospital. All the patients recovered well and got discharged. None of the patients died during the treatment among these 100 patients. The results obtained will be useful for implementing the modifications in the prescription for betterment of the patients and for the community.
Keywords
Antimicrobials; Skin and Soft Tissue Infections; W. H. O. Indicators; Wound Infections
Download this article as:| Copy the following to cite this article: Rachamanti R, kumar V. P, Das M. C, Srikanth M. M, Shravanthi M. L. Antimicrobial Utilization in Wound Infections in Tertiary Care Hospital. Biomed Pharmacol J 2018;11(1). |
| Copy the following to cite this URL: Rachamanti R, kumar V. P, Das M. C, Srikanth M. M, Shravanthi M. L. Antimicrobial Utilization in Wound Infections in Tertiary Care Hospital. Biomed Pharmacol J 2018;11(1). Available from: http://biomedpharmajournal.org/?p=19363 |
Introduction
Drug utilization research or study was defined by WHO (World health organization) in 1977 as the study of marketing, distribution, prescription, and use of drugs in a society, with special emphasis on medical, social and economic consequences.1 It helps in the identification of clinical use of drugs in various populations and its impact on healthcare system.
Wound infections and skin and soft tissue infections (SSTIs) are rising rapidly in the last few decades with a dramatic increase of the economic burden on the patient.2 They can lead to complications like bacteraemia, death,3,4 increased hospitalization and use of antimicrobial therapy can result in significant disability.5
Antimicrobial consumption is increasing globally. Between 2000 and 2010, consumption was increased by 35%. Russia, India, China, and South Africa accounted for 76% of this increase.6 Increased access to antimicrobials has lowered morbidity and mortality rates to a greater extent but also lead to development of resistance. Hence rational pharmacotherapy is the need of the hour to prevent rapidly emerging antimicrobial resistance. Efforts have been made by WHO to promote rational utilization of the drugs including antimicrobials.7
To ensure quality medical care, Drug utilization pattern studies are quite essential. It in turn helps in minimization of economic burden on patient and optimal utilization of available funds.
The Present Study was Carried out with these Objectives
To assess the antimicrobial utilization pattern of patients admitted in tertiary care hospital with suspected wound and skin and soft tissue infections as per WHO drug utilization indicators.
To identify the associated demographic relations and co-morbid conditions.
Materials and Methods
This is a cross-sectional, record based, observational study done at NRI hospital, Guntur. After obtaining Institutional Ethics committee approval, data of patients admitted in between June 2017-October 2017 was collected from the records maintained in the Medical record section (MRD) section.
Inclusion Criteria
Case sheets of patients of all ages admitted into NRI hospital with suspected wound infections and SSTIs were included in the study. Case sheets with incomplete information were excluded from the study.
Sample Size Calculation
On an average, 40 cases of wound infections and SSTIs were admitted in the NRI hospital in Surgery, Ortho and Gynecology wards every month. So, the 5 months admissions were around 200.
Sampling Procedure
Systematic random sampling technique was followed in choosing the sample- Collecting the data from every alternative record. Hence the sample size -100 was chosen.
Data Collection
Data of demographic characteristics, drug consumption, and co-morbid conditions were collected in a designed proforma.
Drug consumption was analysed by WHO drug utilization indicators8:
Average number of drugs prescribed.
Percentage of antimicrobials prescribed
Percentage of antimicrobials prescribed by generic name
Percentage of injections of antimicrobials prescribed.
Percentage of drugs prescribed from essential drug list or formulary.
Statistical Analysis
Data was expressed as numbers, percentages and mean± S.D. All the data was entered into Microsoft office 2013 version and statistically analyzed. No statistical hypothesis was tested.
Results
The data of 100 patients admitted in NRI hospital over a period of 5 months were analysed. Admissions were more in the age group below 35yrs (38 patients). Majority of the admitted patients were married.
