Asadolah Amanolahi1 and Reza Salman Roghani2
1Assistant professor of Physical Medicine and Rehabilitation, Baqiyatallah Medical University, Tehran, Iran 2Associate Professor of Physical Medicine and Rehabilitation, University of Social Rehabilitation. Corresponding Author Email : amanelahi@yahoo.com
DOI : https://dx.doi.org/10.13005/bpj/915
Abstract
The current paper studies the frequency of cervical radiculopathy in patients suffering from lateral Epicondylitis resistant to treatment visiting physical clinic of Baghi’at- Allah hospital (2012- 2013). In fact, lateral Epicondylitis is known as a disease common in elbow, and as an inflammation with degenerative changes of extensor muscles. In this regard, we in this research investigate about all patients visiting physical clinic due to lateral Epicondylitis .the population of this research includes 120 patients suffering from lateral Epicondylitis resistant to treatment who visited physical clinic of Baghi’at-Allah hospital in the year 2012-2013 .it uses SPSS software for data analysis. The results obtained by data analysis indicate that there is not a meaningful relation between radiculopathy and gender of patients suffering from lateral Epicondylitis.
Keywords
lateral Epicondylitis; cervical radiculopathy; elbow lateral Epicondylitis
Download this article as:| Copy the following to cite this article: Amanolahi A, Roghani R. S. Determining Frequency of Cervical Radiculopathy in Patients Suffering from Lateral Epicondylitis Resistant to Treatment Visiting Physical Clinic of Baghi’at-Allah Hospital (2012- 2013). Biomed Pharmacol J 2016;9(1) |
| Copy the following to cite this URL: Amanolahi A, Roghani R. S. Determining Frequency of Cervical Radiculopathy in Patients Suffering from Lateral Epicondylitis Resistant to Treatment Visiting Physical Clinic of Baghi’at-Allah Hospital (2012- 2013). Biomed Pharmacol J 2016;9(1).Available from: http://biomedpharmajournal.org/?p=6884 |
Introduction
Lateral Epicondylitis is disease common for elbow; it is conjunction of extensor muscle tendons. This illness is more common in people up to 35 years old, and its peak of prevalence age is 40-50 years (Gary, 2013).the changes in degenerative of this disease typically are generated in origin of extensor muscle joint between fingers( Randall, 2011).C5-C6 roots of radicular pain are propagated to trapezius muscle, front chest, deltoid, and supracondylar. Radicular pain with C6-C7 propagates to lateral Epicondylitis and posterior forearm; radicular pains with C5, C6, and C7 roots can cause pain and symptoms similar to elbow lateral Epicondylitis. Lateral Epicondylitis is considered as resistant to treatment if it would not respond to cure within 4-6 weeks (Aaron, 2010).
Since the cause of lateral Epicondylitis might be resistance to cervical radiculopathy treat and the patient might be under several medical treatments and even elbow surgery due to inappropriate cognition of pain, thus it seems necessary to do a study in order to determine frequency of cervical radiculopathy in cases resistant to lateral Epicondylitis treat; it is emphasized on attention to cervical radiculopathy in cases resistant to lateral Epicondylitis preventing non-necessary costs, treatments, and also surgeries on patient and society.
Theoretical principles
Elbow lateral Epicondylitis Anatomy
Arm extensor muscles are divided into two surface and depth groups; all muscles of surface group are originated from humorous skeleton lateral Epicondylitis or its surroundings. But most muscles of depth group are originated from a membrane except lateral Epicondylitis.
Surface extensor muscles include:
- Brachioradialis
- ECRL
- ERCRB
- Extensor Digitorum
- Extensor Digihi Minimi
- Extensor Carpiulnaris
All surface extensor muscles of arm are innervated by radial neuron (David, 2009).
 |
Figure 1: lateral Epicondylitis anatomy |
Etiology
Lateral Epicondylitis is an inflammation along with degenerative changes originated from extensor muscles. Typically, the initial trauma ion place of extensor muscle is Carpi Brachioradialis; the other muscle dealing with the disease is ‘joint extensor of fingers’ that might lead to inflammation in 30% of cases (Randall, 2011). The initial inflammation includes: Tendinosis, Periostitis Vantezite, general injuries of muscles, and the symptoms caused by relief process.
Repeated stress imposed on elbow lateral Epicondylitis is among factors creating this disease. Vast and improper use of tennis rocket is also another symptom of disease (Walter, 2009). As said before, this disease is more common in people up to 35 years and its peak of prevalence age is 40-50 years. This disease is more common in men tennis players than women, but its prevalence is the same for men and women in public (Randall, 2011).
Epicondylitis symptoms
The pain of elbow lateral Epicondylitis might spread to proximal or more distal parts; the symptoms of diseases include pain of twist or arm when holding door catch, carrying the luggage, shaking the hands, or inflation (Walter, 2009).
 |
Figure 2: place of pain in lateral Epicondylitis |
Alike other diseases, medical history and medical visit is one of the most important ways to diagnose disease. Local tenderness on lateral Epicondylitis and positive cozen test are among findings of this disease (figure 3). Simple radiography with full face and profile is typical, but fond scheme might show point calcification in extensor muscles offspring (Randall, 2011).
 |
Figure 3: Cozen test |
Skeletal muscular medical ultrasound can be helpful for diagnosis of most diseases; it is applicable for patients with MRI prohibition since it does not use ionization ray. Ideal transducer has the frequency of 7.5-12 MHZ for skeletal muscular medical ultrasound. Medical ultrasound can dynamically show muscles, tendons, ligaments, and surface tissues. Using medical ultrasound, we can distinguish solid bulks from cystic ones and it is possible to recognize vessel bulks using color Doppler. Also medical ultrasound can be used to diagnose external substances such as wood, plastic, and glass that are not observable by cliché of radiography. Medical ultrasound is used for medical interventions such as joint injections in which direct observation of hypo would prevent injection inside tendon of muscles. One of the most common causes of artifact in anisotropy medical ultrasound is existence of tendons’ parallel fibers, and the best image would achieve when medical ultrasound prop is used with a 90 degrees angle toward tendon. Acoustic shadow is one of the fake positive results for rupture of muscles’ tendon (Randall, 2011).
