Roya Islamzadeh1, Fatima Rashid Sheykhahmad2,* and Sonia Hosseini Anbaran1
1Department of Medical, Ardabil Branch, Islamic Azad University, Ardabil, Iran 2Young Researchers and Elite club, Electronic Branch, Islamic Azad University, Tehran, Iran
DOI : https://dx.doi.org/10.13005/bpj/847
Abstract
Non-tumoral skin lesions include several lesions such as eczema, hives, Psoriasis and Lichen-Planus. In this study we review under biopsy lesions in Imam Khomeini Hospital Pathology Clinic. In this study we review the medical files for 866 skin patients. Data analysis showed that there is no relation between the age (p=0.446) and gender (p=0.247) of the patients and their disease. The results also showed that eczema and Liechen-Planus are among non-infectious erythematous us diseases and vesiculobullo us is the most common non-tumoral diseases that get biopsy. Bottom is the most prone part the body.
Keywords
Skin lesions; Biopsy; Tumoral; and Pathology
Download this article as:| Copy the following to cite this article: Islamzadeh R, Sheykhahmad F. R, Anbaran S. H. Study of Non-Tumoral Skin Lesions (Among Patients who visited Imam Khomeini Hospital Pathology Clinic). Biomed Pharmacol J 2015;8(2) |
| Copy the following to cite this URL: Islamzadeh R, Sheykhahmad F. R, Anbaran S. H. Study of Non-Tumoral Skin Lesions (Among Patients who visited Imam Khomeini Hospital Pathology Clinic). Biomed Pharmacol J 2015;8(2). Available from: http://biomedpharmajournal.org/?p=3863 |
Introduction
Non-tumoral skin lesions include several lesions such as eczema, hives, Psoriasis and Lichen-Planus.
Eczema is a chronic allergic skin disease. This skin disease is usually seen in head, face, neck, elbow or knee. The disease can start when you are one month or one year old. The disease will ease when you are three but can toll again at any age. Different kinds of eczema include: Atopic Eczema, which is seen in people prone to allergy and especially among infants; Discoid Eczema, is characterized by round spots of oozing or dry rash, with clear boundaries, often on lower legs. The cause is unknown, and the condition tends to happen to adults; Contact eczema or dermatitis, resulting from direct reaction to a detergent, the symptoms includes
Intense itching in the infected area, small blisters in the infected area that usually is
Followed by releasing some liquid from the wound, skin thickening and dandruff due to the chronic swelling (12).
Liechen-planus is a chronic inflammatory idiopathic disease than engages both skin and Mucous membrane. This is a both acute and chronic disease with unknown cause and resistant toward cure. Many studies have shown a relation between the disease and Helicobacter pylori infection, though some other studies have rejected the relation (108).
Hives are acute or chronic allergic reactions that appear as small pink spots or even sometimes as blisters along with intense itching. Hives usually happen due the reaction of our body toward Histamines or Histamine-like combinations. Among the triggers of hives we can name nuts, chocolates, fish, tomatoes, eggs, strawberries, milk, food essence, and fresh fruits especially citrus and drugs such as antibiotics as Penicillin, pain killers, Codeine, Indomethacin, sleeping pills, Vitamins and almost any other drugs. Continuous usage of Aspirin can also cause hives (11).
Psoriasis is a self-immune chronic skin disease. The problem happens when the immune system of the body sends some false signals and the signals make the skin cells grow faster; one the symptoms of the disease is nail engagement in various kinds (7, 9).
Studying non-tumoral skin lesions among the visiting patients in Imam Khomeini Hospital
Pathology Clinic during 2004 to 2012
Hypothesis
Erythematosus \ Makulopapular \ Squamous Cell Carcinoma (SCC) are among most common skin disease.
Vesiculobullous, Vesicles and Pustules are among most common skin diseases. Skin Pigmentation Disorder is less epidemic among patients.
Subcutaneous fat inflammatory diseases are not common among the patients.
Bottom is most common area for the diseases.
Research methodology
This is a descriptive-analytic periodical study.
Research location
The chosen location is Imam Khomeini Hospital Pathology Clinic.
Population and sample size
The population includes patients who suffered skin diseases and visited Imam Khomeini Hospital Pathology Clinic during 2004-2012.
In this study the patients are studied respectively as they visited the clinic.
Data collection methodology
In this study we first chose all the patients who underwent biopsy in the past 9 years in Imam Khomeini Hospital Clinic. And then exclude all the patients with tumoral lesions. Next, we extracted the data from the patients’ medical files (including age, gender and disease) and inserted it to the analyzing software.
The Variables
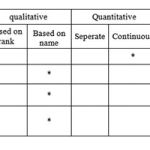 |
Table 1 |
The Patients Genders
In this study we analyzed the medical files for 866 patients suffering skin lesions. The results showed that among them 452 (52.19 percent) were women (Graph 1).
