Batool Teimoori1, Marzie Ghasemi1 , Alireza Jahangirifard2 , Maziar Mahjoubifard3*, Hassan Enayati3, and Tahere Ostadmahmoodi3
1Department of Obstetrics and Gynecology, Health Promotion Research Center, Zahedan University of Medical Sciences, Zahedan, Iran.
2Shahid Beheshti University of Medical Sciences, Tehran, Iran.
3Zahedan University of Medical Sciences, Zahedan, Iran.
Corresponding Author Email: m_mahgobifard@yahoo.com
DOI : https://dx.doi.org/10.13005/bpj/1037
Abstract
WHO estimates 585,000 maternal deaths per year among which 25% is directed by partum hemorrhage. The average volume of bleeding is supposed to be around 500 ml in natural vaginal childbirth while 1000 ml through caesarean section. Regarding much more recent demands for caesarean section, there have been obvious attempts to get effective harm reduction of this surgery by decreased bleeding through several strategies such as selecting more perfect and ideal techniques of anesthesia. Through a randomized controlled trial in 2013, all the elective CS referrals to a university hospital in Zahedan with 38-40 weeks gestational age enrolled via easy sampling before being divided into two groups of general and spinal anesthesia. Patients' hemoglobin and HCT in addition to blood pressure were the major factors which were checked and compared between the groups. HB fell significantly more in patents with general anesthesia, especially at the range of 1-2 g/dl after 6 and 24 hours of CS. Around 91% of GA and more than 50% of SA had middle changes in HB and HCT. These changes were significantly different between GA and SA. The two groups were simply similar according to greater changes including 2-3 g/dl in HB or 6-9 in HCT and contain a minor part of the patients. The present study indicated that bleeding and decreased HB and HCT occur significantly less in spinal anesthesia comparing to general anesthesia. It would need more trials to assess the role of personal conditions in patients and surgeons as well as newer techniques and medications dynamically as well.
Keywords
Caesarean Section; General Anesthesia; Spinal Anesthesia; Hemoglobin; Hematocrit
Download this article as:| Copy the following to cite this article: Teimoori B, Ghasemi M, Jahangirifard A, Mahjoubifard M, Enayati H, Ostadmahmoodi T. Comparison of General and Spinal Anesthesia on Maternal Hemoglobin Changes after Caesarean Section. Biomed Pharmacol J 2016;9(3). |
| Copy the following to cite this URL: Teimoori B, Ghasemi M, Jahangirifard A, Mahjoubifard M, Enayati H, Ostadmahmoodi T. Comparison of General and Spinal Anesthesia on Maternal Hemoglobin Changes after Caesarean Section. Biomed Pharmacol J 2016;9(3). Available from: http://biomedpharmajournal.org/?p=11751 |
Introduction
Obstetrical hemorrhage belongs to main global causes of morbidity and mortality (1). This is prominent in developing countries and WHO estimates 585,000 maternal deaths per year among which 25% is directed by partum hemorrhage (2). The average volume of bleeding is supposed to be around 500 ml in natural vaginal childbirth while 1000 ml through caesarean section (3). Severe bleeding (>10% decreased HCT) occurred usually in 4% of vaginal and 6% of caesarean cases (4,5). Regarding much more recent demands for caesarean section, there have been obvious attempts to get effective harm reduction of this surgery by decreased bleeding through several strategies such as selecting more perfect and ideal techniques of anesthesia (6-11). Race, labor disturbances, preeclampsia, amnionitis, and history of previous labor bleeding are the main causes of bleeding in caesarean section and these factors in addition to mother preference help physicians make decision to operation general or spinal anesthesia (12,13). Evidence for maternal death in CS, especially due to excessive bleeding is rare and general anesthesia is not often considered in this regard. This is because of muscle relaxation and much less labor induction against spinal method (14). Furthermore, inhaled halogen contents in general anesthesia may induce more bleeding via suppression in uterine wall contraction and mother’s consciousness (15). Although both general and spinal anesthesia are used in elective cases of CS, the latter is much preferred, particularly when they need to keep mother awake (16,17). Besides, mother aspiration and fetal distress would effectively reduce by spinal technique (13,18,19). Previous studies show a dilemma about labor bleeding and its causes when compare general and spinal anesthesia although the majority of authors determine more bleeding in general technique (20). A study in 1987 showed that the used medications in general anesthesia decreased patients’ HCT 8-30 % (21). Another trial in 1999 in Thailand experienced significant HCT fall after general anesthesia in US. Unlikely, Hong and colleagues who realized that there was no difference between general and epidural anesthesia in terms of bleeding volume in CS (21).
According to the controversy for the best anesthetic technique to achieve the most perfect efficacy and the least side effects such as bleeding, the present study aimed to compare general against spinal anesthesia concerning their hemodynamic consequences to make decisions easier for patients and surgeons.
