Hadeel Mazin Akram, Omar Husham Ali, Nada Kadhum Omran and Alaa Omran Ali
Periodontics Department, College of Dentistry- University of Baghdad, Baghdad-Iraq.
Corresponding Author E-mail: omarhusham81@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/1295
Abstract
Background: different methods can be used to remove tissue during gingivectomy and produce a good gingival margin, the most common is the conventional gingivectomy which is done by the use of scalpel, now a day’s Laser is widely spread and can be used to perform surgeries. Materials and methods: 50 patients divided into two equal groups, Group 1 gingivectomy was done by Diode Laser, Group 2 gingivectomy was done by scalpel, plaque and gingival index were measured at 1st, 2nd and 3rd visit, swab were taken and sent foe detecting bacterial growth and biopsy were taken for histopathological examination. Group 1 show no significant differences in plaque and gingival means between the visits, the bacteriological examination showed no growth of bacteria and histological examination revealed less inflammatory cells than Group 2. Group 2 show significant differences in plaque and gingival indices between the visits. Though scalpel remains the gold standard choice in gingivectomy but Diode laser may have some advantages over it.
Keywords
Brushing; Diode; Gingivectomy; Laser; Scalpel
Download this article as:| Copy the following to cite this article: Akram H. M, Ali O. H, Omran N. K, Ali A. O. Diode Laser Versus Scalpel Gingivectomy. Biomed Pharmacol J 2017;10(4). |
| Copy the following to cite this URL: Akram H. M, Ali O. H, Omran N. K, Ali A. O. Diode Laser Versus Scalpel Gingivectomy. Biomed Pharmacol J 2017;10(4). Available from: http://biomedpharmajournal.org/?p=17976 |
Introduction
Gingivectomy is a surgical procedure of excising the unsupported gingival tissue to a level where it is attached and create a new gingival margin that is apical to the old position.1 When performing gingivectomy the biological width should not be violated which is about 2.14mm (0.97mm of epithelial attachment and 1.07 mm of the connective tissue attachment).2 This width is important to maintain gingival health and encroaching on it may lead to different consequences such as gingival recession or gingival rebound.3 Another consideration prior to perform gingivectomy is the presence of adequate zone of keratinized tissue after surgery ranging from 3-5mm.5
Different methods can be used to perform gingivectomy; of the most common are scalpel and laser. For many years, scalpel were been used in performing gingivectomy in which small surgical blades and other periodontal surgical instruments were used to cut the tissue and place the gingival margin in a more ideal position 4. Scalpel has advantages of easy to be used, precise incision with well-defined margins, the healing is fast, and there is no lateral tissue damage. While the disadvantages of scalpel are need of giving anesthesia, bleeding that result in inadequate visibility and the incision cut is not sterilized.v
LASER is an acronym for light amplification by stimulated emission of radiation.6 There are four main types of laser that are used in dentistry and they are different in the wavelengths of the emitted light energy. These types are: the Carbon dioxide laser (CO2) the Diode laser, the Neodymium: Aluminum-Yttrium-Garnet (Nd: YAG) and the Erbium: Aluminum-Yttrium-Garnet (Er: YAG).7
In our research we used the Diode laser, Diode laser is highly absorbable by hemoglobin and melanin that allows easy manipulation of soft-tissue during gingival recontouring, and improved epithelization and healing of the wound.8 During the use of laser, heat will be generated which will result in coagulation, drying and vaporization at the area of energy absorption which will prevent bleeding by sealing the blood vessels and also inhibiting the pain receptors at the incision site.9 2-6mm is the range of incision depth of diode laser.10
The better control of laser, less post-operative inflammation and pain and the improved healing in the surgical site all are the benefits of using laser in surgery.11 Soft tissue laser surgery has some disadvantages that include the high cost, buying a laser device is expensive comparing it to scalpel,12 retinal eye damage may occur to the surgeon, the dental assistant and the patient if specific protective goggles were not used 6, some researchers reported that laser is associated with poorer wound healing and greater tissue desiccation than scalpel.13
This study was done to examine the differences between using Diode laser and scalpel in performing gingivectomy, and to evaluate the differences in bacterial count in the surgical area and patient perception regarding the need of taking pain killer following the surgery and the presence of discomfort during eating and speech.
Materials and Methods
Fifty subjects with an age range from 25-45 years old had participated in this study, they were all systemically healthy, nonsmoker, and they were diagnosed as having plaque-induced gingivitis and gingival enlargement. They were divided into two groups: Group 1 includes 25 subjects in which gingivectomy was done using the Diode Laser. Group 2 with 25 subjects in which scalpel had been used to perform conventional gingivectomy. The surgeries were performed at the periodontic department in the college of dentistry- university of Baghdad. All surgeries were done after explaining to the patient the aim of our study and informed consent was taken.