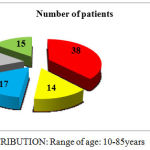 |
Graph 1: AGE DISTRIBUTION: Range of age: 10-85 years
|
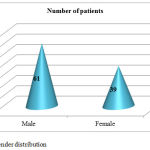 |
Graph 2: Gender distribution
|
Among 100 patients, 55 pus samples and 45 wound samples were sent for culture and sensitivity test to identify the causative organism and sensitive antimicrobials. 46 samples were negative for culture and 54 were positive with Escheria .coli as main causative organism followed by staphylococcus aureus. Total 578 drugs were prescribed to 100 patients. Among them, 201 antimicrobials were prescribed to all the patients irrespective of positivity or negativity of culture test.14 patients were prescribed topical antimicrobial also to be applied on the wound mostly in the form of hydroheal gel.
Results of WHO drug utilization indicators were as follows
Table 1: WHO drug utilization indicators
| Indicator | Result |
| Average number of drugs prescribed per patient | 5.78 |
| Percentage of antimicrobials among total drugs | 34.77% |
| Percentage of antimicrobials in generic name | 31.8% |
| Percentage of antimicrobial Injections | 42.78% |
| Percentage of antimicrobials from national list of essential medicines 2015[9] | 94.51% |
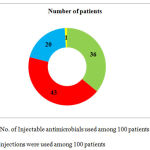 |
Graph 3: No. of Injectable antimicrobials used among 100 patients: Total 86 injections were used among 100 patients
|
For 36 patients, antimicrobial was changed basing on the culture and sensitivity report. Sensitive antimicrobial was prescribed.
The most commonly prescribed antimicrobial after obtaining the report was Inj. Amikacin followed by Inj. Augmentin.
Table 2: Diagnostic pattern of wound and skin and soft tissue infections is as follows:
| Diagnosis | No of Male patients | No of Female patients |
| 1.Abscess including liver abscess | 15 | 8 |
| 2.Post surgical wound | 9 | 5 |
| 3.Diabetic foot | 9 | 3 |
| 4.Appendicitis | 5 | 4 |
| 5.Cellulitis | 6 | 2 |
| 6.others | 17 | 17 |
| Total | 100 |
Table 3: Associated co-morbid conditions among 100 patients:
| Co-morbidity | Number of patients |
| Diabetes Mellitus | 34 |
| Hypertension | 21 |
| others | 11 |
| No co-morbidity | 34 |
The most common co morbid condition associated was diabetes mellitus.
Metronidazole is the most commonly utilized antimicrobial in both tablet and injection form followed by ceftriaxone among 201 antimicrobials used for 100 patients. Ceftriaxone is prescribed as Injection Monocef in all the cases.
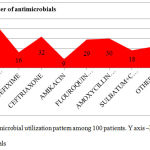 |
Graph 4: Antimicrobial utilization pattern among 100 patients. Y axis –No. of antimicrobials
|
Other drugs prescribed apart from antimicrobials
63 patients were prescribed multivitamins. Cap.Becosules (Vitamin B complex) is the most commonly prescribed followed by Tab.shelcal (Calcium supplement).
80 patients were prescribed anti ulcer agents also. Pantoprazole is the most commonly prescribed both in tablet and in injection form followed by Cap.Omeprazole. As antimicrobial therapy can lead to gastritis, Pantoprazole is prescribed along with antimicrobial to prevent ulcers.
56 patients were prescribed analgesic most commonly in the form Tab.Ultracet(Tramadol+Acitaminophen) followed by Tab.Tramadol.
Discussion
Prescriptions of 100 patients admitted in NRI hospital over a period of 5 months was analysed to know the drug utilization pattern with special emphasis on W.H.O drug use indicators. Among 100 admitted patients with wound infections and SSTIs the Mean ±SD age of the patients admitted were 32.5±7 years. Males (61%) are more when compared to females (39%) in our study which is same as the study done by Rutvij Hedamba et al.10 and contradicting with the study done by Niti Mittal Et al.11 where male and female inpatients were almost equal (50.2% and 49.8%).
