Salman Y. Guraya1, Shaista S. Guraya2 and Hamdi H. Almaramhy3
1Department of Surgery College of Medicine Taibah University Almadinah Almunawwarah Saudi Arabia.
2Department of Radiology College of Medicine Taibah University Almadinah Almunawwarah Saudi Arabia.
3Department of Pediatric Surgery College of Medicine Taibah University Almadinah Almunawwarah Saudi Arabia.
*Corresponding Author E-mail: salmanguraya@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/1007
Abstract
Medical professionalism is a multi-dimensional construct. Teaching the culture-specific, context-based and societal characteristics of medical professional are challenging. This work identifies the teaching strategies for medical professionalism drawn from the published articles that have validated their effectiveness through some objective measures. In May 2016, the databases of ISI web of knowledge, Scopus, the Cochrane Library, and MEDLINE were searched for the full-text English-language articles published during 2005 through 2015 using the keywords “Medical professionalism” OR “Role modelling” OR “Teaching and learning” OR “Mentoring” OR “Hidden curriculum” OR “Reflective practice”. This search showed 974 articles and further shortlisting and exclusion of non-relevant material selected 48 articles for detailed analysis in this systematic review. The published work that employed various pedagogies for teaching medical professionalism showed marked heterogeneity. The most powerful and effective strategies with profound impact has been imparted by role modelling, mentoring, hidden curriculum, reflective practice, and by effective communication. Medical faculty can exert positive and exemplary role by practicing with integrity, respect for patients, and altruism. Interactive lecture, vignettes, small group teaching, simulation and videotape reviews have been shown be effective teaching tools. There is no universally agreed model that can effectively integrate the teaching of professionalism in the medical curriculum. However, the professional performance of medical faculty by role modelling in hidden curricula and by delivering key principles of reflective practice and mentoring can potentially inculcate and promote a professionally rich culture among medical students.
Keywords
Medical professionalism; Role modelling; Teaching and learning; Mentoring; Hidden curriculum; Reflective practice
Download this article as:| Copy the following to cite this article: Guraya S. Y, Guraya S. S, Hamdi H. Almaramhy. The Legacy of Teaching Medical Professionalism for Promoting Professional Practice: A Systematic Review. Biomed Pharmacol J 2016;9(2). |
| Copy the following to cite this URL: Guraya S. Y, Guraya S. S, Hamdi H. Almaramhy. The Legacy of Teaching Medical Professionalism for Promoting Professional Practice: A Systematic Review. Biomed Pharmacol J 2016;9(2). Available from: http://biomedpharmajournal.org/?p=7914 |
Introduction
Academics have not succeeded in agreeing upon a standardised or a universal definition of medical professionalism due to its culture-specific and societal characteristics. Nevertheless, a working definition of medical professionalism is essential to its convey meaning, values, and core constructs to the medical fraternity (1). DeWitt Baldwin defines professionalism as a “value-oriented ideologically based construct” (2), Hafferty considers professionalism as “abstractedness versus specificity” (3), and van Mook describes professionalism as either an ethos or as a set of attributes to be mastered (4). In addition, medical professional has been shown to be a complex construct based on behaviours (5)(6).
The qualities of altruism, honesty, accountability, duty, integrity,respect for others, autonomy, teamwork, and lifelong learning have been attributed to medical professionalism(7). To inculcate these desirable qualities of medical professionalism in students, curriculum reforms need to be implemented that can incorporate a diverse and versatile educational contentsuch as professionalism (8). However, Howeargues that “one of themost pressing requirements for contemporary medicaleducation is to develop a framework for theory andpractice of professional development which results inthe attainment of professional competencies suitablyrobust for a lifetime’s practice” (9). This high level of goal setting is compounded by findings of the research by Guraya et al. that explored the perceptions about lapses of academic integrity from a cohort of a Saudi and a UK medical school and showed that while there was some congruence, there were also substantial differences between ratings of the importance of poor professionalism(10). These findings of variations in the perceptions towards professionalism under the influence of cultural and regional characteristics have been reported by other researchers as well (11)(12).
Teaching medical professionalism is challenging and complex (13). Riley et al. have argued that, although professionalism can be nurtured and developed, learners must possess the generic quest that can motivate them to acquire the desired qualities of professionalism (14). Literature is deeply divided as to when formal teaching of professionalism should begin and when shouldprofessionalism be embedded into the existing medical curricula(15). A wealth of evidence has shown that role modelling and early clinical contact can engage the students in socialisation and thus allowing them to enter their community of practice (16). Nevertheless, there is lack of convincing data that can support the implementation of a validated teaching and learning pedagogy for medical professionalism across the world.
