Mathew Asok1, Prabhu Manickam Natarajan2, Sheikha Saeed3, Majd Khalid4, Nisha Varughese5, Ahmed Al- Radaideh6 and Menon P. K7
1Research scholar,Phdin dental sciences, Pacific university, Udaipur, India.
2Assistant professor, college of dentistry, Gulf medical university, Ajman.
3Internship trainee, Ministry of health.
4Internship trainee, Ajman University of science and technology, Ajman.
5Resident, Hamdan bin Mohammed College of dental medicine, Dubai.
6Faculty, college of general studies, Ajman University of science and technology, Al Fujairah.
7Director, CABRI Labs, Ajman, UAE.
*Corresponding Author E- mail: drashokm@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/990
Abstract
It is found that salivary cortisol values follow the same pattern as the serum cortisol. They are found to have high correlation with some parameters showing disturbances in HPA –axis. Cortisol levels rise due to circadian influences as well as perturbations in the organism’s environment (i.e., stressors) that make it possible to detect. The following study was done to study the effect of HPA axis in the salivary cortisol and daily variation. It was also done to study the circadian rhythm of the hormone in patients with periodontal diseases and the correlation of salivary cortisol with loss of attachment in periodontium, Hamilton’s anxiety scale, BMI, sleeping pattern, waist circumference, PBI( periodontal bleeding index), SOHI(simplified oral hygiene index), etc. The study was planned for patients with chronic adult periodontitis and control subjects. All participants, aged 20-50 years, were examined at the clinics of Ajman University (Al-Fujairah). They were informed to provide three samples that were stored at 3-5 degrees Celsius and submitted next day. Samples were frozen (– 20°c) and analyzed in COBAS e 411 by ECLIA (Electro-chemiluminescence) method. The highest mean value of salivary cortisol was 30 minutes after waking up for both groups, but was higher in the control group. BMI, S-OHI and HAM-A had some correlation in both groups. No correlations found with periodontal loss of attachment and pocket depth. Cortisol gap showed a more positive trend in the periodontitis group compared with control group. The circadian rhythm is established in salivary samples and follows the same pattern in serum. Cortisol gap can be used instead of cortisol awakening response as a diagnostic value in defining periodontal diseases and its severity.
Keywords
Cortisol; Periodontitis; HPA axis; Electro chemilumin escence
Download this article as:| Copy the following to cite this article: Asok M, Natarajan P. M, Saeed S, Khalid M, Varughese N, Al-Radaideh A, Menon P. K. A Study on Comparison of Salivary Cortisol Circadian Rhythm in Periodontal Diseases with External Stressors and Clinical Parameters. Biomed Pharmacol J 2016;9(2). |
| Copy the following to cite this URL: Asok M, Natarajan P. M, Saeed S, Khalid M, Varughese N, Al-Radaideh A, Menon P. K. A Study on Comparison of Salivary Cortisol Circadian Rhythm in Periodontal Diseases with External Stressors and Clinical Parameters. Biomed Pharmacol J 2016;9(2). Available from: http://biomedpharmajournal.org/?p=7684 |
Introduction
There are three endocrine glands that have influences and feedback interactions to each other which are hypothalamus, pituitary and the adrenal glands that’s form a complex known as hypothalamic–pituitary–adrenal axis. It’s the main session of neuroendocrine system which responsible for regulation of stress and control the body metabolisms such as emotion, immune system, digestion, sexuality and energy preservation (10).
It is the major process for interactions of glands and hormones. Also, the midbrain has it as a part that mediates the general adaptation syndrome. Because of the physiological response of the HPA axis and corticosteroids in stress it lies in the vertebrates and monocellular organism (10).
It connects superiorly with the hypothalamus via infundibulum which is funnel shape. It divides into two parts or lobes one of them glandular and the other is neural tissue. The anterior part is the glandular which has the responsibility of manufacturing and releasing hormones. The posterior part and infundibulum form a complex known as neurohypophysis, this complex has the duty to store the hormones. Hypophyseal branches of the internal carotid arteries supplies the blood to the pituitary gland while the drainage via veins into the dural sinuses (4).
