T. Parthasaradhi1, Preethe Paddmanabhan2 and V. Ramya2
1Dept. Of Periodontics. Tagore Dental college and Hospital, Chennai. 2Department of Periodontics, Sree Balaji Dental College and Hospital, Bharath University, Pallikaranai, Chennai-600100
DOI : https://dx.doi.org/10.13005/bpj/702
Abstract
Guided bone regeneration (GBR) is a reconstructive procedure of alveolar ridge using membranes. Combining platelet-rich plasma (PRP) with bone graft materials has been advocated as a means of enhancing rate and quality of new bone formation in regenerative procedures. This procedure is indicated when there is no sufficient bone for implantation, or in the case of optimal implant installation for esthetic or functional needs. The aim of this case report was to evaluate the potential of PRP in combination with Demineralized bone matrix(DMBM) along with membrane to enhance bone regeneration in an siebert’s class III alveolar ridge defect .
Keywords
Guided bone regeneration; Platelet rich plasma; Alveolar ridge defect; Demineralized bone matrix
Download this article as:| Copy the following to cite this article: Parthasaradhi T, Paddmanabhan P, Ramya V. Successfull Localized Ridge Augmentation: A Combination Therapy Using Gbr and Prp. Biomed Pharmacol J 2015;8(October Spl Edition) |
| Copy the following to cite this URL: Parthasaradhi T, Paddmanabhan P, Ramya V. Successfull Localized Ridge Augmentation: A Combination Therapy Using Gbr and Prp. Biomed Pharmacol J 2015;8(October Spl Edition). Available from: http://biomedpharmajournal.org/?p=3515> |
Introduction
Adequate alveolar ridge is needed for a successful implant placement. Bone loss due to periodontitis or trauma causes resorption of the edentulous or partially edentulous alveolar ridge. Hence, to attain predictable long-term functioning and an esthetic treatment outcome, augmentation of an insufficient bone volume is often indicated prior to or in conjunction with implant placement1 Since with the presence of some limitations for an autograft like donor site morbidity, unpredictable resorption, limited quantities available, and the need to include additional surgical sites,2 alternative materials with different features have been developed instead of autografts.
Demineralized freeze-dried bone allograft (DFDBA), which is shown to be both osteoconductive and osteoinductive, has been used alone and in combination with other treatment modalities for periodontal therapy.3
PRP layer that is of interest for use in wound healing since this layer contains a concentrate of the patient’s platelets. These platelets have granules that contain growth factors that affect every cell and the formation of every tissue involved in the wound healing and regeneration of soft tissue and bone. Marx et al.4 first described the use of PRP in dental surgery. They claimed a radiographic maturation rate of bone grafts with PRP that was 1.62 to 2.16 times more rapid than grafts without PRP.
The growth factors within PRP like platelet derived growth factor (PDGFaa, PDGFbb, PDGFab), transforming growth factor beta (TGF-β1, TGFβ2), vascular endothelial growth factor (VEGF), epithelial growth factor (EGF), and insulin-like growth factor (IGF-1) These growth factors are thought to contribute to bone regeneration and increased vascularity, vital features of a healing bone graft.5
The recent randomized controlled clinical trial revealed that clinical and histologic findings had shown PRP enhanced bone regeneration in the platelet rich plasma assisted guided bone regeneration.6
The aim of this case report was to evaluate the potential of PRP in combination with bone xenograft along with membrane to enhance bone regeneration in an siebert’s class III alveolar ridge defect.
Case Presentation
A 35 years old female reported to the department of Periodontology and Implantology, Tagore Dental College, Chennai, complaining of replacement of missing teeth.
History revealed that the teeth 14,15,24, 25 & 26 was extracted due to grossly decayed, three years back and presence of spacing in relation to posterior aspect. The patient was using RPD and was insistent on its replacement with a fixed prosthesis.
On clinical examination, Seibert’s classification class – III in relation to 14 & 15 region and gingival recession in relation to 13 with a Clinical attachment level ((CAL) – Distance from the CEJ to the base of the sulcus) of 5mm. Inadequate alveolar ridge width of 4mm and height of 7mm. (Fig .1)
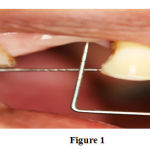 |
Figure 1: Pre-operative view of maxillary right premolar region (14, 15) shows 7 mm alveolar ridge defect. |
The treatment plan for the patient was to increase bone height and width by guided bone regeneration , followed by placement of an endosseous implant as a staged approach preparatory phase included full mouth scaling and polishing, 1 week prior to the surgery; followed by oral hygiene instruction.
