Alireza Kamali1 , Fateme Seidi2 , Maryam Shokrpour2* and Mehri Jamilian2
1Department of Anesthesiology, Arak University of Medical Sciences, Arak Iran.
2Department of Gynecology, Arak University of Medical Sciences, Arak, Iran.
Corresponding Author Email: Maryam_shokrpour@yahoo.com
DOI : https://dx.doi.org/10.13005/bpj/1034
Abstract
Curettage is a common procedure in gynecology. In order to sedate and reduce postoperative pain, different analgesic techniques have been proposed. The objective of this study was to compare the level of sedation and postoperative pain in patients submitted to curettage, using Ketamine vs Fentanyl to lidocaine for para-cervical block. In this double blind clinical trial study, 120 eligible women candidated for curettage were enrolled. The subjects were divided to three equal groups. In first group, 5ml lidocaine 1.5% plus 1ml Fentanyl, in the second group 5ml lidocaine 1.5% plus 1 ml Ketamine, and in third group 5ml lidocaine 1.5% plus 1cc normal saline as placebo was administrated for para-cervical block. The postoperative pain was evaluated within 0-30 and 60 minutes after operation via visual analogue scale (VAS), time of analgesic request in 24hours were recorded. The VAS score within 0 and 30 minutes after procedure was lower in Ketamine and Fentanyl groups than placebo (p<0.05), but in 60 min was lower in ketamine than fentanyl (p<0.05). The time of analgesic request was longer in ketamine group (p<0.05). Ketamine and Fentanyl are effective for improving post-operative pain, but Ketamine is more effective.
Keywords
Curettage; Ketamine; Fentanyl; Post-operative Pain
Download this article as:| Copy the following to cite this article: Kamali A, Fateme Seidi F, Shokrpour M, Jamilian M. Comparing the Effects of Adding Fentanyl vs Ketamine to 1/5% Lidocaine in Para-cervical Block in Order to Reduce of Post-operative Pain Among the Patients Applying for Curettage. Biomed Pharmacol J 2016;9(3). |
| Copy the following to cite this URL: Kamali A, Fateme Seidi F, Shokrpour M, Jamilian M. Comparing the Effects of Adding Fentanyl vs Ketamine to 1/5% Lidocaine in Para-cervical Block in Order to Reduce of Post-operative Pain Among the Patients Applying for Curettage. Biomed Pharmacol J 2016;9(3). Available from: http://biomedpharmajournal.org/?p=11725 |
Introduction
Curettage is one of the most common gynecologic operations in Iran and in the whole world. As many as 660 thousand curettages were carried out in the U.S. in 2003 within the first three months of pregnancy (1). To cause and create anesthesia and analgesia among these patients, methods such as general, local or para-cervical block anesthesia are used. General anesthesia usually results in high bleeding, uterine trauma, or even death due to hypoventilation and aspiration. As a result, only 10% of clinics utilize general anesthesia, while 58% use local anesthesia with/without oral treatment and 32% use intravenous sleeping drugs along with local anesthesia (2). One of the available techniques is para-cervical block. Para-cervical block prevents pain transfer. Sympathetic and parasympathetic sensory fibers are placed inside the internal area of cervix before entering the uterine. During cervix dilatation, pain signals are transferred via parasympathetic fibers along with uterine and cardinal ligament vessels. As a result, para-cervical block takes place within the 3rd and 9th hour (3). Nowadays, the most common drug used for local anesthesia is lidocaine. Lidocaine is economically affordable and it has less side effects compared to other local anesthesia drugs. High doses of lidocaine may result in symptoms of tremor and convulsion. In the case of sensitivity to the medicine, allergic symptoms will show up and in rare cases, we may expect Bradycardia and Hypotension (4). Taking into consideration the above said side effects of general anesthesia and to prevent losing more blood among emergency patients, para-cervical block is really helpful. Para-cervical block is one of the several methods of anesthesia carried out by gynecologists and it does not require the constant and continuous presence of anesthesiologist. As a result, it is considered to be the best method in cases of emergency. Various studies have utilized different medical combinations in para-cervical block. The most common one has been 2% lidocaine. Considering the short term analgesic effects of lidocaine in para-cervical block, we decided to enhance the intensity and length of analgesia by adding Fentanyl and Ketamine to the common local anesthesia drug (lidocaine) and have a better control over post-operative pain.