Materials and Methods
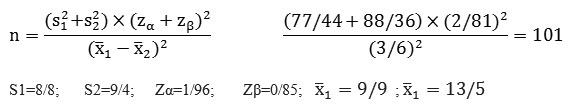
Through a randomized controlled trial in 2013, all the elective CS referrals to a university hospital in Zahedan with 38-40 weeks gestational age enrolled via easy sampling before being divided into two groups of general and spinal anesthesia. Patients had had at most 5 gravidity and 4 parity with current cephalic single pregnancy and normal fetus, placenta and amniotic condition in their 18-36 years of age. Patients who had uterus atony or its risk factors, eclampsia, coagulopathies, premature detachment of the placenta, emergency CS, birth weight > 4 kg and operation time > 90 minutes were excluded from the study. Preterm delivery, cardiac problems, anemia, uterus myoma, placenta previa, drug abuse and drug sensitivity were considered as exclusion criteria as well. Each group of the trial was supposed to contain 101 patients regarding the following sample size equation:
Patients were randomly recruited in the two groups using random codes after getting necessary explanation about the aim, the process and the importance of the performance.
Outcome Measures
Patients’ hemoglobin and HCT in addition to blood pressure were the major factors which were checked and compared between the groups since they are the early factors affected by acute blood loss. Any changes in HB and HCT after 0, 6, and 24 hours following operation were important in this regard.
Anesthesia Techniques
All patients were given one liter intravenous ringer solution during 8 hours before arriving operation room. Blood pressure and heart rate were monitored immediately after setting peripheral IV line at the operation room before anesthesia started. Then, IV ringer lactate was started with 3 ml/ Kg in both groups. In general anesthesia group (GA) oxygenation was used for 5 minutes at 6 lit/min before anesthesia induction with 5mg/ kg thiopental Na. Succinyl with 1.5 mg/kg dose was used for tracheal intubation. Anesthesia was maintained by a gas combination of 50% O2, 50% NO and 0.5% halothane. Fentanyl (1µg/kg) and 10-30 µg/kg midazolam plus 30 units of oxytocin were infused after childbirth. In the other group (SA) patients experienced a spinal subarachnoid injection of 12.5 mg of 0.5% bupivacaine through a 25 gauge spinal needle at L2-L3 or L3-L4 level at sitting position. Patient got immediately supine position and the operation started when the block completed in 30-60 seconds. Intravenous crystalloids were ordered 3cc for each 1cc blood loss. All the operations were done by single surgeon in two groups.
Statistics
Quantitative data were reported using central tendency indices through student t-test while Chi-square test was used in the case of qualitative reports. This study considered 95% confidence interval with 0.05 type one error and significance of P<0.05.
Ethics
Patients were given comprehensive explanation about the aims and the importance of the trial as well as the steps of it before signing their written consents to attend the study. The personal and private data were kept carefully by the principal investigators. There was no ethical issue throughout the study since the both anesthesia techniques are globally demanded yet by patients and physicians.
Results
Total 220 pregnant women enrolled the trial with the mean age of 27.62 ± 5.02 years. The mean gestational age was 38.71 ± 0.49 weeks. There was no difference between the groups in terms of age, BMI, parity and gestational age, operation time length, number of previous CS, and preoperative HB as presented in table 1. Table2 shows that HB fell significantly more in patents with general anesthesia, especially at the range of 1-2 g/dl after 6 and 24 hours of CS. HB fell 1-2 g/dl in 101 (91.8%) of GA group which doubled in number as compared with SA group (54-60%)(P<0.001). The changes in HCT were similarly significant in the groups with more decrease in GA cases (P<0.001) as seen in table 3.