Full thickness flap was raised by giving crestal incision palatally in the region of the missing tooth14,15 and continued by giving sulcular incision to the adjacent teeth for proper accessibility (Fig. 2 ). After complete debridement and isolation, defect was found to be of both horizontal and vertical pattern falling under Siebert’s Class III classification of volumetric deficit of bone and soft tissue within the alveolar process (Fig 3) A surgical burr was used to decorticate the bone in preparation for grafting (Fig 4). Briefly, prior to surgery, PRP was prepared following the protocol by Marx RE & Garg AK. 2005.7 10ml intravenous blood collected through a venepuncture in the antecubital vein was transferred to a test tube containing 1 ml of 10% trisodium citrate anticoagulant solution and centrifuged at 1200 rpm for 20 minutes, which resulted in two fractions.
 |
Figure 2: After giving crestal incision palatally in the region of the missing tooth 14,15 and continued by giving sulcular incision to the adjacent teeth |
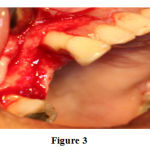 |
Figure 3: After raising Full thickness flap in relation to 14, 15 region and partial thickness flap in relation to 13 region revealing seibert class – III defect. |
 |
Figure 4: Decortcation of the bone using round burr |
The plasma, along with the top 2ml of red blood cells was again centrifuged at 2000 rpm for 15 minutes to get three basic fractions, platelet-poor plasma (PPP) at the top of the preparation (supernatant), platelet rich plasma (PRP) in the middle and the red blood cell fraction at the bottom. The top 80% fraction corresponding to PPP was aspirated with a pipette, leaving the residual (0.5 -2 ml) platelet concentrate (Fig 6). Then the coagulation of platelet rich plasma was obtained by adding 1 ml Batroxobin (Pentapharm) and 1 ml of 10% calcium gluconate (Medicos pharma). Within a few seconds a sticky gel consistency was obtained to be mixed with the bone graft and applied to the surgical site (Fig 7).
 |
Figure 5: Collagen membrane ??? |
 |
Figure 6: Freshly prepared platelet rich plasma. Defect on the mesial aspect of 21 grafted with DMBM /coagulated PRP mixture |
 |
Figure 7: Demineralized bone matrix combined with coagulated PRP prior to insertion into defect. |
DMBM (Osseograft, Advanced Biotech) and PRP mixture bone graft was placed into defect and care was taken not to overfill the defect and over the grafted area, resorbable guided tissue regeneration collagen membrane (Healigude, Advanced Biotech) was stabilized by giving periosteal suturing (Fig 8). Finally flap was closed by simple interrupted sutures (Figs 9) and periodontal dressing Coe-Pak was given over the surgical site Postoperative instructions were given and also adviced Amoxicillin (500 mg), three times daily for 5 days, and Ibuprofen (400 mg) thrice daily was prescribed for 3 days along with 10 ml of chlorhexidine (0.2%) mouthwash twice daily for 14 days. The patient was recalled after 1 week for suture removal. Healing was satisfactory with no postsurgical complications.
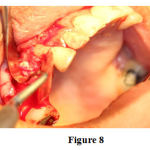 |
Figure 8: Defect in relation to 14 &15 grafted with DFDBA /coagulated PRP mixture along with stabilized membrane. |
 |
Figure 9: Flaps sutured with No.3-0 silk. |
She was recalled after 1 and 6 months for further evaluation and maintenance showing appreciable improvement in ridge both vertically as well as labiolingually. At 6 months postoperatively in the region of 14 and 15, clinical examination of the treated ridge defect showed significant improvement of alveolar ridge in both aspects of height and width of about 2.5mm and a gain in the clinical attachment level of about 3mm in relation to 13 compared to baseline values. (Fig 10).