Posterior pituitary and the hypothalamus are related by the formation of oxytocin and ADH by the hypothalamic neurons. These hormones are transported via hypothalamic-hypophyseal tract to the posterior lobe of pituitary gland. Anterior pituitary and the hypothalamus relationship have three steps. At the beginning hypothalamic neuron stimulated, it secretes releasing and inhibiting hormones into the primary capillary plexus (4). Adrenal glands are pyramid-shaped and lie above the kidney. They consist of two components which are adrenal medulla and adrenal cortex. Each of them releases a specific type of hormones(4).
Essentials for the Function of the HPA Axis
The inhibition of the hypothalamus and the pituitary glands by the negatively feedback from the cortisol that produced in the adrenal cortex. Those results in reduction of CRH and vasopressin, also minimize the cleavage of proopio-melanocortin into ACTH and β-endorphins (1). Sympathateic stimulation and the local effect of cortisol and induce the secretion of epinephrine and norepinephrine which both lead to positively feedback to the pituitary gland that increases the breakdown of POMCs into ACTH and β-endorphins(10).
The Pathophysiology of HPA Axis
Stress, illness, physical activity, blood level of cortisol and sleep\wake cycle which known also as circadian rhythm are the main factors that result in releasing of CRH(corticotrophin releasing hormone). In normal people after wakening, the cortisol level rapidly increases. After 30-45 minutes it reaches the peak, while through the day it decreases, and increases again at afternoon period. After that it decreases in late evening. If there is abnormality like insomnia, burnout or chronic fatigue the circadian cortisol cycle will be flattened (2).
The HPA axis regulates physical and psychosocial effects that leads to the adaptation of its environment and maintain the situations. It plays a main role in regulation hemostatic systems such as metabolic system, immune, reproductive, central nervous system and cardiovascular system (2 ).
Because of the stress the releasing of cortisol will be more which leads to increase the glucose that mediate fighting. This procedure decreases the highly demanding metabolic processes of immune system (2).
Cortisol is a lipophilic steroid with low molecular weight. It is synthesized and released into the blood stream, following ACTH binding to membrane receptors on cells of the adrenal cortex. Up to 95% of the secreted cortisol will be bound to large proteins (CBG, albumin) and carried throughout the body in the blood. The vast majority of cortisol actions rely on binding to its cytosolic mineralocorticoid and glucocorticoid receptors, so only the small fraction of unbound, i.e., free cortisol is thought to be biologically active. Unbound cortisol enters cells by passive diffusion, Due to its low molecular weight and lipophilic nature, which makes it feasible to measure the free cortisol fraction in all bodily fluids. While the assessment of cortisol in sweat or tears is only of theoretical importance and urinary cortisol of decreasing interest, salivary cortisol has become an invaluable tool for both clinicians and basic scientists. A number of significant advantages over the assessment of cortisol in blood have resulted in a steadily increasing interest in salivary cortisol (3)
 |
Figure 1: Cortisol chemical formula
|
The concentration of cortisol in saliva accurately reflect the level in blood when compared to the amount of unbound cortisol in serum or plasma samples however, the correlation between the total cortisol levels in blood and salivary cortisol is usually weaker due to different amounts of CBG found in blood (3).The salivary cortisol levels don’t depend on saliva flow rate relying on studies looking at salivary cortisol levels obtained under minimal and maximal flow rate. The level of salivary cortisol is influenced by drugs such as prednisone, dexamethasone and other steroids administered orally or IV While prednisone usually cross reacts with the antiserum used for assaying cortisol (leading to false high values), dexamethasone will significantly suppress the HPA axis (resulting in low cortisol levels) (3).
Periodontal disease may aggravate with stress and depression. The individuals who has stress with have less ability for brushing their teeth & there will be association of attachment loss >5mm.Addressing psychological factors, such as depression, may be an important part of periodontal preventive maintenance (6).