Materials and Method
This is a double blind, randomized clinical trial research conducted on 120 women aging 20 to 45 who had resorted to Taleghani Hospital of Arak for curettage. The participants were randomly divided into three groups (using the table of random numbers): lidocaine with Ketamine, lidocaine with Fentanyl, and lidocaine with distilled water. Each group was composed of 40 people. All the participants entered the research after their informed consent was gained and their inclusion criteria were checked. After a full monitoring of vital signals (ECG, BP, RP, BP, SPO2), the patients received 3-5 cc/kg crystalloid as the alternative liquid. Then while the patients were lying on their back (supine position), 2 μg Midazolam as a sedative and 2cc (equal to 10 mg) Sufentanil were injected to them. The patients were then asked to assume a lithotomy position and para-cervical block was accomplished in completely sterilized conditions. The first group was injected with 5cc of 1.5% lidocaine and 50 μg Fentanyl equal to 1cc (totally 6cc), while those in the third group were 25 mg (1cc) 1.5% lidocaine-ketamine and the third group was injected with 5cc lidocaine plus 1cc placebo within the 3rd and 9th hour after cervix. 10cc syringes containing the medicine were previously prepared by anesthesiologist and labeled by A, B, and C. The syringes were then given to executor of plan and para-cervical block was accomplished. Having made sure about the position of the above-said block, curettage operation was carried out. Every 5 minutes during the operation, the hemodynamic status of patients (including BP, PR) was registered in the questionnaire and after the operation was over, the pain score of patients was measured using VAS (visual analog score) ruler 30 and 60 minutes after operation in recovery. The average analgesia length of patients was also measured based upon their first request for painkillers and the correlating information was registered in the questionnaire. The information obtained through this questionnaire was statistically analyzed using SPSS 19 and statistical tests such as T-test and ANOVA.
Table 1: The average age of patients in three groups
| Study groups | Ketamine | Fentanyl | Placebo | P-value |
| Average age | 29.9 ± 6.2 | 28.9 ± 5.5 | 28.5 ± 5.9 | P ≥ 0.05
Nonsignificant |
Table 2: The average pregnancy length of patients in three groups
| Study groups | Ketamine | Fentanyl | Placebo | P-value |
| Average pregnancy length | 39.5 ± 1.5 | 39.2 ± 1.3 | 39.3 ± 1.7 | P ≥ 0.05
Nonsignificant |
Table 3: The average systolic pressure of patients in three groups
| Study groups | Ketamine | Fentanyl | Placebo | P-value |
| Average systolic pressure | 111.1 ± 7.5 | 109.5 ± 7.6 | 108.5 ± 9.4 | P ≥ 0.05
Nonsignificant |
Table 4: The average diastolic pressure of patients in three groups
| Study groups | Ketamine | Fentanyl | Placebo | P-value |
| Average diastolic pressure | 71.2 ± 7.5 | 70.2 ± 9.1 | 71.5 ± 8.9 | P ≥ 0.05
Nonsignificant |
Table 5: The average heart rate of patients in three groups
| Study groups | Ketamine | Fentanyl | Placebo | P-value |
| Average HR | 85.1 ± 7.5 | 85.9 ± 5.1 | 85.9 ± 5.7 | P ≥ 0.05
Nonsignificant |
Table 6: The average pain scale of patients in three groups in zero minute
| Study groups | Ketamine | Fentanyl | Placebo | P-value |
| Average VAS0 | 2.1 ± 1.8 | 2 ± 1.3 | 5.2 ± 0.8 | P ≤ 0.05
Nonsignificant |
| Average VAS30 | 1.3 ± 0.5 | 1.2 ± 0.8 | 2.1 ± 0.5 | P ≤ 0.001
significant |
| Average VAS60 | 1.01 ± 0.2 | 1.4 ± 0.8 | 1.6 ± 1.1 | P ≤ 0.01
significant |
Table 7: The average analgesia length of patients in three groups
| Study groups | Ketamine | Fentanyl | Placebo | P-value |
| Average analgesia | 5.3 ± 3.9 | 5.1 ± 4.5 | 4.9 ± 2.6 | P ≤ 0.05
significant |
Inclusion Criteria
Mothers resorting to Taleghani Hospital for curettage aging 25 to 40, class I or II ASA, no background cardiovascular or pulmonary diseases, no history of convulsion, tremor, psychological or mental disease, informed consent of patient for para-cervical block, conducting the block by only one individual, conducting the curettage by only one individual, the length of curettage should not exceed 20 minutes.
