Manuscript accepted on :October 04, 2017
Published online on: --
Bhaskaran Sathya Priya1, K. R. Srinivasan2, Purushothaman Lakshmanan3 and Panneer Selvi2
1Department of Anatomy, Sree Balaji Dental College and Hospital, Bharath Institute of Higher Education and Research, Chennai, Tamilnadu.
2Department of Anatomy, Vinayaka Missions Kirupananda Variar Medical College and Hospital, Vinayaka Missions University, Salem, Tamilnadu.
3Consultant Orthodontist, Apollo White Dental, Chennai, Tamilnadu.
Corresponding Author E-mail: dr.sathyapriyalakshmanan@yahoo.com
DOI : https://dx.doi.org/10.13005/bpj/1304
Abstract
The temporomandibular (TMJ) joints are multipart structures containing muscles, ligaments, bones and neurovascular bundle. Surgery for TMJ disorders represents a significant risk of facial nerve damage that can result in facial weakness affecting patients’ mental health, ability to communicate and self-image. This case report examined the effect of electrical stimulation in the treatment of facial palsy. A 15 year old male patient with a left sided facial palsy came with the history of TMJ surgery exactly at 7th day after surgery. The patient was functionally assessed by House Brackmann method, neurologically evaluated by strength duration (SD) curve and graded by Sunderland’s classification of peripheral nerve injury. The SD curve was plotted at 0 week and then at 1st and 2nd week after subjecting the patient to electrical stimulation, facial massage and ‘Y’ shaped facial adhesive strap. The prognosis of the patient shows the shift of the SD curve to the left which indicates near normal complete re-innervations after treating with electrical stimulator for a month. It was concluded that electrical stimulation may improve the facial paralysis and decrease the psychosocial influence on the patient.
Keywords
Electrical stimulation Facial paralysis; Strength Duration curve; Temporomandibular disorders;
Download this article as:| Copy the following to cite this article: Priya B. S, Srinivasan K. R, Lakshmanan P, Selvi P. Facial Nerve Injury Following TMJ Surgery and its Management by Electrical Stimulation - A Case Study. Biomed Pharmacol J 2017;10(4). |
| Copy the following to cite this URL: Priya B. S, Srinivasan K. R, Lakshmanan P, Selvi P. Facial Nerve Injury Following TMJ Surgery and its Management by Electrical Stimulation - A Case Study. Biomed Pharmacol J 2017;10(4). Available from: http://biomedpharmajournal.org/?p=17198 |
Introduction
Temporomandibular joint (TMJ) disorders are characterized by the incidence of pain, clicking sound and restricted mouth opening.1 TMJ disorders include disease, derangement, degeneration, hypo mobility, hyper mobility, benign/malignant tumors and trauma.
Epidemiological studies have shown that, adolescents and young adults, reported clicking sounds during energetic movement of the mandible.2 The universal causes of clicking sound are neuromuscular incoordintion of lateral pterygoid muscle, dislocation and derangement of the articular disc. However, the etiology of clicking is divisive; it is not known whether it’s due to undisruptive situation3-4 or due to internal derangement of the TMJ.5-6
Despite the surgical management of TMJ disorders, there are possible complication which comprise internal bleeding, disease, auriculo-temporal (ATN) nerve syndrome, ear pathology, parotid gland tumor,12 and damage to the facial or VII cranial nerve.7-12 The facial nerve is mixed cranial nerve comprising both sensory and motor components. The motor branch arise from pons while the sensory branch arise from the nervus intermedius and emerge from the brainstem and enters petrous part of the temporal bone into the internal auditory meatus and forms the geniculate ganglion prior to entry into the facial canal. After passing through the canal, it comes out through the stylomastoid foramen and runs throughout substance of the parotid gland and divides into five terminal branches. It has an important function on facial aesthetics by enabling the movements of mimic muscles, and it is the most damaged nerve among the cranial nerves after leaving the central nervous system.13 Eating, drinking and speaking difficulties are observed in peripheral facial nerve damages, as well as difficulties in expressing the feelings.
The nerve supplies the muscles of facial expression, the posterior belly of the digastric muscle, the stylohyoid muscle, and the stapedius muscle developing from hyoid arch. It provides secretomotor supply to the submandibular and sublingual salivary glands.