Table 1: Age, gravid, parity and gestational age of all the patients
| Variable | Number (%) | |
| Age | 15-20 | 24 (10.9) |
| 21-25 | 60 (27.3) | |
| 26-30 | 72 (32.7) | |
| 31-35 | 54 (24.5) | |
| 36-40 | 10 (4.5) | |
| Gravid | 1 | 1 (0.5) |
| 2 | 49 (22.3) | |
| 3 | 90 (40.9) | |
| 4 | 49 (22.3) | |
| 5 | 31 (14.1) | |
| Parity | 1 | 59 (26.8) |
| 2 | 106 (48.2) | |
| 3 | 37 (16.8) | |
| 4 | 18 (8.2) | |
| Gestational Age | 38 weeks | 146 (63.4) |
| 39 weeks | 74 (36.6) | |
Table 2: HB changes in the studied groups at two time points of assessment
| Group | HB decrease
Time point |
< 1g/dl
N (%) |
1-2 g/dl
N (%) |
2-3 g/dl
N (%) |
| GA | 6 hours | 7 (6.4) | 101 (91.8) | 2 (1.8) |
| 24 hours | 4 (3.6) | 101 (91.8) | 5 (4.5) | |
| SA | 6 hours | 48 (43.6) | 60 (54.5) | 2 (1.8) |
| 24 hours | 40 (36.4) | 66 (60) | 4 (3.6) | |
| Significance | < 0.001 | |||
Table 3: HCT changes in the studied groups at defined time assessment points
|
Group |
HCT decrease
Time |
< 3
N (%) |
3-6
N (%) |
6-9
N (%) |
| GA | First 6 hrs. | 7 (6.4) | 100 (90.9) | 3 (2.7) |
| First 24 hrs. | 3 (2.7) | 102 (92.7) | 5 (4.5) | |
| SA | First 6 hrs. | 47 (43.6) | 58 (52.7) | 5 (4.5) |
| First 24 hrs. | 39 (35.5) | 63 (57.3) | 8 (7.3) | |
| P value | <0.001 | |||
When time is concerned, table 4 and 5 show that the majority of the patients had a rather stability in the fell HB and HCT which occurred at first 6 hours of operation. Around 91% of GA and more than 50% of SA had middle changes in HB and HCT (1-2 g/dl and 3-6 units, respectively). The changes were somehow stable after 24 hours. These changes were significantly different between GA and SA (P < 0.001). The two groups were simply similar according to greater changes including 2-3 g/dl in HB or 6-9 in HCT and contain a minor part of the patients. HB mild reduction (< 1g/dl) occurred in 6.4 % of GA and 43.6% of SA group.
Table 4: Time-based HB fall after CS in two groups
| Time | Tachnique | < 1 g/dl
N (%) |
1-2 g/dl
N (%) |
2-3 g/dl
N (%) |
Significance |
| First 6 hrs. | GA | 7 (6.4) | 100 (90.9) | 3 (2.7) | < 0.001 |
| SA | 48 (43.6) | 60 (54.5) | 2 (1.8) | ||
| First 24 hrs. | GA | 4 (3.6) | 101 (91.8) | 5 (4.5) | < 0.001 |
| SA | 40 (36.4) | 66 (60) | 4 (3.6) |
Table 5: Time-based HCT changes in two groups
| Time | Technique | < 3
N (%) |
3-6
N (%) |
6-9
N (%) |
Significance |
| First 6 hrs. | GA | 7 (6.4) | 100 (90.9) | 3 (2.7) | < 0.001 |
| SA | 47 (43.6) | 58 (52.7) | 5 (4.5) | ||
| First 24 hrs. | GA | 3 (2.7) | 102 (92.7) | 5 (4.5) | < 0.001 |
| SA | 39 (35.5) | 63 (57.3) | 8 (7.3) |
Discussion
The present study confirms that spinal anesthesia in CS results obviously in less blood loss and HB and HCT fall when compared with general anesthesia, especially at first 6-24 hours of the operation. Many studies have been done to assess blood loss after CS through different techniques of anesthesia among which lertakyamanee’s work in 1999 obtained the same findings we got (20). They studied 341 pregnant women in Thailand to assess HB and HCT reduction following general and spinal anesthesia. In 1994 Naef et al. had found also a prognostic role for the techniques of anesthesia in blood loss and hemodynamic changes (12) despite their work does not exactly support our significant results. The superiority of local spinal anesthesia was explained later in 2011 in Taiwan when Chang and colleagues attributed 10-time bleeding rate to general anesthesia in comparison with spinal technique (22). A research work studied 3052 CS cases to find the causes of bleeding and showed 4.6% severe bleeding rate (>10% HCT fall) while general anesthesia was among main causes (23). On the contrary, Hong et al. in 2003 in South Korea found no difference between GA and SA in maternal hemodynamic changes (24) disregarding different race, patients characteristics, used medications and the details of the techniques between their work and ours. Halogenated medications which are often used in general anesthesia are usually blamed for increased bleeding by many authors in the past century (21,25). However, low dose halothane does not increase the risk of bleeding in GA as Hood et al. realized in 1990 (15). In the United States, 93% of total CS is done under local anesthesia and maternal death rate and other complications are rare as authors report (26). In Britain, a KAP study showed that 63% obstetricians prefer local anesthesia against 5% who prefer general anesthesia and 32% who devolve it to patients (27).
To sum up, the present study indicated that bleeding and decreased HB and HCT occur significantly less in spinal anesthesia comparing to general anesthesia. It would need more trials to assess the role of personal conditions in patients and surgeons as well as newer techniques and medications dynamically as well.
References
- Jeong Ek,Ji HL,Eun JK ,Myung WM , Jong SB, Sang GL.The effect of type of anesthesia on intra and post operative blood loss at elective cesarean section . Korean J Anesthesiol 2012; 62(2):125-129.
