E. Rajesh, R. Jayasri Kurupaa, M. Kasthuri* and N. Balachander
Department of Oral Pathology, Sree Balaji Dental College and Hospital, Bharath University, Pallikaranai, Chennai-600100.
DOI : https://dx.doi.org/10.13005/bpj/1027
Abstract
In oral tissues,the mast cell releases various pro-inflammatory cytokine tumor necrosis factor alpha (TNF-Ü) which stimulate leukocyte infiltration in various inflammatory condition of oral cavity such as oral lichen planus (OLP), periapical lesions, gingivitis & periodontitis. Mast cells are the local residents of the connective tissue and plays an important role in immunopathology and producing mitogenic cytokines.These cells plays a role in pathogenesis of oral diseases.
Keywords
tissues; releases; various
Download this article as:| Copy the following to cite this article: Rajesh E, Kurupaa R. J, Kasthuri M, Balachander N. Role of Mast Cell in Oral Pathology. Biomed Pharmacol J 2016;9(2). |
| Copy the following to cite this URL: Rajesh E, Kurupaa R. J, Kasthuri M, Balachander N. Role of Mast Cell in Oral Pathology. Biomed Pharmacol J 2016;9(2). Available from: http://biomedpharmajournal.org/?p=8173 |
Introduction
Mast cells are granulated cells and appears as a large spherical cells which is present in all of the connective tissue elements including skin, submucosa or connective tissue of various organs and mucosal epithelial tissues & also in dental pulp1,2. Life span of weeks to months.It is derived from bonemarrow and it contains granules granules are rich in heparin, chondroitin sulphate, proteoglycan and numerous enzymes including collagenase.These granules are metachromatic in nature and it is confirmed with staining such as Toludine blue.
Ultrastructure of Mast Cell :
Three types of mast cell :In deeper connective tissue,the cells (except that in close vicinity to blood vessels) appears as round /oval in shape & dark purple in colour. The borders of cell are well defined & nucleus is not visible due to granules called as intact cells3
In the superficial connective tissue, the mast cells appear flattened / irregular and the cytoplasm appears granular immediately below the infiltrate area and near the blood vessels . The cell borders are not defined and the nucleus is only partially appreciable; these are called spreading cells4.
The third type called degranulated cells found within the infiltrate & appeared paler the staining has reverted from metachromatic violet to light pink, the nucleus blue in color and well defined5
Role of mast cell released cytokines: –
IL-3 – induce basophil recruitment & activation
IL-5-eosinophil recruitment & activation
IL-13 – induction of IgE synthesis
Mast cell bears receptors for IgE and degranulates this cytophilic antibody is cross-linked by antigen . Mast cell RANTES degranulation can be caused by other factors such as mechanical trauma, complement C5a, eosinophil –derived cationic protein, and bacterial products . In the absence of IgE mediated activation the mast cell can produce inflammation and its events under many conditions6.
Thus, mast cell release proinflammatory mediators, promotes inflammation and angiogenesis, extracellar matrix degeneration and tissue remodeling.
Role of MC in Oral Pathologies:
Role of MC in OLP:
Mechanism
RANTES activation
↓
Mast Cells chemotaxis and degranulation
↓
TNF- Ü
↓
Endothelium cell adhesion molecule
expression (Cd62 E, CD54, CD106)
↓
Chymase activation
↓
MMP- 9 activation
↓
Disruption of basement membrane
↓
Keratinocyte apoptosis
↓
Intra epithelial CD 8
T-cell migration through BM
↓
Survival of inflammatory cell
↓
Non-specific T-cell recruitment1
Action of mast cell mediators in oral lichen planus leading to the following clinical
and histopathological changes7
Table 1
| Mediators | Clinical features | Histopathologic features |
| Histamine
. Induces vasopermeability.. . Antigen induced T-cell proliferation Inhibits the neutrophil. . Induces increased expression of E-selectin, ICAM and ICAM, which causes leukocytic margination |
. Vesicles, bullae and erosive lesions
Chronic persistence of the lesion.
|
Submucosal edema. Traffi cking of T-lymphocytes..