Materials and Methods
After getting the ethical approval from Ajman University of science and technology shown in , we started collecting samples. All the patients were given the questionnaires to assess their anxiety level and clinical examination form is filled along with the collecting vials in the initial visit. Donors may collect whole saliva by tilting the head forward, allowing the saliva to pool on the floor of the mouth, and then passing the saliva through the Saliva Collection Aid into a polypropylene vial supplied by the CABRI labs UAE. The subjects were given instruction not to eat or drink for 1 hour before the sample collection is planned. The amount of saliva collected was 2 ml. All the subjects were motivated to participate in the study by signing the patient participation form. The saliva was collected in 3 timings on the same day to find out the pattern of circadian rhythm, the first one immediately after waking up (Sample a ), second one 30 minutes after the first one( Sample b) and the third one 1 hour before sleeping( sample c). The collected samples were stored in home refrigerator at 3-5 degrees and handed over to the Ajman University next day morning. The Samples were transported to biotechnology lab to be frozen under-16 degree Celsius. The patients were divided in to 2 groups. Group A (control group) without any gingivitis or periodontal disease and group B with clinically and radio graphically established cases of chronic adult periodontitis. Sample size selected is 12 subjects in each group with 3 different readings for each patient and will collect 36 samples in each group to be tested. 2 subjects were rejected from the periodontitis group B and 1 from the control group A due to insufficient scanty saliva sample. The salivary cortisol will be evaluated with electro-chemiluminescence immunoassay method (ECLIA) using Cobas e- 411 autoanalyser by ROCHE USA.
Exclusion criteria
Patients with any systemic disease other than the ones investigated for.
Patients who are pregnant/likely to be pregnant.
Patients who are having any adverse habits (Tobacco (smoking- chewing), Bruxism, Alcohol) which can affect the said study.
Patients who are taking any sort of corticosteroids in any formulations.
Inclusion criteria
All the patients will be examined from university student clinics in the age range of 25-50 yrs.
Group 0
Control group – healthy individuals without any habits and systemic diseases.
Group A
Patients who are diagnosed with chronic adult periodontitis.
 |
Figure 2: Collecting the samples at 3 different times. |
 |
Figure 3: Centrifuge the salivary samples. |
 |
Figure 4: Arrangement of salivary samples for incubation |
 |
Figure 5: Incubation of samples under 16 centigrade |
 |
Figure 6: Cobas e- 411 autoanalyser by ROCHE USA. |
 |
Figure 7: Running the samples in the machine. |
 |
Figure 8: CORT reagent. |
Results
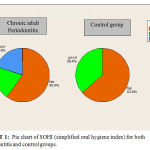 |
Chart 1: Pie chart of SOHI (simplified oral hygiene index) for both periodontitis and control groups. |
In chart 1 The percentage of patients are represented in three categories(fair, Good and Poor),but in the control group the highest percentage was for the fair group while the lowest percentage was for the good, while in the chronic adult Periodontitis group there was an equal percent for the Poor and the good category while the fair category took 60% from the group.
 |
Chart 2 |
Chart2 shows that there is correlation between the time and the salivary cortisol level during the day for both control and periodontitis groups. At the morning, after 30 minutes of waking up it shows that there is increasing in the salivary cortisol level comparing of salivary cortisol level immediately after waking up, and it decreases at evening.
Table 1: Mean and standard deviation of both groups.
| group | N | Mean | Std. Deviation | |
| a | Perio. | 10 | 17.6190 | 9.26061 |
| control | 11 | 21.2582 | 11.42968 | |
| b | Perio. | 10 | 25.4710 | 11.24774 |
| control | 11 | 31.2727 | 17.08145 | |
| c | Perio. | 10 | 8.5180 | 4.13991 |
| control | 11 | 20.3836 | 16.98513 |
*a= salivary cortisol level immediately after waking up
* b= salivary cortisol level after 30min of waking up
*c= salivary cortisol level before 1hr of sleeping
Comparing the salivary cortisol level of the control patients immediately after waking up to the patients with periodontitis, the difference between both Mean is equal to (3.64). After 30 minutes of waking up, the difference between both Mean of salivary cortisol level in the control and the periodontitis groups is (5.8) and it is (11) at 1 hour before sleeping. We notice that in control patients the mean of salivary cortisol level is higher in all timing comparing to the periodontitis patients group.
