P.Shanmuga Priya* and K. Balasubramanian Kabali
Stanley Medical College,Chennai. Tamilnadu. India.
DOI : https://dx.doi.org/10.13005/bpj/620
Abstract
Diabetes mellitus mainly type II is due to resistance to insulin action. The hyperglycemia casued by diabetes lead to micro and macrovascular complication that endangers with life. Premenopausal women with diabetes had the risk similar to that of men with diabetes. Due to reduced estrogen hormone deficiency postmenopausal diabetic women had additional risk . To compare the frequency domain analysis of heart Rate Variability between premenopausal and postmenopausal known diabetic females. 60 Type II diabetic females around the age of 40- 5yrs (both pre and postmenopausal) from diabetic OPD were recruited from Stanley Medical College Hospital. Institutional Ethical committee approval was obtained. After obtaining written and informed consent from the subjects. ECG(LEADII)was recorded for five mintues in supine position using RMS Digital Polyrite.HRV analysis was done using Frequency domain methods using RMS Digital Polyrite software version 2.1. Our study indicates that there is a lower HRV in postmenopausal known diabetic females when compared to that of premenopausal known diabetics. Further, decline in estrogen level and diabetes gives a additional risk of increased sympathovagal balance in postmenopausal diabetic women. Type II postmenopausal diabetic females have increased level of autonomic dysfunction .Hence they require hormonal replacement therapy, regular periodic evaluation of cardiac autonomic status in order to prevent future cardiovascular morbidity and mortality.
Keywords
Diabetes Mellitus; Heart Rate Variability; Premenopausal and postmenopausal ageing; ostrogen
Download this article as:| Copy the following to cite this article: Priya P.S, Kabali K. B. Heart Rate Variability Analysis Between Premenopausal and Postmenopausal Known Diabetics: A Comparative Study. Biomed Pharmacol J 2015;8(1) |
| Copy the following to cite this URL: Priya P.S, Kabali K. B. Heart Rate Variability Analysis Between Premenopausal and Postmenopausal Known Diabetics: A Comparative Study. Biomed Pharmacol J 2015;8(1). Available from: http://biomedpharmajournal.org/?p=1749 |
INTRODUCTION
Diabetes Mellitus is a group of common metabolic disorders that share the phenotype of hyperglycemia.The metabolic dysregulation associated with diabetes mellitus causes secondary pathophysiological changes in multiple organ system that impose a tremendous burden on the individual with diabetes and on the health care system1.With evolving trend across worldwide, Diabetes Mellitus will be a leading cause of mortality and morbidity. The worldwide prevalence of Diabetes Mellitus has risen drastically over past two decades, from an estimated 30 million cases in 1985 to 285 million in 2010.In individuals aged more than 65 years ,the prevalence was 26.9%. Worldwide estimates project that in 2030 shows that the greatest number of individuals with Diabetes will be aged 45-64 years1. Diabetic Autonomic Neuropathy (DAN) is among the most recognized and silent complications of diabetes, in the face of its significant harmful impact on survival and quality of life in people with diabetes2 DAN may be either clinically evident or subclinical3 Reduced heart rate variability is the earliest indicator of CAN4.
MATERIALS AND METHODS
60 Type II Diabetic females around the age of 40-65yrs(both pre and postmenopausal) from diabetic OPD with duration of diabetes of 3-10 yrs with Random Blood Sugar ≥ 200 mg/dl or Fasting Blood Sugar ≥ 126 mg/dl were recruited from Stanley Medical College Hospital. Institutional Ethical committee approval was obtained. After obtaining written and informed consent from the subjects ECG(LEADII)was recorded for five mintues in supine position using RMS Digital Polyrite. HRV analysis was done using Frequency Domain methods using RMS Digital Polyrite software version 2.1.
Exclusion Criteria
Subjects with a history of asthma, hypertension , cardiovascular disease and those on chronic medication .