The temporal and zygomatic branches of the facial nerve are highly susceptible for damage during TMJ surgery.14 The functional integrity of facial nerve should be preserved during TMJ surgery.15 There are many factors that could contribute to the injury of the temporal and zygomatic branches of the facial nerve.16 These nerves lie in a confluence of superficial fascia, temporalis fascia, and periosteum, and may be damaged during surgical approach. Undue retraction causes compression and/or stretching of nerve fibres resulting in neuropraxia which forms the basis for the nerve injuries associated with TMJ surgery.17
Treating facial paralysis in early period with a multidisciplinary approach is important for speeding up the recovery process.18 In addition to medical therapy, thermal heat modalities, electrical stimulation, exercise and massage are physical therapy methods of which the effectiveness were shown.18
Aim and Objective
The aim of the present study is to detect the facial nerve injury following TMJ surgery and its prognosis by electrical stimulation with the case report.
Materials and Methods
A 15 year old male patient with a left sided facial paralysis came to the hospital with the history of TMJ surgery exactly at 7th day after surgery. After receiving informed consent from the parents of the patient, the neurological signs of the patient were assessed at 0, 1 & 2 weeks by the following methods:
Functional assessment
Strength – Duration Curve
Functional assessment
The patient was functionally assessed by
The House-Brackmann method ( Table-1)
Sunderland’s classification ( Table-2)
The House-Brackmann method is the conventional method for the clinical assessment of facial nerve function. It is prejudiced and sporadic, prone to inter-observer disparity.
Table 1: House-Brackmann Classification of Facial Function
| Grade | Characteristics |
| I | Normal facial function |
| II | Mild dysfunction |
| III | Moderate dysfunction |
| IV | Moderately severe dysfunction |
| V | Severe dysfunction |
| VI | Total paralysis |
Sunderland’s Classification
Table 2: Degree of peripheral nerve injury by Sunderland’s classification
| 1st degree | 2nd degree | 3rd degree | 4th degree | 5th degree | |
| Electro-diagnosis | Conduction block | Axon loss | Axon loss | Axon loss | Axon loss |
| Pathology | Demyelination | Only axon loss | Disrupted endoneurium | Disrupted endoneurium & perineurium | Disrupted endoneurium, perineurium and endoneurium |
| Prognosis | Excellent
2-3 month |
Slow
Dependent on sprouting |
Slow may fail because of misdirected sprouts | Unlikely w/o surgery | Impossible w/o surgery |
Strength – Duration (SD) Curve
The plotting of strength duration curve indicates the strength of impulse of various duration required to produce contraction in a muscle. It is easy and consistent. It shows the percentage of denervation. It cannot indicate the site of nerve lesion.
Procedure
The SD curve was plotted at 0 week and then the patient was subjected to electrical stimulation, facial massage and ‘Y’ shape facial adhesive strap.
A nineteen year old male patient with a left sided facial paralysis after TMJ surgery was assessed for neurological signs at 0, 1 & 2 weeks by the following methods in this case study.
Functional assessment
Strength duration curve
Functional assessment
The House-Brackmann method was clinical assessment of facial nerve function. The following observations were made in the study (Table 3).
Table 3: Clinical assessment of facial nerve function using House-Brackmann method
| S.No | Clinical Signs | Present / Absent |
| 1. | Facial asymmetry | Present |
| 2. | Wrinkling of forehead | Absent |
| 3. | Closure of eyes | Absent |
| 4. | Frowning | Absent |
| 5. | Dribbling of saliva | Present |
| 6. | Flat nasolabial furrow | Present |
| 7. | Blowing of cheek | Absent |
| 8. | Deviated angle of mouth | Present |
| 9. | Bell’s phenomenon | Present |
Strength Duration Curve
The graph represents the interdependence between the stimulus strength and the time required in activating the muscles. It also indicates the strength of impulses of various durations necessary to generate muscle contraction by joining the points that graphically represent the threshold value along the ordinate for various durations. This SD curve was plotted at 0, 1 and 2 weeks following postsurgical facial paralysis.
SD Curve at 0 Week
When all the nerve fibre supplying a muscle has degenerated, the strength duration produced is characteristic of complete denervation. For all impulses with duration of 100 ms or less the strength of the stimulus must be amplified each time the duration is reduced and no reaction is recorded to impulses of very short duration. The curve rises sharply and moves to the right than that of normally innervated muscle. The plotted SD curve showed that the facial nerve is at the state of 3rd degree injury according to Sunderland’s classification. (Figure 1)
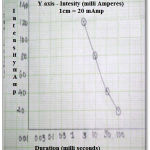 |
Figure 1: SD curve at 0 week
|
The patient was then subjected to electrical stimulation using an electrical stimulator with diagnostic interrupted Galvanic current facility (Figure2), facial massage and “Y” shaped facial adhesive strap (Figure 3) to prevent the over stretching of the angle of the mouth. The current was passed to the patient through two small electrodes – Active electrode (nape of the neck) and Inactive electrode (motor points of the facial muscles). First the Faradic current was applied to the patient and observed for the contraction which was absent in this case. Next the galvanic current was applied after which the contraction was observed. This process was repeated for each length of the stimulus in turns, the magnitude being increased. The SD curve was plotted from the outcome of the investigation.