Table 2: T-test paired samples for the periodontitis group.
| N | Correlation | Sig. | ||
| Pair 1 | BMI & a | 10 | .731 | .016* |
| Pair 2 | BMI & b | 10 | .730 | .017* |
| Pair 3 | BMI & c | 10 | .230 | .523 |
| Pair 4 | PBI & a | 10 | .157 | .665 |
| Pair 5 | PBI & b | 10 | -.048 | .895 |
| Pair 6 | PBI & c | 10 | .190 | .599 |
| Pair 7 | Waist circumference & a | 10 | .414 | .235 |
| Pair 8 | Waist circumference & b | 10 | .584 | .076 |
| Pair 9 | Waist circumference & c | 10 | .563 | .090 |
| Pair 10 | Highest value of periodontal pocket in mm & a | 9 | -.332 | .382 |
| Pair 11 | Highest value of periodontal pocket in mm & b | 9 | -.247 | .521 |
| Pair 12 | Highest value of periodontal pocket in mm & c | 9 | -.330 | .386 |
| Pair 13 | Highest value of loss of attachment in mm & a | 10 | .213 | .554 |
| Pair 14 | Highest value of loss of attachment in mm & b | 10 | .241 | .503 |
| Pair 15 | Highest value of loss of attachment in mm & c | 10 | -.030 | .935 |
*a= salivary cortisol level immediately after waking up.
* b= salivary cortisol level after 30min of waking up.
*c= salivary cortisol level before 1hr of sleeping.
There are significant values between BMI and a (soon after waking up) – BMI and b (30 mts after waking up), but there is no significant correlation with any of the other parameters.
Table 2: T- test paired samples for the control group.
| N | Correlation | Sig. | ||
| Pair 1 | BMI & a | 11 | -.182 | .592 |
| Pair 2 | BMI & b | 11 | -.409 | .212 |
| Pair 3 | BMI & c | 11 | -.166 | .626 |
| Pair 4 | PBI & a | 11 | -.503 | .115 |
| Pair 5 | PBI & b | 11 | -.533 | .092 |
| Pair 6 | PBI & c | 11 | -.234 | .489 |
| Pair 7 | Waist circumference & a | 11 | -.113 | .742 |
| Pair 8 | Waist circumference & b | 11 | -.451 | .163 |
| Pair 9 | Waist circumference & c | 11 | -.255 | .448 |
*a= salivary cortisol level immediately after waking up.
* b= salivary cortisol level after 30min of waking up.
*c= salivary cortisol level before 1hr of sleeping.
There are no significant values between parameters and salivary cortisol level.
Table 4: Correlations between the parameters and the salivary cortisol level in control patients
| HAMA-A | Waist
Circum. |
Sleeping
pattern |
PBI | SOHI | BMI |
| a | Pearson Correlation | .794** | -.113 | .569 | -.503 | -.227 | -.182 |
| Sig. (2-tailed) | .004 | .742 | .068 | .115 | .503 | .592 | |
| N | 11 | 11 | 11 | 11 | 11 | 11 | |
| b | Pearson Correlation | .484 | -.451 | .614* | -.533 | -.618* | -.409 |
| Sig. (2-tailed) | .131 | .163 | .045 | .092 | .043 | .212 | |
| N | 11 | 11 | 11 | 11 | 11 | 11 | |
| c | Pearson Correlation | .666* | -.255 | .285 | -.234 | -.203 | -.166 |
| Sig. (2-tailed) | .025 | .448 | .396 | .489 | .548 | .626 | |
| N | 11 | 11 | 11 | 11 | 11 | 11 |
*a= salivary cortisol level immediately after waking up.
* b= salivary cortisol level after 30min of waking up.
*c= salivary cortisol level before 1hr of sleeping.
From the table, we found out that there is no correlation between any of the parameters in control patients with the salivary cortisol level immediately after waking up (a). Moreover; The salivary cortisol level after 30min of waking up (b) has correlation with the sleeping pattern and the oral hygiene index of the control group. Furthermore; there is correlation between the anxiety scale of the control group with the salivary cortisol level (c) at 1 hour before sleeping.
Table 5: Correlations between the parameters and the salivary cortisol level in chronic adult periodontitis patients
| HAMA-A | Waist
Circum. |
Sleeping
pattern |
Highest v. of attachment loss | PBI | SOHI | BMI |
| A | Pearson Correlation | .642* | .414 | .131 | .213 | .157 | .667* | .731* |
| Sig. (2-tailed) | .046 | .235 | .718 | .554 | .665 | .035 | .016 | |
| N | 10 | 10 | 10 | 10 | 10 | 10 | 10 | |
| B | Pearson Correlation | .416 | .584 | -.121 | .241 | -.048 | .922** | .730* |
| Sig. (2-tailed) | .231 | .076 | .739 | .503 | .895 | .000 | .017 | |
| N | 10 | 10 | 10 | 10 | 10 | 10 | 10 | |
| C | Pearson Correlation | .488 | .563 | .178 | -.030 | .190 | .537 | .230 |
| Sig. (2-tailed) | .153 | .090 | .623 | .935 | .599 | .109 | .523 | |
| N | 10 | 10 | 10 | 10 | 10 | 10 | 10 |
*a= salivary cortisol level immediately after waking up.