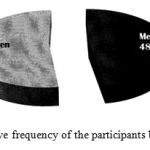 |
Figure 1: Relative frequency of the participants based on gender |
Patients Age
The age of the patients were also studied. The data analysis showed that the medium of the patient’s age is between ±16.81 and 38.4. Also most of the patients were between 30 to 40 years old (Graph 2).
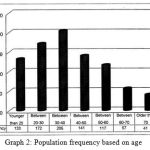 |
Figure 2: Population frequency based on age |
The Infected Area
The location of the lesion has also been studied. The analysis showed that bottom with 211 cases (24.36 percent) has been the most common area (Graph 3).
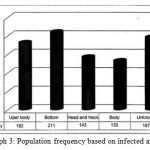 |
Figure 3: Population frequency based on infected area |
The patients visiting time
The year when the patients had visited the clinic was also studied. The analysis showed that in 2012 with 181 patients (20.90 percent) the Pathology clinic was most visited (Graph 4).
 |
Figure 4: Population frequency based on the visiting time |
Non-infectious diseases of Erythematosus \ Makulopapular \ Squamous Cell
Carcinoma (SCC)
The study also included Erythematosus \ Makulopapular \ Squamous Cell Carcinoma (SCC) diseases. The results showed that 325 patients (37.52 percent) were categorized in this set, among which Liechen-Planus with 153 cases (17.55 percent) was the most common disease (Graph 5).
 |
Figure 5: Population frequency based on non-infectious Erythematosus \ Makulopapular \ Squamous Cell Carcinoma (SCC) diseases |
Skin – Vascular diseases
The study examined the diseases with vascular causes and it was proved that 41 patients (4.75 percent) suffered skin lesions with vascular causes, among which leukocytoclasis Vasculitis with 21 cases (2.42 percent) was the most common disease (Graph 6).
 |
Figure 6: Population frequency based on skin vascular diseases |
Non-infectious Vesiculobullous, Vesicles and Pustules diseases
This group included 226 patients (26. 09 percent). In this group we can name Dermatitis Eczematous, Pemphigus, Pemphigoid, Vesiculobullous dermatitis (dermatitis herpetiformis) and Vesicles- Pustules dermatitis (Erythema Multiforme), among which Eczema with 159 case was the most common disease (Graph 7).
 |
Figure 7: Population frequency based on non-infectious Vesiculobullous, Vesicles and Pustules diseases |
Eczema (Dermatitis)
Since the diseases categorized under eczema title seem important and with high frequency, in this study we also analyzed the disease and found out Eczematoid dermatitis to be the most common (Graph 8).
 |
Figure 8: Population frequency based on Eczema |
Connective tissue diseases
After we examined the biopsy of the patients with Connective tissue disease, which included 145 patients (16.7 percent), we found out that the most common kind was chronic cutaneous lupus Erythematosus (DLE) with 87 patients (Graph 9).
 |
Figure 9: Population frequency based on connective tissue disease |
Epidermal inflammatory diseases
In this study we also analyzed epidermal inflammatory diseases and the result showed that among 54 patients (6.23 percent), Pilaris keratosis was the most common (Graph 10).
 |
Figure 10: Population frequency based on epidermal inflammatory diseases. |
Inflammatory lipid sub transcutaneous diseases
After the data was analyzed we found out that 16 patients (1.84 percent) were suffering inflammatory lipid sub transcutaneous diseases (Graph 11).
 |
Figure 11: Population frequency based on inflammatory lipid sub transcutaneous diseases |
Skin Pigmentation diseases
Skin Pigmentation includes Vitiligo and hyperpigmentation after inflammation; the result of the analysis showed that 16 patients (1.84 percent) were suffering the disease (Graph 12).
 |
Figure 12: Population frequency based on skin Pigmentation diseases |
Other Disease Groups
The other groups of the patients suffered from Histiocytosis (Cerebrotendinous), Skin toxicity caused by drugs, non-infectious Granulomatous (Granuloma Annulare), Degenerative disorder (solar Elastose), metabolic skin diseases (lichen amyloidosis) and physical disorders. The data analysis revealed that 43 patients (4.96 percent) were categorized in this group (Graph 13).
 |
Figure 13: Population frequency based on other group diseases |
The Relation Between Age and Skin Pathology
In this study we analyzed patients with common pathology and skin diseases based on age. The results showed that there is no correlation between patients ages and skin pathology (p=0.446). The data analysis was implemented using ANOVA
(Table 1-4).
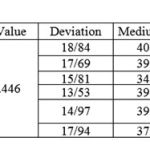 |
Table 2 |
The relation between gender and skin pathology
After we analyzed the data using Chi-Square test we found no meaningful correlation between patients gender and their skin diseases (p=0.247) (Table 2-4).