Exclusion Criteria
1- failure in the above-mentioned block and conducting GA, 2- a length of more than 20 minutes, 3- being allergic to local anesthetics, 4- IV, III < ASA, 5- history of background cardiac diseases.
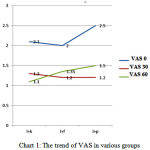 |
Figure 1: The trend of VAS in various groups |
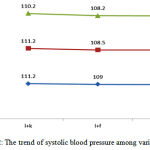 |
Figure 2: The trend of systolic blood pressure among various groups |
Results
The following results were achieved in investigating the para-cervical block in both groups concerning the average age of participants: 29.9 ± 6.2 years in ketamine plus lidocaine group, 28.9 ± 5.05 in fentanyl plus lidocaine group, and 28.5 ± 5.9 in placebo plus lidocaine group. As p-v ≥ 0.05, no significant difference was observed in the average age of treatment group (with synchronization). The following average lengths of pregnancy were reported for each group: 9.5 ± 1.5 weeks in ketamine plus lidocaine group, 9.2 ± 1.3 weeks in fentanyl plus lidocaine group, and 9.3 ± 1.7 weeks in placebo plus lidocaine group. As p-v ≥ 0.05, no significant difference is observed in treatment group concerning the average length of pregnancy. The following results were reported for the average systolic blood pressure: 111.2 ± 7.5 in lidocaine plus ketamine group, 109 ± 7.6 in fentanyl plus lidocaine group, and 108.5 ± 9.4 in placebo group. As p-v ≥ 0.05, there is no significant difference between the three therapeutic groups in terms of systolic blood pressure. As for the average diastolic blood pressure, these results were observed: 71.2 ± 7.5 in ketamine plus lidocaine group, 70.2 ± 9.1 in fentanyl plus lidocaine group, and 71.5 ± 8.9 mm Hg in placebo group. As p-v ≥ 0.05, there is no significant difference between the three therapeutic groups in terms of diastolic blood pressure. As for the average heart rate, these results were observed: 85.07 ± 5.7 in ketamine plus lidocaine group, 85.9 ± 10.5 in fentanyl plus lidocaine group, and 85.6 ± 7.5 in placebo group. As p-v ≥ 0.05, there is no statistically significant difference between the three therapeutic groups in terms of heart rate indicator. However, a significant difference was observed between the three groups in terms of heart rate: 85.6 ± 6.5 in ketamine group, 84.5 ± 2.1 in fentanyl group, and 88.3 ± 8.9 in placebo group. As P-V = 0.02, the average heart rate in fentanyl group was less than the other two groups. The following results were achieved concerning the average heart rate in the 10th minute: 86.4 ± 2.1 in ketamine group, 82.7 ± 6.1 in fentanyl group, and 88.8 ± 4.7 in placebo group. As P-V = 0.001, the average heart rate in the 10th minute in fentanyl group was less than other groups. The average levels of pain in ketamine group within 0, 30 and 60 minutes were as follows: 2.1 ± 1.8, 1.3 ± 0.5, and 1.1 ± 0.2. The average levels of pain in fentanyl plus lidocaine group within 0, 30 and 60 minutes were as follows: 2 ± 1.3, 1.2 ± 0.8, and 1.35 ± 0.3. The average levels of pain in placebo plus lidocaine group within 0, 30 and 60 minutes were as follows: 2.5 ± 0.8, 1.2 ± 0.5, and 1.5 ± 1.1. Based on the value calculated for P-V, no significant difference was observed between two groups of fentanyl and ketamine in zero minute (P ≥ 0.05). However, the average scale of pain (VAS) observed in zero minute in placebo group was more than the two other groups (P ≤ 0.05). Within 30 minutes, no significant difference is observed between the group of ketamine plus lidocaine and fentanyl plus lidocaine (P-V = 0.2). However, a higher level of pain was observed in the 30th minute in placebo group compared to other two groups (based on P ≤ 0.001). A significant difference was observed between the three groups in terms of scale of pain in 60th minute. As P ≤ 0.01, VAS in the 60th minute in Ketamine group was less than the other two groups and VAS in the 60th minute in placebo group was more than other groups. The following values were reported for the average time of requesting the primary painkiller (average analgesia time): 5.3 ± 3.9 hours in placebo group, 5.1 ± 4.5 hours in ketamine group and 4.9 ± 2.6 in fentanyl group. As P ≤ 0.05, the average length of analgesia in placebo group was less than the other two groups. However, no significant difference was observed between fentanyl and ketamine groups in terms of average analgesia length after operation (P ≥ 0.05). No post-operation nausea and vomiting was observed in ketamine group and its frequency was much less than the 2 other groups (P ≤ 0.05). No post-operative hypotension or Bradycardia was observed in any of those three groups. There was no significant difference between the three groups in terms of Bradycardia occurrence and hypotension (P ≥ 0.05).