*b= salivary cortisol level after 30min of waking up.
*c= salivary cortisol level before 1hr of sleeping.
From the table, we found out that there is correlation between the anxiety scale, oral hygiene index and body mass index of the periodontitis patients with the salivary cortisol level immediately after waking up (a). Also, the salivary cortisol level after 30min of waking up(b) has correlation with the body mass index of the periodontitis group. But, there is no correlation of any of the parameters with the salivary cortisol level at 1 hour before sleeping (c).
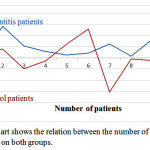 |
Chart 3: Chart shows the relation between the number of patients and the cortisol gap on both groups. |
The difference between the salivary cortisol level at early morning (immediately after waking u and without eating or drinking) and the salivary cortisol level at evening 1 hour before sleeping (and without eating or drinking before 30min) showed that it is higher in periodontitis patients comparing to control patients.Moreover;the values are more dispersed in control compared to periodontitis group.
Discussion
This study has showed clearly a circadian rhythm in the samples in both of the groups. All patients have been informed to obtain three samples (to spit without eating and drinking anything), first one immediately after waking up, the second one, 30 minutes after waking up, and the last one in the evening one hour before sleeping. It shows that a circadian rhythm with cortisol awakening response was observed, with the second sample cortisol levels noticeably greater than the others (peak value) followed by a plateau in the evening.
Our study showed that there are statistically significant association between the body mass index (BMI) and the salivary cortisol level immediately after waking up and the salivary cortisol level after 30 min of waking up yet not at 1 hour before sleeping or any of the other parameters in periodontitis patients.
C.G. Tornhage and G.Alfven (2006), did a study says that the increasing of the morning salivary cortisol level and total cortisol concentration negatively correlated with the body mass index (4). Laura ManenschijnRulanda G. P. M. Van kruysbergen(2004), conducted a study that showed results comparative to our results by proving that salivary cortisol level elevation has relation with BMI(9). In another study by S wallerius, R. Rosmond (2014), showed that rise in the morning salivary cortisol is associated with abdominal obesity (10). In our study it showed that there is no correlation between sleep pattern & salivary cortisol level. On the other hand, Juttabackhaus(2004), proved that there was decrease on the morning cortisol because of sleeping disturbances (7)
In control group, we noticed that there is a strong correlation between the salivary cortisol level and the oral hygiene index 30 minutes after waking up, but in periodontitis group there is a correlation between salivary cortisol level and the oral hygiene index immediately after waking up.J. B. Hilgert(2006), conducted a study that had (p<0.003) with patient who has high amount of plaque deposition. He also found that women with stress will have more plaque accumulation & increased levels of IL-6 and cortisol in gingival curricular fluid than the normal control (6).
In control patients, HAMA-A( Hamilton’s anxiety scale) has correlation with the salivary cortisol level 1 hour before sleeping, while in the periodontitis group we noticed that there is correlation between HAMA-A and the salivary cortisol level immediately after waking up.
Kavvedhara (2003), did a study shows that there was non-linear relation between cortisol level and the time of the day, but the extend of non-linearity was dependent upon levels of stress and anxiety(8).Van Eck (1996), did a study that focused on stress and anxiety that leads on increasing of the cortisol secretion depending on whether the event was still ongoing and on the frequency(12). Arashazizi (2013) studied the mean of the hospital anxiety and depression scale(HAD scale) with salivary cortisol level and was found to be 14.07 ± 6.10 in periodontitis group and 11.27 ± 4.24 in control group, and there is positive correlation between the anxiety scale and periodontitis (1).