Among 578 prescribed drugs, antimicrobials (201) were most commonly prescribed. This is in accordance with the study conducted by Dhamija P et al 12 in the emergency medicine ward. In the study conducted by Jacob J et al13 in Karnataka which stood at antimicrobials were 20% of the total drugs prescribed.
Metronidazole was the most commonly used antimicrobial as it covers both aerobic and anaerobic wound infections.
Antimicrobial agents were prescribed even if the culture of pus or wound swab was negative in 46 patients in the present study. Even medical students were using antibiotics as self medication practice commonly which is irrational. The study of Ramya.R et al14 proved that antimicrobials usage incidence was as high as 24% among medicos. There should be a limit to the frequent and inappropriate prescription of antimicrobials especially the newer and costlier agents. An important step to avoid this could be implementation of antibiotic restriction program. The success of this program in has been proved previously.15 Another useful strategy might be making prescription practice guidelines accessible to all the physicians before making clinical decisions.16 The use of biomarkers like Procalcitonin helps in reducing the antimicrobial misuse. It has been identified as a surrogate marker for estimating the likelihood of a bacterial infection.17
Diabetes and hypertension were the two most commonly associated co-morbid illnesses which are in accordance with the study done by Dawalji S et al.18
The median duration of stay in the hospital was 7 days in our study. In the study done by Tavallaae M et al.19 the average duration of stay is around 5 days among intensive care unit patients.
On average 5±2 drugs were prescribed for 100 patients. It is differing with the study done by Muhit MA et al.20
Percentage of drugs prescribed by their generic name was 28.8% in our study .It is contradicting with suggestions of W.H.O which advised 100%8 Generic drug prescriptions in our study was less when compared to study done by Maharani et al.21
Majority of the drugs (94.51%) were from National list of essential medicines 2015-India which is more compliant than W.H.O recommendation of 70%.
Lethal adverse events observed during the study period were nil.
Our study has few limitations. It was conducted in a single tertiary care centre, so the results cannot be extrapolated to the general population. Pharmaco-economic analysis was not done.
Conclusion
This drug utilization study has highlighted the strengths and shortcomings of the drug utilization pattern of patients admitted in a tertiary care hospital. The information derived from this research work will be handed over to the stakeholders for implementing the modifications wherever needed for the betterment of the patient and the community.
Acknowledgement
The authors would like to thank Medical Record Section, NRI hospital for their valuable help in data collection.
Conflicts of Interest
There is no conflicts of interest
Funding sources
There is no funding sources
References
- World Health Organization. Introduction to drug utilization research.1.1. Definition and domains. http://apps.who.int/medicinedocs/en/d/Js4876e/2.html
- Esposito S, Noviello S, Leone S. Epidemiology and microbiology of skin and soft tissue infections. Curr Opin Infect Dis. 2016 Apr;29(2):109-15. doi: 10.1097/QCO.0000000000000239.
CrossRef - Carratala J, Roson B, Fernandez-Sabe N, Shaw E, del Rio O, et al. Factors associated with complications and mortality in adult patients hospitalized for infectious cellulitis. Eur J Clin Microbiol Infect Dis. 2003;22:151–7.
- Lipsky B.A, Kollef M.H, Miller L.G, Sun X, Johannes R.S, Tabak Y.P. Predicting bacteremia among patients hospitalized for skin and skin-structure infections: derivation and validation of a risk score. Infect Control Hosp Epidemiol. 2010;31(8):828–37.
CrossRef - Addison K,May M.D. Skin and Soft Tissue Infections.J surgical clinics. 2009 April;89(2):403-420. https://doi.org/10.1016/j.suc.2008.09.006
CrossRef - Thomas P, Boeckel V , Gandra S,Ashok A, Caudron Q, Bryan T.G et al. Global antibiotic consumption 2000 to 2010: an analysis of national pharmaceutical sales data. The Lancet Infect Dis. 2014;14:742–50.