The current research work attempts to systematically identify the published research that provides the best evidence for teaching medical professionalism. This work also draws upon the findings by the evidence-based studies about the instructional strategies for medical professionalism with established effectiveness through validation and objective evaluation.
Study Design
Data Sources
The databases of ISI web of knowledge, Scopus, the Cochrane Library, and MEDLINE were searched for the full-text English-language articles published during 2005 through 2015. The process of selection of articles for this systematic review was structured by the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)(17).
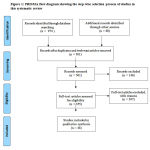 |
Figure 1: PRISMA flow diagram showing the step-wise selection process of studies in this systematic review
|
Data Selection
Medical Subject Headings (MeSH) keywords ““Medical professionalism” OR “Role modelling” OR “Teaching and learning” OR “Mentoring” OR “Hidden curriculum” OR “Reflective practice”were used for the literature search. All qualitative and quantitative reports, empirical studies and papers with clear methodology were included.
Data Extraction and Data Synthesis
The bibliographic lists from all papers fulfilling the inclusion criteria were analysed and full-text of relevant papers were retrieved. These papers were then reviewed for inclusion in the final data synthesis. To eliminate search bias and for transparency and quality, two researchers independently reviewed every single article to matching qualifying criteria during data synthesis.
Search Results
Initial search showed 974 publications and when search was refined on the bibliographic list, it showed several non-relevant articles such as abstracts, conference proceedings, letters to editor, and short communications. Articles about professionalism in professions other than medicine were also excluded.In addition, the articles about any single aspect of professionalism, like communication skills or honesty, were also excluded. Finally, 48 articles about how to teach medical professionalism were selected for this systematic review.
Lack of A Unified Model for Teaching Medical Professionalism
There is a little evidence that can support the existence of a universal theoretical or practical model that can conveniently integrate the teaching of professionalism in the medical curriculum (18). This flaw in globalization of teaching medical professionalism is mainly driven by the regional perceptions and institutional and cultural approaches towards the understanding of professionalism. Although professional institutions across the world have established criteria for professionalism, there is scarcity of literature that can signal concerted efforts mounted by a group of leading institutions that can demonstrate a validated, consolidated, and replicable teaching framework for professionalism.
Place of Medical Professionalism in Curriculum
Coulehan has rightly stated that the traditional education of professionalism is ‘too little, too soon, too late, too distant, and too countercultural’ (19). Its because professionalism is introduced too early in the medical curricula amidst other basic subjects that invariably demand rote memorization and the real essence of professionalism is overlooked. Its too distant from reality as the case scripts reviewed in classrooms often bear little resemblance to real clinical practice. Its too countercultural as the primary aims and scopes of clinical training don’t resonate well with the professional virtues. Cruess has proposed a pragmatic approach for the place of professionalism module in curriculum and has suggested that “the teaching of professionalism should start with the recognition that there is a cognitive base to professionalism which must be taught explicitly and then be reinforced and internalized by the student through experiential learning” (20).
Teaching Pedagogies for Medical Professionalism
The use of a myriad of insurrectional tools such as interactive lectures, small group discussions, case vignettes, role plays, simulations, videotape reviews, experiential learning, and dependent and independent learning play key roles in teaching professionalism (21)(22)(23). The induction of faculty development programs can be powerful tools in initiating and setting the direction for curricular reform and in promoting the faculty’s knowledge and expertiseabout medical professionalism (24)(25). Al-Eraky et al. has introduced a three-step faculty development program that has been shown to carry great promise in the Arabian context; an orientation workshop for a full-day interactive workshop; vignettes development for constructing clinical scenarios about professionalism in the relevant disciplines; and teaching professionalism where teachers presented their written vignettes to students in classrooms and clinical rounds (24).
Goldie et al. conducted tutor interviews and students focus group discussions to probe the tutors’ andstudents’ perceptions aboutthe delivery of professionalism in the early years of Glasgow’s learner-centred,integrated medicalcurriculum(16). This research developed themesabout the nature and impact of medical professionalism and effective learning strategies such as small group teaching, curriculum integration, and portfolios. The profound impact of early clinical exposure inspired the studentsand fostered their contextual and integrated learning that promote theirsocialisation into the medical profession.