- Dias de Souza JP, Duarte G, Basile-Filho A. Near-miss maternal mortality in developing countries. Eur J Obstet Gynecol Reprod Biol 2002; 104(1):80.
- Pritchard JA, Baldwin RM, Dickey JC, Wiggins KM. Blood volume changes in pregnancy and the puerperium. Am J Obstet Gynecol 1962; 84: 1271-82 4.
- Combs CA, Murphy EL, Laros Jr PK. Factors associated with post partum hemorrhage with vaginal birth. Obstet Gyncol 1991; 77: 69-76.
- Combs CA, Murphy EL, Laros Jr PK. Factors associated with post partum hemorrhage with Cesarian deliveris. Obstet Gyncol 1991; 77: 78-82.
- Cuningham FG, Williams J.Williams obstetrics. 21st New York: trident press.2001.chap 26.
- Robert K, Miller RD. Basics of anesthesia. 4th New York: Churchil living stone. 1996:458-62
- Robert k, Stephen S, Dierelorf F. Anesthesia and lo-existing disease.4th New York: Churchil living stone. 2002:539-9.
- Prendivile W, Elbourne D. Care during the third stage of labour: In Chalmers I, Enkin M, Keirse MJNC. Effective care in pregnancy and child birth. Oxford University Press 1989; 1145-69.
- Keirse MJNC, Renfrew MJ, Nilson JP, Crowther C. Cochrane database of systemic reviews pregnancy and child birth module. The Cochrane Collabration. Oxford: update software 1995; 2:2999-5352.
- Cunningham FG, Lenovo Kj, Bloom SL, Hauth JC, Gilstrap L, Wenstron KD.Williams 20th edition. New York: trident press. 1997. Chap 26.
- Naef RW, Chauhan SP, Roberts WE, Meydreh EF, Morrison JC. Prediction of hemorrhage at cesarean delivery. Obstet gynecol 1994; 83(6): 923-6.
- Hawkins JL , Koonin LM, Palmer SK, Gibbs CP. Anesthesia-related deaths during obstetric delivery in the united states,1979_1990. Anesthesiol 1997; 86:277.
- Lao TT, Halpern SH, Crosby ET. Anestesia and blood loos in preterm cesarean section: comparison beetween general and regional International J of obstetric Anesthesia 199; 2:85-88.
- Hood DD, Holubec DM. Elective repeat cesarean section. Effect of anesthesia type on blood loos. OJ reprod Med. 1990; 35(4):368-72.
- Kanepp NB, Kumar S, Shelley WC. Fetal and neonatal hazards of maternal hydration with 5% deyrose before cesarean section. Lancet 1982; 1:1150-4.
- Ramanathan S, Grant GJ. Vasopressor therapy for hypotention due to epidural anesthesia for cesarean Acta anaesthesiol scand 1988; 32:559-563.
- American College of obstetricians and gynecologists. Optimal goals for anesthesia care in obstetrics. Acog committee opinion 256. Washington DC: American college of obstetricians and gynecologists; 2001.
- Lam DT, Ngan KD, Khaw KS. Extension of epidural blocade in labour for emergency caesarean using 2% lidocaine with epinephrine and fentanyl, with or without alkalinisation. Anaesthesia 2001; 56:790.
- lertakyamanee J, Chinachoti T, Tritrakarnt M, Muangkasem J, Omboonnanonda A, Kolatat T. Comparison of general and regional anesthesia for cesarean section:Success rate,blood loss satisfaction from a randomized J Med Assoc Thai 1999:82(7):672-80.
- Gilstrap LC, Hauth JC, Hankins GD,Patterson Effect of aype of anesthesia on blood loss at cesarean section. Obstet gynecol 1987; 69 (3): 328-32.
- Chang CC, Wang IT, Chen YH, Lin HC. Anesthetic management as a risk factor for post partum hemorrhage after cesarean deliveries. Am J obstet Gynecol 2011; 205(5):462.e 1-7.
- Combs CA, Murphy EL, Laros RK. Factors associated with hemorrhage in cesarean deliveries. Obset gynecol 1991; 17:77-82.
- Hong JY, Jee YS, Yoon HJ, Kim Comparison of general and epidural anesthesia in elective cesarean section for placenta previa totalis: maternal hemodynamics,blood loss and neonatal outcome. Int J obstet anesth 2003; 12(1):12-6.
- Wiliam w, Andrews S, Susan M, Mark RC. Shearer MB, Black S, Wallace DH. Effect of type of Anesthesia on blood loss at elective repeat cesarean section. Amer j perinatol 1992; 9 (3); 197-200.
- Chan YL, Wong KL, Lin CF. View of patients who refuse regional Anesthesisiol 1998; 36(2):99-102.
- Gajraj NM, Sharmask, Souter AJ. A survey of obstetric patients who refuse regional anesthesia. Anesthesia1995; 50(8):740-1.