The difference between the salivary cortisol level on the early morning and the salivary cortisol level at evening 1 hour before sleeping is termed as cortisol gap. This is new parameter investigated for as it showed some significance. It showed that it is higher in periodontitis patients comparing to control patients. But in another study done by Arash azizi1 (2013), showed that the salivary cortisol mean is higher on periodontitis (56.7%) than the control (13.3%) (1).
In our study, we noticed that there is no correlation between the loss of attachment, the periodontal pocket depth and the salivary cortisol level. However in a study conducted by J. B. Hilgert(2006), it was noticed that there is positive correlation between the cortisol level and the loss of attachment level (> = 4 mm) and with periodontal probing depth > = 4 mm(6).
In future studies as investigators, we canrecommend using cortisol gap as a parameter to study the effects along with cortisol awakening response as it shows a more reliable response compared to the day light variation of cortisol release. The advantage being this cortisol gap ( the difference in the values between morning level of cortisol soon after waking up and the one hour before sleep is less influenced by the chemicals from the pineal gland and external stressors.
Conclusions
In periodontitis patients, there is statistical significance observed between the body mass index (BMI) and the salivary cortisol level immediately after waking up and 30 min after waking up.It was also observed that there are no statistical differences found between any of other parameters in periodontitis patients.There is a strong correlation between BMI, SOHI and HAMA-A with the salivary cortisol level immediately after waking up (cortisol a).There is a correlation between BMI and salivary cortisol level on 30 minutes after waking up ( cortisol b).
But in control patients,there are no statistical significances existing between any of the parameters with the salivary cortisol level.There is a strong correlation between sleeping pattern and salivary cortisol level 30 minutes after waking up. It has shown that there is a correlation between patients’ oral hygiene index (S- OHI) and salivary cortisol level 30 minutes after waking up. HAMA-A / anxiety level index has a strong correlation existing with the salivary cortisol level 1 hour ( sample c )before sleeping.
References
- Arashazizi, Fatemehsarlati., 2013.Salivary cortisol levels and moderate to severe periodontitis, Research Dental Science 11(1) pp. 32-37.
- Tsigos, G.P. Chrousos., 2002. Hypothalamic–pituitary–adrenal axis, neuroendocrine factors and stress, Journal of Psychosomatic Research 53 (25) pp. 865– 871
- Clemens Kirschbaum, Dirk H. Hellhammer., 2000. Salivary Cortisol, Encyclopedia of stress, 3(7) pp. 379-383
- G. Tornhage and G.Alfven.,2006. Diurnal Salivary Cortisol Concentration in School-aged Children, Journal of Pediatric Endocrinology and Metabolism 19 (6), pp. 843–854.
- Elaine N. KatjaHoehn., 2010. Human Anatomy and Physiology, eighth edition, Benjamin Cummings.
- B. Hilgert, F.N. Hugo, D.R. Bandeira, M.C. Bozzetti., 2006. Stress, Cortisol, and Periodontitis,Journal of periodontology 85(4) pp. 324-328
- Jutta Backhaus, Klaus Junghanns., 2004. Sleep disturbances are correlated with decreased morning awakening salivary cortisol, Inernationalsocity of Psychoneuroendocrinology 29(9) pp. 1184–1191.
- KavVedharaa, Jeremy Milesc, Paul Bennettd Sue Plummer., 2003. An investigation into the relationship between salivary cortisol, stress, anxiety and depression, Biological Psychology62(2) pp. 89–96.
- Laura Manenschijn, Rulanda G. P. M. van Kruysbergen., 2011. Shift Work at Young Age Is Associated with Elevated Long-Term Cortisol Levels and Body Mass Index, Journal of Pediatric Endocrinology and Metabolism 96(11) pp.2-5.
- Wallerius, R. Rosmond, T. Ljung, G. Holm., 2003. Rise in morning saliva cortisol is associated with abdominal obesity in men, Journal of endocrinological investigation 26(7) pp. 616-619.
- Sandra Marcia. Cristiane Von Werne. Camila Maria. Mario Juruena., 2011. Early life stress, HPA axis, and depression, Psychology & Neuroscience 4 (2) pp. 229-234.
- Van Eck, Marleen, Hans.,1996. The Effects of Perceived Stress, Traits, Mood States, and Stressful Daily Events on Salivary Cortisol, Psychosomatic Medicine 58(5) pp. 447-458.