The Most Commonly Applied Strands for Teaching Medical Professionalism
Research has shown a scaffold of teaching pedagogies of individual traits of medical professionalism that can be customized to the needs analysis and goal setting set by different institutions. We have identified four individual strands of professionalism and each institution can formulate a teaching framework by selecting the most suitable strands of medical professionalism(Figure 2).
 |
Figure 2: Illustration showing the contribution of role modelling, mentoring, hidden curriculum, reflective practice and various educational tools for teaching medical professionalism
|
Role Modelling
Role-modelling remains one of the most effective tools of teaching professionalism to undergraduate medical students (26).Role modelling refers to a process where “faculty members demonstrate clinical skills, model and articulate expert thought processes and manifest positive professional characteristics” (26). Role modelling has been shown to occur during forums of formal, informal and hidden curricula (27).The informal curriculum a primarily ad hoc and interpersonal type of teaching among faculty and students. Role models differ from mentors as they teach and influence by example, while mentors have a formal relationship with students.
An effective role model must possess excellent level of clinical knowledge(28), superlative teaching skills, and can create exemplary rapport with learners in a positive, supportive educational environment. The physician role models are required to inculcate a role modelling consciousness in that they should be aware of being role models when interacting with patients in the presence of learners (29). The desired personal traits of role models include effective interpersonal skills, integrity; physician leadership qualities, polite and enthusiastic, and a commitment to excellence (30). Although Basco and Reigart proposed three-stage process (observation, reflection and reinforcement) of learning from positive role models (31), role modelling can be more informal and unscheduled particularly when learners directly observe skilled doctors’ performing procedures in real workplace environment (32).Another dimension of doctors role modelling is its positive impact on career selection made by the learners as medical disciplines are so complex and current evidence identifies that the trainees’ decisions change at different stages of undergraduate and postgraduate training (33). In contrast, role modelling has been shown to disappoint the learners as doctors displayed derogatory humour and unprofessional behaviours towards their patients (34).
Mentoring
Mentoring is a relationship where mentor plays the role of an influential person whosignificantly helps the learner in achieving major life goals (35). “Mentoring is a protected relationship in which learning and experimentation can occur, potential skills can be developed, and results can be measured in terms of competencies and attainments, rather than territory covered” (36). In contrast, coaching involves a set pattern where coach teaches or trains in a particular way. The main essence of mentoring predominantly relies upon self-directed, student-centred learning through a holistic approach.
Gibbs et al. have provided ten desired core competencies that would lead to an effective mentor (36): Strong command on the subject; easy to approach and not intimidating; show genuine concerns to the mentee’s future; provide subtle judgments and don’t impose their decisions; discuss in a non-threatening environment; argue and debate in a friendly manner; compassionate; stay neutral; compassionate; and provide constructive feedback. The creation of mentor-mentee dyads holds significant potential for developing and fostering professionalism. Mentorship has a crucial role in monitoring learners’ behaviors that transcends routine assessments, as currently practiced in the majority of medical programs(37). Mentor’s role of remediation of unprofessional behavior is offered in the spirit of helping, not punishing.
The Hidden Curriculum
A hidden curriculum is known as a group of “processes, pressures and constraints which fall outside the formal curriculum, and which are often unarticulated or unexplored (38). The hidden aspects of the curriculum have been shown to be important in professional education that essentially includes prolonged periods of exposure to the predominant culture(39). Educators have pursued that hidden curriculum is the most powerful tool in transmitting the values of the profession (40)(41). As compared to what students listen in the classroom, the ever-lasting impression is created by what they witness in the daily practice of faculty members, peer, and residents. This experience ultimately strengthens their attitudes and perceptions about the real expectations of the medical profession. Its an irony that medical students witness contradictory experiences between the taught principles of professionalism and unprofessional practices (42). To witness the life-long effects of true medical professionalism, medical institutions must maintain learning environments that reflect professional aspirations and values (43).
Reflective Practice
Reflective practice, a way of studying one own’s experiences to improve the way his/her work, has also been shown to be instrumental in developing professionalism qualities, if introduced in the early in the medical education(44).It is perceived to be the preparedness of doctors to think critically and to immerse themselves in reflection upon their professional behaviours that would, in turn, promote their professional competence (45). The emerging landscape of medical professionalism emphasises the doctors to critically reflect upon their own decisions(46).Schon has argued that professionals’practice is largely based upon tacit knowledge, knowing-in-action rather than reflection-in-action, and this approach does not allow them to critically identifytheir initial understanding of the problem(47). Studies have shown that doctorswho regularly reflect upon their professional practice and learn from their experiences and errors may ultimatelyserve their community better than those who do not(44)(48). Teaching the medical students about the core principles of reflective practice has an important role in promoting the professional attributes of tomorrow’s doctors.