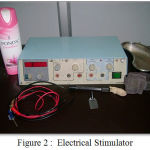 |
Figure 2: Electrical Stimulator
|
 |
Figure 3: Adhesive Strap
|
SD Curve at 1st Week
SD curve plotted after 1 week shows the slight shift of the curve towards left which indicates the slight progression of the re- innervations after electrical stimulation (Figure 4).
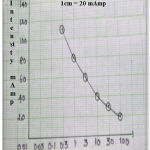 |
Figure 4: SD curve at 1st week
|
SD Curve at 2nd Week
Longer duration impulse – contraction was recorded with the stimulus of low intensity. As the impulses are shortened, some fibres respond less readily, so that a stronger stimulus was applied to produce a perceptible contraction and the curve rises steeply like that of the denervated muscle.
Shorter duration impulse – some fibres respond to a weaker stimulus than that necessary for the denervated fibres, so that the contraction of denervated fibres was not obtained and this part of the curve is similar to that of the innervated muscle.
Thus the right side of the curve is similar to denervated muscle, the left side of the curve is similar to innervated muscle, and the bend is seen at the junction of the two (Figure 5).
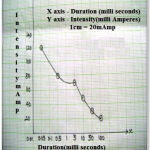 |
Figure 5: SD curve at 2nd week
|
Prognosis
The prognosis of the patient was assessed after treating with an electrical stimulator for a month. The SD curve plotted shows the shift of the curve to the left which indicates near normal complete re- innervations (Figure 6).
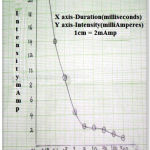 |
Figure 6: SD curve after a month
|
Discussion
A male patient with a left sided facial paralysis came to the hospital with the history of TMJ surgery exactly at 7th day after surgery. The patient was functionally assessed by House Brackmann method, neurologically evaluated by strength duration curve and graded by Sunderland’s classification of peripheral nerve injury. Choosing between the treatment methods is one of the important points together with the paralysis diagnosis. The most efficient treatment strategy is still controversial.19 The treatment may be planned with the determination of the disease period, actual lesion site and the exact degree of damage in the nerve. Physical methods are used in facial paralysis treatment along with medical therapy which include thermal therapies, electrical stimulation, exercise, massage, biofeedback and acupuncture therapy.20
In this case study the SD curve was plotted at 0 week and then at 1st and 2nd week after subjecting the patient to electrical stimulation, facial massage and ‘Y’ shaped facial adhesive strap. The prognosis of the patient was assessed after treating with electrical stimulator for a month. At 0 week no reaction was recorded to impulse of extremely small duration and the curve rises sharply and is further to the right than that of the normally innervated muscle. It also showed that the facial nerve is at the state of 3rd degree injury according to Sunderland’s classification. Studies on the successful results of the long-term electrical stimulation in sub acute and chronic period of facial paralysis were seen in literature.21-24
Alakram et al applied hot application, massage and exercise program to one group and electrical stimulation to the other in their study and reported that there were improvements in both groups which co-relates with our current case study.25
The prognosis of the patient shows the shift of the SD curve to the left which indicates near normal complete re-innervations after treating with electrical stimulator for a month. The physical therapies like electrical stimulation, facial massage and facial strapping are important in terms of speeding-up the recovery process and decreasing the psychosocial influence on the patient.
Conclusions
The facial nerve injury is associated to the complexity implicated in TMJ surgery. The nerve lesion was shown to be temporary in nature. Care should be taken while doing TMJ surgery because of its varied complications one of which is facial nerve injury This case study proves that the patient display a near normal function of the facial nerve by subjecting patient to electrical stimulation, facial strapping and massage.
Acknowlegment
Subject of this Study
Conflict of Interest
Nil
Source of Funding
Self
References
- Schwartz L.L, Cobin H.P. Symptoms associated with the temporomandibular joint: a study of 491 cases. Oral Surg Oral Med Oral Pathol. 1957;10:339–44.
CrossRef - Wänman A, Agerberg G. Temporomandibular joint sounds in adolescents: a longitudinal study. Oral Surg Oral Med Oral Pathol. 1990;69:2-9.