Scaling and polishing were done to all the participants prior to the surgery. Plaque index (pl.I)14 and gingival index (GI)15 were measured at 1st visit before the scaling, at 2nd visit before surgery and at the 3rd visit after one week. In Group 2, periodontal pack was placed after the surgery and was removed after one week.
Microbiological samples had been collected with the use of sterile paper points from the surgical area immediately after performing gingivectomy and then sent to the microbiological lab to measure the presence or absence of bacterial growth after 24 hours and 72 hours of incubations. The tissue removed during the surgery had been sent for histopathological examination. A second biopsy was taken at the 3rd visit and also been sent to histopathological examination. Regarding the post-operative pain, at the follow up visit the patients had been asked if they needed to use any pain killer. Also they were asked about any discomfort and difficulty during speech and eating.
Results
The bacterial growth
In Group 1 and after 24 hours and 72 hours of incubation 88% of the speciments showed –ve bacterial growth (22 out of the 25) while 12% (3 from the 25) showed +ve bacterial growth as graphed in chart 1.
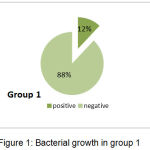 |
Figure 1: Bacterial growth in group 1 |
In group 2 all the 25 cultures showed positive bacterial growth as graphed in chart 2
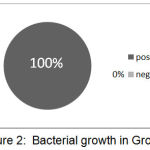 |
Figure 2: Bacterial growth in Group2 |
Pain and Discomfort
Chart 3 demonstrated that315 of 25 (60%) subjects in Group 1 experienced some pain and took analgesic for two days following the laser surgery while 21 of the 25 (84%) in Group 2 experienced pain and needed analgesic
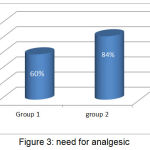 |
Figure 3: need for analgesic |
The subjects in Group 2 all experienced some discomfort in speech and eating after the surgery and before the removal of the periodontal pack, while in Group 1 none of the patient experienced any discomfort. Figure 4
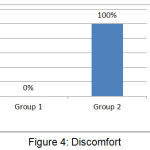 |
Figure 4: Discomfort |
Plaque and Gingival Indices
The mean of the plaque index in Group 1 was 1.22 at the 1st visit and 0.38 at the 2nd visit and 0.417 at the 3rd visit while in Group 2 it was 1.37, 0.39 and 1.31.
For the gingival index, the mean in Group 1 was 1.18, 0.449 and 0.534 at the 1st, 2nd and 3rd visits, while in Group 2 it was 1.34, 0.523 and 0.914. (Table 1)
Table 1: Descriptive statistics of periodontal parameters in the groups
| Groups | Pl.I | ||
| 1st visit | 2nd visit | 3rd visit | |
| Group 1 | 1.22 + 0.49 | 0.3 8+ 0.26 | 0.417 + 0.18 |
| Group 2 | 1.37+ 0.64 | 0.39+ 0.19 | 1.31 + 0.36 |
| GI | |||
| Group 1 | 1.18 + 0.451 | 0.449 + 0.271 | 0.534 + 0.275 |
| Group 2 | 1.34 + 0.299 | 0.523 + 0.3 | 0.914 + 0.88 |
Using the t-test, there was a high significant difference between the means of the plaque index and a significant difference in the means of the gingival index at the 2nd and the 3rd visits in Group 2, while there were no significant differences between the means of the plaque index as well as the gingival index in Group 1. (Table 2)
Histopathological Examination
The biopsy taken immediately during the conventional gingivectomy shown dense fibrous connective tissue stroma and stratified squamous epithelium while the laser biopsy showed necrotic epithelium and burning like appearance with no clear demarcation between layers.
Seven days later, second biopsies were taken, in conventional gingivectomy moderate fibrous connective tissue with dense inflammatory infiltrated cells.
In Laser the biopsies revealed densely fibrous connective tissue with fewer inflammatory cells and clearly re-epithelization suggestive of good histological healing.