Communication Skills
Traditionally, effective communication skills and professionalism are known to be crucial for the practicing physicians to maintain optimum care and win patients’ confidence and trust (49). Effective communication during medical practice leads to profound benefits such as patients’ adherence to management plans, symptom resolution, and satisfaction of both patients and physicians (50). In contrast, physicians who exhibit negative communication behaviors are more likely to have been sued for malpractice than those with better doctor-patient relations (51). A study has shown that in as many as 70% of malpractice law suits, poor communication between physicians and patients accounted for most of the problems (52).
Recognising the importance of effective communication skills for physicians, academics have emphasized for a shift from biomedical to biopsychosocial and, recently, from patient-centered to relationship-centered care (53). In addition, research has shown that students’ communication skills deteriorate during their clinical years (54) and, unfortunately, the delivery of these skills is grossly overlooked during these years of studies (55). Therefore, one of the major curricular reform should aim at embedding communication skills module during the clinical years of training.
The Impact of Teaching Professionalism on Medical Students
Several quantitative studies have shown a positive impact of embedding and teaching medical professionalism to the undergraduate medical students. A study by Boenink et al. compared the professionalism of medical students before and after the introduction of professionalism programme in the Netherlands(56). The researchers reported a positive impact on students’ ability to correctly analyse and judge a scenario given as an example of professional or unprofessional behaviour. Another study by Roberts et al. showed that medical students were more satisfied by the clinical teaching of medical professionalism than the formal didactic lectures, videos, and grand rounds presentations (57). Other studies have also endorsed the effectiveness of embedding medical professionalism modules in medical curricula that can potentially improve the quality of professional practice in the long run (58)(59)(60).A growing body of qualitative research has also showna positive impact of teaching critical reflection (60), role modelling (61), and communication skills (62) to the medical students. These reports may encourage the educators for immersing medical professionalism courses in the undergraduate medical curricula. Educators can embed individual traits of medical professionalism in congruence with the societal and cultural values and institutional policies.
Conclusion
Current literature fails to reflect a clear consensus definition of professionalism. The lack of a consensus definition of professionalism hampers the development of an agreed teaching pedagogy. The educational strands for individual traits of medical professionalism that can be embedded in courses are role modelling, mentoring, hidden curriculum, reflective practice, and effective communication.However, the professional conduct of medical faculty by role modelling in hidden curricula and by teaching core principles of reflective practice and mentoring can potentially encourage and enhance a professionally rich culture among medical students. Academics are urged to collaborate worldwide to share ideas in developing excellence in role modelling and reflective that will, in turn, establish high standards of patient care and professional excellence.Future research is needed to explore the association between culture, versatility and gender while recruiting physician role models and mentors.
Authors’ contributions
SYG conceived the idea, conducted literature review and wrote the first and final draft. SSG verified the search findings and reviewed the final draft. HHA reviewed the final draft and all authors approved final manuscript.
Conflict of Interests
None declared
References
- Birden H, Glass N, Wilson I, Harrison M, Usherwood T, Nass D. Teaching professionalism in medical education: a Best Evidence Medical Education (BEME) systematic review. BEME Guide No. 25. Medical teacher. 2013;35(7):e1252-e66.
- Baldwin DC. Two faces of professionalism. 2006.
- Hafferty F. Toward the operationalization of professionalism: A commentary. 2004.
- van Mook WN, van Luijk SJ, O’Sullivan H, Wass V, Zwaveling JH, Schuwirth LW, et al. The concepts of professionalism and professional behaviour: Conflicts in both definition and learning outcomes. European Journal of Internal Medicine. 2009;20(4):e85-e9.
- Green M, Zick A, Makoul G. Defining professionalism from the perspective of patients, physicians, and nurses. Academic Medicine. 2009;84(5):566-73.
- Guraya SY, Guraya SS, Mahabbat NA, Fallatah KY, Al-Ahmadi BA, ALalawi HH. The Desired Concept Maps and Goal Setting for Assessing Professionalism in Medicine. 2016.
- Cruess SR, Cruess RL. Professionalism as a Social Construct: The Evolution of a Concept. Journal of graduate medical education. 2016;8(2):265-7.
- Gordon J. Fostering students’ personal and professional development in medicine: a new framework for PPD. Medical education. 2003;37(4):341-9.