Discussion
As the results of this research indicated, neither the fentanyl nor the ketamine had any influence upon hemodynamic parameters and arterial oxygen; however, they caused a higher level of analgesia compared to placebo. Compared to placebo, this scale of analgesia up to 60 minutes after operation showed a significant difference between fentanyl and ketamine groups and both groups exhibited higher levels of analgesia. However, no significant difference was observed between the two groups. In the 60th minute, the scale of pain in ketamine group was less than what was observed in the other 2 groups and VAS in the 60th minute in placebo group was more than other groups. The average time for requesting the primary painkiller (the average analgesia length) in placebo group was less than what was observed in the other 2 groups, but no significant difference was observed between two groups of fentanyl and ketamine in terms of the average analgesia time after operation. In other words, ketamine has a more efficient performance in post-operative analgesia compared to fentanyl, but the two medicines are similar to one another in causing the analgesia during operation and right after it. Causing damages to peripheral tissues during operation results in two changes in the response of the nervous system: 1 – Peripheral Sensitization that reduces the threshold of pain afferent terminals, 2 – Central Sensitization that increases the sensitivity of spinal neurons. When both of these changes take place together, they reduce pain threshold, sensitize the tissues and cause pain in the sight of operation and even in the areas far from the sight of operation (10). According to researches, those sensory signals dispatched from the tissues injured during operation increase the sensitivity and stimulation of central nervous system. The recent researches aim at controlling and harnessing this central sensitization. Nonsteroidal anti-inflammatory drugs, local anesthetics and opioids can be used for preemptive treatments and controlling the peripheral sensitization. An efficient treatment for analgesia and to reduce post-operative pain must focus on harnessing and controlling both central and peripheral sensitization together (10). Ketamine is an NMDA (N-methyl-D-Asparate) antagonist. It has been proposed that ketamine helps harness or reverse central sensitization and results in less post-operative pain (6). Empirical researches have pointed to the major role NMDA receptors play in injury induced spinal hypersensitivity. This sensitization of central nervous system might be one of the important causes of post-operative pains (6). Creation and development of chronic neuropathic pains can also be associated with activation of NMDA receptors. According to empirical and clinical studies, blocking NMDA receptors before or while causing injury may harness or reduce central sensitization. Blocking NMDA receptors after injury can also reduce this previously caused central sensitization (6). It has also been shown that antagonists of NMDA receptor enhance the effectiveness of other painkillers such as morphine, local anesthetics and NSAID. The mechanism of this reinforcement is probably reduction of morphine tolerance and lowering of Tachyphylaxis to local anesthetics. Seemingly, this reduced pain is caused by less central sensitization induced by ketamine (6). The results of this research are in line with the results of the research conducted by Tversicoy M. et al (1992). They studied the effects of fentanyl and ketamine on pain and the operation injury induced pain and arrived at the conclusion that fentanyl and ketamine are both effective in reducing the pain and causing analgesia compared to placebo, but they found no significant difference between them. Howver, our research pointed to the fact that ketamine was more effective than fentanyl in reducing long term analgesia. This difference may probably be attributed to the short life span of fentanyl which is a short-lived opioid (7). Mansanori Y. et al. (2008) arrived at the conclusion that adding a low dose of fentanyl helps enhance controlling analgesic pain among patients undergoing cervical spine operation. They argued that as fentanyl is a short-lived opioid, the length of its analgesia will also be short and higher doses of this medicine will be required which are not without side effects (11). The study conducted by Warwick D. et al (1997) showed that those patients who were anesthetized using ketamine for caesarian exhibited a longer period of analgesia and required less anesthetics compared to those who had taken thiopental (12). In another research carried out by Esmaoglu A. et al titled “Preemptive Application of Epidural Fentanyl in Elective Abdominal Surgeries”, it was shown that using epidural fentanyl before inflicting surgical cuts resulted in no clinically useful analgesia in patients and no difference was found between those patients and those in the control group (8). The difference between the results of this research and our results may be attributed to the methods used in each study. We used para-cervical block method in our research. Less post operation complications and side effects such as nausea, vomiting, headache, feeling dizzy and Bradycardia were observed in the group using ketamine compared to other groups. In the study carried out by Nergiz K. et al (1998), using ketamine didn’t result in less application of opioid doses to control post-operative pains (13). As mentioned above, various results have been reported concerning the effect of anesthetics such as fentanyl and ketamine in different researches. These differences may be attributed to factors such as different types of surgery, various lengths of operation, selecting different patients, and the design of research. In the current research, all the patients chosen for study were undergoing the same operation and the type of operation was never a heavy type where the abdominal organs are disposed. The operation referred to in this research was a light one where abdominal organs were not disposed. Considering the fact that patients had no background disease and the short period of operation, fentanyl and ketamine seem useful drugs to cause short term analgesia and numbness after operation. However, ketamine is more useful in long term analgesia considering the short life span of fentanyl.