Medical ultrasound is a diagnostic imagery method to study elbow lateral Epicondylitis. Medical ultrasound sensitivity for this disease is 80%, and its specific rate is 50%. Some symptoms such as osteomyelitis, tendon rupture, calcification, and skeletal bony irregularity might be observed by medical ultrasound (Richard, 2010).
 |
Figure 4: lateral Epicondylitis medical ultrasound scheme |
 |
Figure 5: calcification medical ultrasound scheme of lateral Epicondylitis |
Lateral Epicondylitis Treatment
Initial treatment includes relative rest, avoiding repeated twist motions and avoiding moves that cause stress on lateral Epicondylitis. Using twist band that links distal to origin of extensor muscles can be helpful to decrease symptoms. Impact mechanism of this band is probably force distribution in a more extensive surface of arm’s soft tissue instead of focusing on origin of extensor muscles. Also, it is effective to use twist fix bands to decrease pain. This splint can be prescribed in neutral position or 30-40 degrees of twist extension causing decrease of tension on extensor muscles. Of course, the brace extension is also used for decease treatment (Walter, 2009). The enforcement eccentric exercises of twist extensor muscles are the most effective sport program of lateral Epicondylitis treatment. The corticosteroid injection around tendon is used as a treatment but its long-time benefit is questionable.
New treatment methods include skin hypo tenotomy conducting by medical ultrasound, blood ethology transfusion and plasma transfusion enriched with platelet. Use of shock wave is also helpful in 48-73% of cases; otherwise, the degenerate tissue removal surgery can be influential in 85% of cases (Randall, 2011).
Methodology
In this study, all lateral Epicondylitis patients who visited physical clinic were examined. The patients suffering from romanticism diseases, cancer experience, diabetes, neuropathy or elbow fracture would be excluded from study. The informed consent was obtained from patients qualified for entry to the study. The criterion of lateral Epicondylitis diagnosis is localized pain of distal to Epicondylitis with approximate pressure of 4 kg. The pain intensifies with twist extension against resistance. (Walter, 2009). As said before, the population of this study was patients suffering from lateral Epicondylitis resistant to treatment visiting physical clinic of Baghi’at- Allah hospital (2012- 2013).the population size (n=120) was estimated with census method. The questionnaires and SPSS software were used for data gathering and data analysis, respectively.
Data analysis results
Results based on age groups
Table (1) frequency of lateral Epicondylitis patients based on age
| Age group | ||||
| 30-39 years | 40-49 years | 50-60 years | ||
| lateral Epicondylitis | positive | 23 | 58 | 48 |
| negative | 0 | 0 | 0 | |
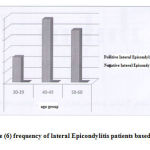 |
Figure 6: frequency of lateral Epicondylitis patients based on age |
Results based on gender
Table (2) frequency of lateral Epicondylitis patients based on gender
| Gender | Statistics | |
|
male |
Mean | 45.61 |
| N | 38 | |
| Median | 45.50 | |
|
female |
Mean | 46.48 |
| N | 91 | |
| Median | 47.00 | |
|
Total |
Mean | 46.22 |
| N | 129 | |
| Median | 47.00 | |
 |
Figure 7: mean and median based on gender |
Results based on occupation
Table (3) frequency of lateral Epicondylitis patients based on occupation
| occupation | ||||||
| employee | military | Housewife | ||||
| Count | Row N | Count | Row N | Count | Row N | |
| Positive lateral Epicondylitis | 39 | 30.2% | 35 | 27.1% | 55 | 42.6% |
| Negative lateral Epicondylitis | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
 |
Figure 8: Radiculopathy frequency in patients suffering from lateral Epicondylitis |
Discussion and results
The average of age for patients suffering from lateral Epicondylitis resistant to treatment is 45.6 years in men and 46.5 years in women; the total average is 46.2 years. This disease has the most frequency in age group of 40-49 years that is similar to results of previous studies. Women consisted majority of patients visiting clinic, particularly in morning shift; thus, most of patients under study are women but in general there is no difference between frequency of men and women suffering from lateral Epicondylitis.
Also, though majority of patients participating in this study are women but there is not a meaningful relation between Radiculopathy and gender of patients suffering from lateral Epicondylitis.
References
- Gary, s. firesterin. (2013). Kelleys text book of rheumatology, 9th
- Randall, L. (2011). Braddom/ physical medicine and Rehabilitation, 4th
- Aaron, l., Robinson, Md. (2010). Evaluating concomitant lateral Epicondylitis and cervical Radiculopathy. Journal of Musculoskeletal medicine.
- David, B. (2009). Genkins/Hollinsheads functional anatomy/.9th
- Walter, R. (2009). Frontra, gulie K. silver/ Essential of physical medicine and Rehabilitation 2vd edition.
- Richard, j. (2010).Wakefield/ Essential applications of musculoskeletal ultrasound in Rheumatology, 1st edition.