CrossRef
- World health organization. The Pursuit of Responsible Use of Medicines: Sharing and Learning from Country Experiences. http://apps.who.int/iris/bitstream/10665/75828/1/WHO_EMP_MAR_2012.3_eng.pdf?ua=1.
- World health organization. How to investigate drug use in health facilities http://apps.who.int/medicinedocs/en/d/Js2289e/3.1.html
- CDSCO. India. National list of essential medicines. 2015. http://apps.who.int/medicinedocs/documents/s23088en/s23088en.pdf
- Hedamba R, Doshi C, Nishita H.D. Drug utilization pattern of antimicrobial drugs in intensive care unit of a tertiary care hospital attached with a medical college. IJBCP. 2016;5(1):169-172.
CrossRef - Mittal N, Mittal R, Singh I, Shafiq N,Malhotra S. Drug Utilisation Study in a Tertiary Care Canter: Recommendations for Improving Hospital Drug Dispensing Policies. Indian J Pharm Sci. 2014 Jul-Aug;76(4):308–314.
- Dhamija P, Bansal D, Srinivasan A, Bhalla A, Hota D, Chakrabarti A. Patterns of prescription drug use and incidence of drug-drug interactions in patients reporting to medical emergency. Fundam Clin Pharmacol . 2013 Apr;27(2):231-7.
CrossRef - Jacob J, Thomas C, Naaz A, Ramasamy R, Nazeem T, Shekar S. Study of Prescription Pattern in an intensive care unit: A prospective observational study. World J of Pharmacy and Pharmaceutical Sciences. 2015;5(1):1125-32.
- Rachamanti R , Bano Z. The pattern of self-medication practice among undergraduate medical students of tertiary care hospital, Andhra Pradesh. India. IJBCP. 2017 OCT;6(12):2848-2852. DOI: http://dx.doi.org/10.18203/2319-2003.ijbcp20175206
CrossRef - Mansouri M.D, Cadle R.M, Agbahiwe S.O, Musher D.M. Impact of an antibiotic restriction program on antibiotic utilization in the treatment of community-acquired pneumonia in a Veterans Affairs Medical Center. Infection. 2011;39:53–58.
CrossRef - Westphal J.F, Jehl F, Javelot H, Nonnenmacher C. Enhanced physician adherence to antibiotic use guidelines through increased availability of guidelines at the time of drug ordering in hospital setting. Pharmacoepidemiol Drug Saf. 2011;20:162–8.
CrossRef - Schuetz P, Christ-Crain M, Wolbers M, Schild U, Thomann R, Falconnier C, et al. Procalcitonin guided antibiotic therapy and hospitalization in patients with lower respiratory tract infections: A prospective, multicenter, randomized controlled trial. BMC Health Serv Res. 2007;7:102
CrossRef - Dawalji S, Venkateshwarlu K, Thota S, Venisetty P.K, Venisetty R.K. Prescribing pattern in coronary artery disease:A prospective study. Int J Pharm Res Rev. 2014;3(3):24-33.
- Tavallaee M, Fahimi F, Kiani S. Drug-use patterns in an intensive care unit of a hospital in Iran: an observational prospective study. Int J Pharm Pract. 2010;18(6):370-6.
CrossRef - Muhit M.A, Rahman M.O, Raihan S.Z, Asaduzzaman M, Akbar M.A, Sharmin N. Cardiovascular disease prevalence and prescription patterns at a tertiary level hospital in Bangladesh. J Appl Pharm Sci. 2012;2(3):80-4.
- Maharani1 B, Lourdu A, Jafrin M, Prakash P. Priyadarshini.Prescription pattern of patients admitted in the intensive care unit of a tertiary care hospital in Puducherry, India: a cross sectional study. IJBCP. 2017 Dec; 6(12):2822-2826.
CrossRef