CrossRef - Gross A, Gale E.N. A prevalence study of the clinical signs associated with mandibular dysfunction. J. Am Dent Assoc. 1983;107:932-36.
CrossRef - Greene C.S, Laskin D.M. Long-term status of TMJ clicking in patients with myofascial pain and dysfunction. J. Am Dent Assoc. 1988;117:461-65.
CrossRef - Dolwick M.E. Internal derangement of the temporomandibular joint: fact or fiction? J Prosthet Dent. 1983;49:415-18.
CrossRef - Brooke R.I, Grainger R.M. Long-term prognosis for the clicking jaw. Oral Surg Oral Med Oral Pathol. 1988;65:668-70.
CrossRef - Marciaini R, Ziegler R. Temporomandibular joint surgery, a review of fifty-one operations.Oral Surg Oral Med Oral Pathol. 1983;56:472–6.
CrossRef - Peoples J, Euzenio G, Dion J. Management of internal maxillary artery hemorrhage from TMJ surgery via selective embolization. J. Oral Maxillofac Surg. 1988;46:1005–7.
CrossRef - Eppley B, Delfino J.Use of prophylacticantibiotics in temporomandibular joint surgery. J. Oral Maxillofac Surg. 1985;43:675–9.
CrossRef - Kryshtalskyj B, Weinberg S. An assessment for auriculotemporal syndrome following temporomandibular joint surgery through the preauriclar approach. J. Oral Maxillofac Surg. 1989;47:3–6.
CrossRef - Sickles V.J, Nishioka G, Hegewold M, Neal G. Middle ear injury resulting from temporomandibular joint arthroscopy. J. Oral Maxillofac Surg 1987;45:962–5.
CrossRef - Epker B, Burnette J. Trauma to the parotid gland and duct: primary treatment and managementof complication. J. Oral Surg. 1970;28:657–70.
- Teixeira L.J, Soares B.G, Vieira V.P, Prado G.F. Physical therapy for Bell’s palsy (idiopathic facial paralysis).Cochrane Database Syst Rev. 2008;16(3):CD006283.
- Dolwick M.F, Kretzschmar D.P. Morbidity associated with the preauricular and perimeatal approaches to the temporomandibular joint. J. Oral Maxillofac Surg. 1982;40:699–700.
CrossRef - Winberg S, Kryshtalskyj B. Analysis of facial and trigeminal nerve function after arthroscopic surgery of the temporomandibular joint. J. Oral Maxillofac Surg. 1996;54:40–3.
CrossRef - Weinberg S, Kryshtalskyj B. Facial nerve function following temporomandibular joint surgery using the preauricular approach. J. Oral Maxillofac Surg. 1992;50:1048–51.
CrossRef - Ellis III E, McFadden D, Simon P, Throckmorton G. Surgical complication with open treatment of mandibular condylar process fracture. J. Oral Maxillofac Surg. 2000;58:950–8.
CrossRef - Paternostro-Sluga T, Herceg M, Frey M. Conservative treatment and rehabilitation in peripheral facial palsy. Handchir Mikrochir Plast Chir. 2010;42(2):109-14.
CrossRef - Chen N, Zhou M, He L, Zhou D, Li N. Acupuncture for Bell’spalsy. Cochrane Database Syst Rev. 2010;(8):CD002914.
- Hyvarinen A, Tarkka I.M, Mervaala E, Paakkönen A, Valtonen H, Nuutinen J. Cutaneous electrical stimulation treatment in unresolved facial nevre paralysis. Am J Phys Med Rehabil. 2008;87:992-7.
CrossRef - Narin S, Barutçu A. Treatment of prolonged Facial with Temporalis Myoplasty and Electrical Stimulation. Journal of Neurological Sciences. 2011;29(4):513-519.
- Shafshak T.S. The treatment of facial palsy from the point of view of physical and rehabilitation medicine. Eura Medico phys. 2006;42(1):41-7.
- Targan R.S, Alon G, Kay S.L. Effect of long-term electrical stimulation on motor recovery and improvement of clinical residuals in patients with unresolved facial nevre palsy. Otolaryngol Head Neck Surg. 2000;122(2):246-52.
CrossRef - Teixeira L.J, Soares B.G, Vieira V.P, Prado G.F. Physical therapy for Bell’s palsy (idiopathic facial paralysis). Cochrane Database Syst Rev. 2008;16(3):CD006283.
- Alakram P, Puckree T. Effects of electrical stimulation on House-Brackmann scores in early Bell’s palsy. Physiother Theory Pract. 2010;26(3):160-6.
CrossRef