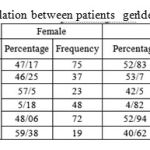 |
Table 2-4: The correlation between patients gender and skin pathology |
The Debate
In this study we analyzed 866 patients with skin lesion diseases, out of which
52.19 percent were women and their medium age was 38.47±16.81 years. Bottom with 24.36 percent was the most common infected area. In this study also 37.52 percent of all the lesions were non-infectious Erythematosus \ Makulopapular \ Squamous Cell Carcinoma (SCC) diseases, among which Liechen-Planus (17.66 percent in total and 47.07 percent in the group) was the most common. About
26.09 percent of the skin lesions were comprised of non-infectious Vesiculobullous, Vesicles and Pustules diseases, among which Eczema (18.36 percent in total and 70.35 percent in the group) was the most common. Moreover,
16.7 percent of the skin lesions were recorded to be connective tissue diseases with DLE being the most common one (10.04 percent in total and 60 percent in the group). This is while, 6.23 percent of the skin lesions were epidermal inflammatory diseases with Pilaris keratosis being the most common disorder (2.77 percent in total and 44.44 percent in the group). Almost 1.84 percent of all the skin lesions were inflammatory lipid sub transcutaneous diseases with Erythema-Nodosum being the most common (1.83 percent in total and 75 percent in the group). On the other hand, 1.84 percent of the skin lesions were skin Pigmentation diseases with hyperpigmentation being the most common (1.61 percent in total and 87.5 percent in the group). And finally, 4.96 percent were related to the other groups among which Granuloma Annulare was the most common (1.96 percent in total and 39.53 percent in the group).
Significantly, the data analysis showed that there is no correlation between the patients age and skin pathology (p=0.446) nor their gender (p=0.247).
This is while, Tusi et al (5) in their study on over 450 patients, who were the personnel of a hospital, found that 44 percent of the studied population suffered Contact Dermatitis.
Conclusion
This study showed that Eczema from non-infectious Vesiculobullous, Vesicles and Pustules diseases and Liechen-Planus from Erythematosus \ Makulopapular \ Squamous Cell Carcinoma (SCC) diseases were the most common non-tumoral skin lesions that have undergone biopsy.
In this study we found that patients with Hives or Eczema visit Clinics less and their disease is usually cured through explanation and self-cure rather than biopsy.
Bottom proved to be the most common infected area in the patients.
Reference
- Saeed, Sadia, Connie A. Keehn, and Michael B. Morgan. “Cutaneous metastasis: a clinical, pathological, and immunohistochemical appraisal.” Journal of cutaneous pathology6 (2004): 419-430.
- Bénet, Claire, et al. “Histologic and immunohistologic characterization of skin localization of myeloid disorders a study of 173 cases.” American journal of clinical pathology2 (2011): 278-290.
- Tanière, Ph, et al. “Lymphomatoid granulomatosis–a report on four cases: evidence for B phenotype of the tumoral cells.” European Respiratory Journal1 (1998): 102-106.
- Bittencourt, Achiléa L., et al. “Adult T-Cell Leukemia/Lymphoma in Bahia, Brazil Analysis of Prognostic Factors in a Group of 70 Patients.” American journal of clinical pathology5 (2007): 875-882.
- Rush, Walter L., et al. “Pulmonary pathology of Erdheim-Chester disease.” Modern Pathology7 (2000): 747-754.
- Topaz, Orit, et al. “Absence of intraepidermal glycosyltransferase ppGalNac-T3 expression in familial tumoral calcinosis.” The American journal of dermatopathology3 (2005): 211-215.
- Topaz, Orit, et al. “Mutations in GALNT3, encoding a protein involved in O-linked glycosylation, cause familial tumoral calcinosis.” Nature genetics6 (2004): 579-581.
- Perrin, C., et al. “Multicentric Reticulohistiocytosis: Immunohistological and Ultrastructural Study: A Pathology of Dendritic Cell Lineage.” The American journal of dermatopathology5 (1992): 418-425.
- Haroche, Julien, et al. “Dramatic efficacy of vemurafenib in both multisystemic and refractory Erdheim-Chester disease and Langerhans cell histiocytosis harboring the BRAF V600E mutation.” Blood9 (2013): 1495-1500.
- Ruiter, Dirk J., et al. “Pathologic staging of melanoma.” Seminars in oncology. Vol. 29. No. 4. WB Saunders, 2002.
- Bonnier, Pascal, et al. “Inflammatory carcinomas of the breast: a clinical, pathological, or a clinical and pathological definition?.” International journal of cancer4 (1995): 382-385.
- Ingen-Housz-Oro, Saskia, et al. “IgG4-related skin disease successfully treated by thalidomide: a report of 2 cases with emphasis on pathological aspects.” JAMA dermatology6 (2013): 742-747.
- Seeger, Leanne L., et al. “Tumoral calcinosis-like lesion of the proximal linea aspera.” Skeletal radiology8 (1990): 579-583.
- Hammoud, Sommer, Edward F. McCarthy, and Kristy Weber. “Tumoral calcinosis in infants: a report of three cases and review of the literature.” Clinical orthopaedics and related research 436 (2005): 261-264.
- Chojniak, Rubens, et al. “Computed tomography guided needle biopsy: experience from 1,300 procedures.” Sao Paulo Medical Journal 124.1 (2006): 10-14.