 |
Figure 10: 2 years postoperative radiographic view of 21 region |
Discussion
The most commonly seen localized alveolar ridge defects are the combined Class III defects (56% of cases) followed by horizontal Class I defects (40% of the cases). Vertical defects were reported to be found in 4% of the patients.8 Large vertical and horizontal bone defects pose a prosthodontic challenge as it is difficult to restore esthetics and function along with the complete closure of the defect. Such clinical conditions are not successfully treated by conventional fixed or removable prosthesis alone.9 Guided bone regeneration can be successfully used in either a simultaneous approach or a staged approach.10
PRP, as used in this study, may affect the wound healing not only by a release of PGFs from platelets, but also because of other physical and chemical properties. The PRP preparation, because of its high fibrin content, presents a “sticky” characteristic that works as a hemostatic and stabilizing agent and may aid blood clot and bone graft immobilization in the defect area. Blood clot immobilization has been suggested as an important event in the early phases of wound healing in periodontal regenerative procedures.11 Studies proposed benefits of using PRP when combined with allografts results in dense and mature bone with better organized trabecular and greater bone regeneration with more rapid epithelization.12
Clinical studies evaluating the combination of PRP and bone grafts for GBR showed successful bone regeneration in the ridge defects.13,12,6 The collagen membrane has the ability to promote platelet aggregation, be chemotactic for fibroblast and enhance wound stability, required for proper healing. Even though lack of stiffness is drawback of collagen membranes but the studies have shown that space creation and maintenance are essential for periodontal regeneration.14 Bone replacement grafts have been advocated for maintaining space under membrane and providing osteoinductive and osteoconductive capacity. In our study, demineralized bone matrix was used instead of an osteoconductive material primarily due to its ability to stimulate progenitor cells to undergo differentiation to osteoblasts and form bone under the membrane
In this case, the combination of DMBM with PRP by making use of collagen membrane in GBR was sufficient to fill the alveolar ridge defect in width and length with predictable healing and improvement in clinical parameters which is suitable for implant placement.
Conclusion
This case demonstrates the successful augmentation of an atrophic, edentulous maxillary premolar using guided bone regeneration.
The use of a collagen membrane in conjunction with demineralized allograft Platelet rich plasma putty resulted in regeneration of vital bone of sufficient volume and density to accommodate a wide diameter implant.
References
- Buser D,Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: Anatomic and surgical considerations. Int J Oral Maxillofac Implants 2004;19(suppl): 43–61.
- Bell RB, Blakey GH, White RP, et al. Staged reconstruction of the severely atrophic mandible with autogenous bone graft and endosteal implants. J Oral Maxillofac Surg 2002; 60: 1135-41.
- Schwartz Z, Mellonig JT, Carnes DL Jr, et al. Ability of commercial demineralized freeze-dried bone allograft to induce new boneformation. J Periodontol 67:918–926.
- Marx R, Carlson ER, Eichstaedt RM, et al. Platelet Rich Plasma growth factors enhancement for bonegrafts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998; 85: 638-46.
- Aghaloo TL, Moy PK, Freymiller EG. Evaluation of platelet-rich plasma in combination with freeze-dried bone in the rabbit cranium. A pilot study. Clin. Oral Impl. Res. 16, 2005; 250–257.
- Eskan MA, Greenwell H, Hill M, Morton D et al., Platelet-rich plasma-assisted guided bone regeneration for ridge augmentation: a randomized, controlled clinical trial. J Periodontol. 2014 May; 85:661-8.
- Marx RE and Garg AK. Dental and craniofacial application of PRP 1st ed. Illinosis: Quintessence, 2005. p. 53-86.
- Abrams H, Kopczyk RA, Kaplan AL. Incidence of anterior ridge deformities in partial edentulous patients. J Prosthet Dent 1987; 57:191-194.
- Philip G, Dayakar MM, Gupta S, Khattri S. Preprosthetic soft tissue ridge augmentation using modified roll technique: a case report. Indian J Dent Sci 2013 Dec; 5:82-83.
- Buser D, Dula K, Belser U, Hirt HP, Berthold H. Localized Ridge Augmentation Using Guided Bone Regeneration: Surgical in the Maxilla. Int J Periodont Rest Dent 1993; 13:29-45.
- Wikesjo UME, Nilveus RE, Selvig KE. Significance of early healing events on periodontal repair. A review. J Periodontol 1992; 63:158-165.
- Sanchez AR, Sheridan PJ, Kupp LI. Is PRP a perfect enhancement factor? A current review. Int J Oral Maxillofac Implants. 2003;18:93-103
- Yasushi NakajimaJoseph P. Fiorellini, David M. Kim et al., Regeneration of standardized mandibular bone defects using expanded polytetrafluoroethylene membrane and various bone fillers. Int J Periodontics Restorative Dent 2007; 27:151–159.
- Haney JM, Nilveus RE, McMillan PJ, Wikesjo UM. Periodontal repair in dogs: Expanded polytetrafluoroethylene barrier membranes support wound stabilization and enhance bone regeneration. J Periodontol. 1993;64:883–90.