References
- Mankowski , JL. et al. Paracervical compared with intracervical lidocaine for suction curettage: a randomized controlled trial. Obstetrics & Gynecology 2009; 113(5): 1052-1057.
- Poornima, C. “Intracervical block compared with intramuscular sedation for dilatation and curettage Int J Reprod Contracept Obstet Gynecol 2014; 3(1): 149-152.
- Kingston, J, Charles W. N. “Paracervical Compared With Intracervical Lidocaine for Suction Curettage: A Randomized Controlled Trial.” Obstetrics & Gynecology 2009; 114(4): 927-928.
- Ejlersen, Ellen, et al. “A comparison between preincisional and postincisional lidocaine infiltration and postoperative pain.” Anesthesia & Analgesia 1992; 74(4):495-498.
- Gourlay, Geoffrey K., et al. “Fentanyl blood concentration-analgesic response relationship in the treatment of postoperative pain.” Anesthesia & Analgesia 1988; 67(4): 329-337.
- Kwok, Rebecca FK, et al. “Preoperative ketamine improves postoperative analgesia after gynecologic laparoscopic surgery.” Anesthesia & Analgesia 2004; 98(4): 1044-1049.
- Tverskoy, Mark, et al. “Preemptive effect of fentanyl and ketamine on postoperative pain and wound hyperalgesia.” Anesthesia & Analgesia 1994; 78(2): 205-209.
- Esmaoğlu, A., Y. Cuha, and A. Boyaci. “Pre‐emptive efficacy of epidural fentanyl in elective abdominal surgery.” European journal of anaesthesiology 2001; 18(1): 59-63.
- Lauretti, Gabriela R., and Vera MS Azevedo. “Intravenous ketamine or fentanyl prolongs postoperative analgesia after intrathecal neostigmine.” Anesthesia & Analgesia 1996; 83(4):766-770.
- Eide PK, Stubhaug A, Oye I. The NMDA-antagonist ketamine forprevention and treatment of acute and chronic post-operative pain.Baillie`re’s Clin Anaesthesiol 1995; 9: 539–54.
- Masanori Y, Makoto A,Masanori W,Soushi Iw,Shingo F, Akiyosh i N,Continuous Low-Dose Ketamine Improves the Analgesic Effects of Fentanyl Patient-Controlled Analgesia AfterCervical Spine Surgery Anesth Analg 2008; 107: 1041–4.
- Warwick D at al Postoperative Analgesic Requirement After Cesarean Section: A Comparison of Anesthetic Induction with Ketamine or ThiopentalAnesthesia & Analgesia. 1997; 85(6):1294-1298.
- Kucuk, Nergiz, Mehmet Kizilkaya, and Murat Tokdemir. “Preoperative epidural ketamine does not have a postoperative opioid sparing effect.” Anesthesia & Analgesia 1998;87(1):103-106.
- J ha AK, Bhardwaj N, Yaddanapudi S, Sharma RK, Mahajan JK. A randomized study of surgical site infiltration with bupivacaine or ketamine for pain relief in children following cleft palate repairPaediatrAnaesth. 2013;23(5):401-6.
- Elia N, Tramer MR. Ketamine and postoperative pain a quantitativesystematic review of randomised trials. Pain 2005;113(1–2):61–70.