- Howe A. Professional development in undergraduate medical curricula–the key to the door of a new culture? Medical education. 2002;36(4):353-9.
- Guraya SY, Norman RI, Roff S. Exploring the climates of undergraduate professionalism in a Saudi and a UK medical school. Medical teacher. 2016:1-3.
- Chandratilake M, McAleer S, Gibson J. Cultural similarities and differences in medical professionalism: a multi‐region study. Medical education. 2012;46(3):257-66.
- Babelli S, Chandratilake M, Roff S. Recommended sanctions for lapses in professionalism by student and faculty respondents to Dundee Polyprofessionalism Inventory I: Academic Integrity in one medical school in Saudi Arabia. Medical teacher. 2015;37(2):162-7.
- Martin J, Lloyd M, Singh S. Professional attitudes: can they be taught and assessed in medical education? Clinical Medicine. 2002;2(3):217-23.
- Riley S, Kumar N. Teaching medical professionalism. Clinical Medicine. 2012;12(1):9-11.
- Levenson R. Understanding doctors: harnessing professionalism. 2008.
- Goldie J, Dowie A, Cotton P, Morrison J. Teaching professionalism in the early years of a medical curriculum: a qualitative study. Medical education. 2007;41(6):610-7.
- Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic reviews. 2015;4(1):1.
- Gracey CF, Haidet P, Branch WT, Weissmann P, Kern DE, Mitchell G, et al. Precepting humanism: strategies for fostering the human dimensions of care in ambulatory settings. Academic Medicine. 2005;80(1):21-8.
- Coulehan J. Viewpoint:: Today’s Professionalism: Engaging the Mind but Not the Heart. Academic Medicine. 2005;80(10):892-8.
- Cruess SR. Professionalism and medicine’s social contract with society. Clinical orthopaedics and related research. 2006;449:170-6.
- Steinert Y, Cruess S, Cruess R, Snell L. Faculty development for teaching and evaluating professionalism: from programme design to curriculum change. Medical education. 2005;39(2):127-36.
- Guraya SY, Almaramhy HH. Small group teaching improves students’ acquisition of knowledge and skills. Saudi medical journal. 2012;33(12):1304-9.
- Guraya S, Alzobydi A, Salman S. Objective structured clinical examination: Examiners’ bias and recommendations to improve its reliability. J Med Med Sci. 2010;1(7):269-72.
- Al-Eraky MM, Donkers J, Wajid G, Van Merrienboer JJ. Faculty development for learning and teaching of medical professionalism. Medical teacher. 2015;37(sup1):S40-S6.
- Lu W-H, Mylona E, Lane S, Wertheim WA, Baldelli P, Williams PC. Faculty development on professionalism and medical ethics: The design, development and implementation of Objective Structured Teaching Exercises (OSTEs). Medical teacher. 2014;36(10):876-82.
- Loh KY, Nalliah S. Learning professionalism by role‐modelling. Medical education. 2010;44(11):1123-.
- Ravindra P, Fitzgerald J. Defining surgical role models and their influence on career choice. World journal of surgery. 2011;35(4):704-9.
- Côté L, Leclère H. How Clinical Teachers Perceive the Doctor—Patient Relationship and Themselves as Role Models. Academic Medicine. 2000;75(11):1117-24.
- Kahn MW. Etiquette-based medicine. New England Journal of Medicine. 2008;358(19):1988-9.
- Cohen JJ. Professionalism in medical education, an American perspective: from evidence to accountability. Medical education. 2006;40(7):607-17.
- Basco Jr WT, Reigart JR. When Do Medical Students Identify Career‐influencing Physician Role Models? Academic Medicine. 2001;76(4):380-2.
- Guraya SY. Workplace-based assessment; applications and educational impact. Malaysian Journal of Medical Sciences. 2015;22(6):5-10.
- Park J, Woodrow SI, Reznick RK, Beales J, MacRae HM. Observation, reflection, and reinforcement: surgery faculty members’ and residents’ perceptions of how they learned professionalism. Academic Medicine. 2010;85(1):134-9.
- Passi V, Johnson S, Peile E, Wright S, Hafferty F, Johnson N. Doctor role modelling in medical education: BEME Guide No. 27. Medical teacher. 2013;35(9):e1422-e36.
- Pololi LH, Knight SM, Dennis K, Frankel RM. Helping medical school faculty realize their dreams: an innovative, collaborative mentoring program. Academic Medicine. 2002;77(5):377-84.