Table 2: t-test between the 2nd and 3rd visits
| Periodontal parameters | Groups | 2nd visit | 3rd visit | t-test | P value | Sig. |
| Plaque index | Group 1 | 0.383 | 0.417 | -0.53 | 0.601 | NS |
| Group 2 | 0.388 | 1.305 | -11.3 | <0.001 | HS | |
| Gingival index | Group 1 | 0.449 | 0.534 | -1.09 | 0.27 | NS |
| Group 2 | 0.523 | 0.914 | -2.07 | 0.04 | S |
Discussion
Deciding whether to do a conventional gingivectomy by scalpel or to use laser depends on many factors, in our study we compared between the two methods. First of all the surgery was easier and quicker in Laser than conventional gingivectomy. Bleeding was observed in the conventional gingivectomy while relatively blood-less in laser. Less anesthesia is needed in laser gingivectomy.16
In Laser gingivectomy we found that the pain post-operatively was less compared to the pain in conventional gingivectomy this could be attributed to the heat generated by laser that inhibit the pain receptors9 and the coagulation which provided a dry and isolated environment and less infection to the wound. 17,18
A significant increase in the plaque index and the gingival index had been seen in patients with conventional gingivectomy when comparing the means at the day of the surgery and after week at the removal of the periodontal pack, this could be explained by the presence of periodontal pack which act as retentive factor for plaque leading to gingival inflammation
Histologically, in the biopsy taken after 7 days less infiltration of inflammatory cells had been seen in laser with a good improved epithelization, which result in reducing the scars and the contraction of the wound and thus improve the healing.19
References
- Mosby’s. Dental Dictionary, 2nd edition. © Elsevier. 2008
- Garguilo A., Wenz F and Orban B. Dimension and relation at the dentogingival junction in humans. Journal of periodontology. 1961;32:261-267.
CrossRef - Levine R And Mcguire M. The diagnosis and treatment of the gummy smile. Compendium. 1997;18(8):757-764.
- Allen E. Use of mucogingival surgical procedures to enhance esthetics. Dent Clinics of No Amer. 1988;23:307-330.
- Funde S., Baburaj M. D., Pimpale S. K. Comparison between Laser, Electrocautery and Scalpel in the Treatment of Drug-Induced Gingival Overgrowth: A Case Report. IJSS Case Reports & Reviews. 2015;1(10):27-30.
- Kravitz N. D and Kusnoto B. Soft tissue lasers in orthodontics: An overview. American Journal of orthodontics and dentofacial orthopaedics. 2008;133(4,1):110-114.
- The Research Science and Therapy Committee of the American Academy of Periodontology Lasers in Periodontics. J Periodontal. 2002;73:1231-1239.
CrossRef - Ozcelik O., Haytac M. C., Kunin A., Seydaoglu G. Improved wound healing by low-level laser irradiation after gingivectomy operations a controlled clinical pilot study. J Clin Periodontol. 2008;35:250-4.
CrossRef - Ize-Iyamu I. N., Saheeb B. D., Edetanlen B. E. Comparing the 810nm diode laser with conventional surgery in orthodontic soft tissue Figure 6: Initial healing after 7 days Funde, et al. Comparison between Laser, Electrocautery, and Scalpel in Drug-Induced Gingival Overgrowth 30 IJSS Case Reports & Review.Ghana Med J. 2013;47:107-11.
- Fornaini C., Rocca J. P., Bertrand M. F., Merigo E., Nammour S., Vescovi P. Nd: YAG and diode laser in the surgical management of soft tissues related to orthodontic treatment. Photomed Laser Surg. 2007;25:381-92.
CrossRef - Pirnat S., Lukac M., Ihan A. Study of the direct bactericidal effect of Nd:YAG and diode laser parameters used in endodontics on pigmented and nonpigmented bacteria. Lasers Med Sci. 2011;26:755-61.
CrossRef - Christensen G. J. Soft tissue cutting with laser versus electrosurgery. Journal of the American dental Association. 2008;139:981-984.
CrossRef - Sarver D. M and Yanosky M. Principles of cosmetic dentistry in orthodontics: Part 2. Soft tissue laser technology and cosmetic gingival contouring. American Journal of Orthodontics and Dentofacial Orthopedics. 2005;127(1):85-90.
CrossRef - Loë H. The gingival index, the plaque index and the retention index system. J Periodontal. 1967; 38(l):610.
CrossRef - Loe H. Silness: Periodontal disease in pregnancy. Acta Odontol Scand. 1963;22:533.
CrossRef - Pourzarandian A., Watanabe H., Ruwanapura S. M., Aoki A., Ishikawa I. Effect of low-level Er:YAG laser irradiation on cultured human gingival fibroblast. J Periodontal. 2005;76:187-193.
CrossRef - Haraji A., Rakhshan V. Chlorhexidine gel and less difficult surgeries might reduce post-operative pain, controlling for dry socket, infection and analgesic consumption a split-mouth controlled randomised clinical trial.J Oral Rehabil. 2014. DOI: 10.1111/joor. 12230.
CrossRef - D’Arcangelo C., Nardo D. D. F., Prosperi G. D., Conte E., Baldi M., Caputi S. A preliminary study of healing of diode laser versus scalpel incisions in rat oral tissue a comparison of clinical, histological, and immunohistochemical results. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:764–773. doi: 10.1016/j.tripleo.2006.08.002.
CrossRef - Zeinoun T., Nammour S., Dourov N., Aftimos G., Luomanen M. Myofibroblasts in healing laser excision wounds. Lasers Surg Med. 2001;28:74-9.
CrossRef