|
| TNF-alpha
. Increased production of matrix metalloproteinases like stromyelsin, collagenase. Destruction of basement membrane |
Vesicles, bullae and erosive lesions | Necrosis and liquifactive degeneration of basal cell layer. |
Action of mast cell mediators in oral submucous fi brosis leading to the following
clinical and histological changes7
Table 2
| Mediators | Clinical features | Histopathologic features |
| Prostaglandins and leukotreines
Increase the mucous gland secretion Increased venous permeability
|
– Excessive salivation. | Submucosal edema |
| Histamine
Causes vasodilatation and vasopermeability. |
Submucosal edema
|
|
| Heparin
. Causes vasoproliferation. – |
Petechiae
|
|
| Interleukin-5
. Causes growth and differentiation of eosinophils
|
Itching sensation
. |
In early stages of oral submucous fibrosis consists of Inflammatory infiltrate eosinophils |
| Eosinophilic chemotactic factor (ECF)
Causing eosinophilic migration |
||
| Interleukin-1
. Stimulates fibroblastic proliferation. |
Decreased mouthopening | Increased collagen fiber bundles. |
Role of MC in angiogenesis in oral squamous cell carcinoma:
Action of mast cell mediators in oral squamous cell carcinoma leading to the following clinical and histologic
al changes7
Table.3
| Mediators | Clinical features | Histopathologic features |
| IL-1 AND TNF-alpha
. Causes increased epithelial cell proliferation.. |
Exophytic growth or a plaque | Increased thickness of the epithelium |
| Heparin
. Causes angiogenesis and type-VIII |
Tumour angiogenesis | Increased vascularity of the stroma. |
Role of MC in oral leukoplakia:
Action mast cell mediators in oral leukoplakia leading to the following clinical and histological changes7
Table.4
| Mediators | Clinical features | Histopathologic features |
| Histamine
. Enhances permeability across the epithelial surface. Antigen induced T-cell proliferation. |
Chronicity of the lesion | Increased mucosal permeability despite hyperkeratosis
|
| Heparin
. Causes endothelial cell proliferation and migration |
Erosive leukoplakia. | Increased vascularity of the stroma
and ulceration. |
| Interleukin-1 and TNF
. Increased epithelial cell proliferation. |
White patch or a plaque | Increased thickness of the epithelium. |
Role of MC in Periapical lesions
Mechanism
Role of MC in Pyogenic Granuloma
MC + neuropeptides
neural immune network with LC in mucosal tissue
↓
Degranulation of MC
↓
Cytokine, vasoactive amine and enzyme
↓
Inflammatory and vascular changes
↓
Pyogenic granuloma
Role of MC in wound healing
Wound healing is a dynamic process consisting of four phases:
- Homeostasis
- Inflammation
- Proliferation
d. Tissue remodeling and resolution
MC activate fibroblast
enzyme
tryptase
↓
synthesis collagen + hyaluronic acid
↓
fibrous tissue formation
↓
MC + fibroblast13
↓
fibronectin integrin
receptor
Wound healing
Wound healing involves degradation, cell migration, synthesis of fibronectin, fibrin and high amount of collagen type II and matrix remodeling to return the tissue to normality
III. MMP – 9 from mast cell →
Wound healing1
Role of mast cell in peripheral ossifying fibroma9:
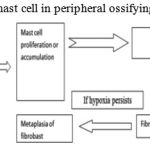 |
Figure 1
|
Conclusion
This article mainly focus that all oral reactive lesions have MCs , thus having a possible role in pathogenesis of these lesions.In recent years. Mast cells have gained a lot of importance owing to the vast number of chemical mediators released by them with wide range of actions in various disease processes. Once confirmed, it makes easier for us to target the therapeutic modalities against mast cells and the granules it contains to alter the course of disease/lesion.
Reference
- Supriya Kheur Deepali Patekar Neeta Bagul, Role of mast cell in oral pathology;ompj,vol .4,no.1 jan – june 2013
- molouk torabi parizi1, mehrnaz karimi afshar, maryam rad, an investigation on mast cells count in oral reactive lesions, int.j.curr.res.aca.rev,2015;3(8):1-6
- Mahija Janardhanan,V.Ramesh. Mast Cells in Oral Lichen Planus. OMPJ(2010); Vol 1 No 2
- I.G.Rojas, A.Martinez, A.Pineda, et al.Increased mast cell density and protease content in actinic cheilitis.J Oral Pathol Med(2004);33:567-7
- Lawrence J. Walsh. Mast Cells and Oral Inflammation.Crit Rev Oral Biol Med(2003); 14(3);188-98.
- Radojica Drazic, Jelena Sopta, Arsa J et al. Minic. Mast cells in periapical lesions: potential role in their pathogenesis. J Oral Pathol Med (2010) 39:257-262.
- Madhuri Ankle R, Alka Kale D, Ramakant Nayak; Mast cells are increased in leukoplakia, oral submucous fi brosis, oral lichen planus and oral squamous cellcarcinoma. Journal of Oral and Maxillo Facial Pathology Vol. 11 Issue 1 Jan – Jun 2007
- S. Guo and L.A.DiPietro. Factors affecting wound healing. JDent Res (2010);89(3):219- 229
- Humaira Nazir, Dr. Imran NazirSalroo,Dr.Jyothi Mahadesh,Quantitative Assessment of Mast Cells in Oral Reactive Lesions,IOSR Journal of Dental and Medical Sciences, Jun. 2015,Volume 14, Issue 6 Ver. III