- Gibbs T, Brigden D, Hellenberg D. Mentoring in medical practice. South African Family Practice. 2005;47(8):5-6.
- Larkin GL. Mapping, modeling, and mentoring: charting a course for professionalism in graduate medical education. Cambridge Quarterly of Healthcare Ethics. 2003;12(02):167-77.
- Cribb A, Bignold S. Towards the reflexive medical school: the hidden curriculum and medical education research. Studies in Higher Education. 1999;24(2):195-209.
- Marinker M. Myth, paradox and the hidden curriculum. Medical education. 1997;31(4):293-8.
- Haidet P, Kelly PA, Chou C. Characterizing the patient-centeredness of hidden curricula in medical schools: development and validation of a new measure. Academic Medicine. 2005;80(1):44-50.
- Hafferty FW. Beyond curriculum reform: confronting medicine’s hidden curriculum. Academic Medicine. 1998;73(4):403-7.
- Cruess RL, Cruess SR. Teaching professionalism: general principles. Medical teacher. 2006;28(3):205-8.
- Karnieli-Miller O, Vu TR, Holtman MC, Clyman SG, Inui TS. Medical students’ professionalism narratives: a window on the informal and hidden curriculum. Academic Medicine. 2010;85(1):124-33.
- Mamede S, Schmidt HG. The structure of reflective practice in medicine. Medical education. 2004;38(12):1302-8.
- Maudsley G, Strivens J. Promoting professional knowledge, experiential learning and critical thinking for medical students. Medical education. 2000;34(7):535-44.
- Arnold L. Assessing professional behavior: yesterday, today, and tomorrow. Academic Medicine. 2002;77(6):502-15.
- Schon DA, DeSanctis V. The reflective practitioner: How professionals think in action. The Journal of Continuing Higher Education. 1986;34(3):29-30.
- Mamede S, Schmidt HG, Penaforte JC. Effects of reflective practice on the accuracy of medical diagnoses. Medical education. 2008;42(5):468-75.
- Symons AB, Swanson A, McGuigan D, Orrange S, Akl EA. A tool for self-assessment of communication skills and professionalism in residents. BMC medical education. 2009;9(1):1.
- Zolnierek KBH, DiMatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Medical care. 2009;47(8):826.
- Levinson W, Roter DL, Mullooly JP, Dull VT, Frankel RM. Physician-patient communication: the relationship with malpractice claims among primary care physicians and surgeons. Jama. 1997;277(7):553-9.
- Beckman HB, Markakis KM, Suchman AL, Frankel RM. The doctor-patient relationship and malpractice: lessons from plaintiff depositions. Archives of Internal Medicine. 1994;154(12):1365-70.
- Engel GL. The need for a new medical model: a challenge for biomedicine. Psychodynamic psychiatry. 2012;40(3):377.
- Haidet P, Dains JE, Paterniti DA, Hechtel L, Chang T, Tseng E, et al. Medical student attitudes toward the doctor–patient relationship. Medical education. 2002;36(6):568-74.
- Silverman J. Teaching clinical communication: A mainstream activity or just a minority sport? Patient education and counseling. 2009;76(3):361-7.
- Boenink AD, Jonge Pd, Smal K, Oderwald A, Tilburg Wv. The effects of teaching medical professionalism by means of vignettes: an exploratory study. Medical teacher. 2005;27(5):429-32.
- Roberts LW, Hammond KAG, Geppert CM, Warner TD. The positive role of professionalism and ethics training in medical education: a comparison of medical student and resident perspectives. Academic Psychiatry. 2004;28(3):170-82.
- Shapiro J. Perspective: does medical education promote professional alexithymia? A call for attending to the emotions of patients and self in medical training. Academic Medicine. 2011;86(3):326-32.
- LIE D. Point-of-view writing: a method for increasing medical students’ empathy, identification and expression of emotion, and insight. Education for Health. 2006;19(1):96-105.
- Baernstein A, Fryer-Edwards K. Promoting reflection on professionalism: a comparison trial of educational interventions for medical students. Academic Medicine. 2003;78(7):742-7.
- Lempp H, Seale C. The hidden curriculum in undergraduate medical education: qualitative study of medical students’ perceptions of teaching. BMJ. 2004;329(7469):770-3.
- Guraya SS, Habib F, Khoshhal KI, Guraya SY, Fawzi MM. Students attitude and response towards communication skills course at the College of Medicine, Taibah University. Education in Medicine Journal. 2013;5(3).