Experimental Protocol
The short term Heart rate variability recording is usually performed for research , clinical investigations and followed the procedure given in the Task-Force report on Heart Rate Variability subjects were instructed to avoid heavy physical activity and also instructed to retrain from all caffeinated beverages for 12 hours prior to research activity. All the study subjects and controls have a prestructed proforma completed .Subjects were screened after measuring height,weight,blood pressure.The basal recording of blood pressure was done using sphygmomanometer by standard Riva Rocci method. Ask the subjects to lie down comfortably in the supine position in the Neuro physiology lab ,Department of Physiology,Stanley Medical Collage.(5 mints rest). Placed the ECG electrodes on the limbs of the subjects and connect the leads to the machine for lead II ECG recording. Transfer the data from RMS Polyrite to window based PC loaded with software for Heart rate variability.Removed ectopics and artifacts from the recorded ECG.Extracted the R-R tachogram from the edited 256 –second ECG using the R wave detector in the Acq Knowledge software and saved it in the ASCII format which is later used offline for short –term HRV analysis. Performed HRV analysis using the HRVanalysis software version 2.1(Biosignal Analysis group,Finland). Mean R-R is measured in second(s).Variance, defined as power in a portion of the total spectrum of frequencies, is measured n milliseconds squared(ms2).Mean R-R is measured in seconds .
Parameters studied
Spectral indices (LF ms2,HF ms 2 , LF/HF ratio) are calculated.
Statistics
Data are expressed as mean ± SD .Data between the study groups were compared using unpaired Student t-test. Differences were considered statistically significant at (P<0.05). The collected data was analysed with SPSS 16.0 version.Data were normally distributed based on the Kolmogorov-Smirnov Z test for normality.To describe about the data mean and S.D was used. To find the significant difference between the Patients and controls Independent t-test was used.
RESULTS AND DISCUSSION
Diabetes Mellitus is characterized by hyperglycemia mainly in Type II diabetes due to reduced action of insulin (Insulin resistance)1. It is the major cause for cardiovascular morbidity and mortality. The main advantage of using frequency domain analysis of Heart rate variability is that one can study the signal’s frequency-specific oscillations.Thus both the amount of variability and the oscillation frequency(number of heart rate fluctuations per second) can be obtained. Spectral analysis involves decomposing the series of sequential R-R intervals into a sum of sinusoidal functions of different amplitudies and frequencies by the FFT algorithm. . The LF fluctuations are predominantly under sympathetic control with vagal modulation, whereas the HF fluctuations are under parasympathetic control5. Three main spectral components are distinguished in a spectrum calculated from short-term recordings of 2 to 5 minutes6,7,8,9,10 : VLF, LF, and HF components. Frequency domain analyses contributed to the understanding of autonomic background of RR interval fluctuations in the heart rate record.11,12Silent ischemic heart disease or cardiac arrhythmias have both been invoked as contributors to sudden death. In Asymptomatic Diabetics (DIAD) study of 1123 patients with type 2 diabetes, cardiac autonomic dysfunction was a strong predictor of ischemia. Results from the European Diabetes Insulin-Dependent Diabetes Mellitus (IDDM) Complications Study showed that patients with impaired HRV had a higher corrected QT prolongation than without this complication Cardiac autonomic neuropathy (CAN), which can be documented by abnormal heart rate variability (HRV), occurs commonly in patients with diabetes and is associated with silent myocardial ischemia6 and increased mortality7, In a recent large meta-analysis, Maser et al. reported that the presence of cardiac autonomic neuropathy was associated with a greater than threefold increase in mortality and sudden death7.. Autonomic imbalance between the sympathetic and parasympathetic nervous systems regulation of cardiovascular function contributes to metabolic abnormalities and significant morbidity and mortality for individuals with diabetes.8-10The presence of CAN was associated with a greater than threefold increase in mortality and sudden death. Silent ischemic heart disease or cardiac arrhythmias have both been invoked as contributors to sudden death. Meta-analyses of published data demonstrate that reduced cardiovascular autonomic function as measured by heart rate variability (HRV) is strongly associated with an increased risk of silent myocardial ischemia.s9,15 Regular HRV testing provides early detection and thereby promotes timely diagnostic and therapeutic interventions. HRV was found to be an independent predictor of all-cause mortality during a period of 9 years, in a population-based study using Cox proportional hazard models. Moreover, the Hoorn study by Gerritsen et al demonstrated that impaired autonomic function is associated with increased all-cause and cardiovascular mortality and that CAN in patientsalready at risk (diabetes, hypertension, or history of CVD) may be especially hazardous Clinical manifestations of cardiovascular autonomic dysfunction (e.g., exercise intolerance, intraoperative cardiovascular liability, orthostatic tachycardia and bradycardia syndromes, silent myocardial ischemia) can result in life-threatening outcomes10-14
Table 1: Subjects Characteristics, Anthropometric Measures
| Parameter | Mean | SD | t value | p value | |
| BMI | Pre | 31.6 | 39 | 1.01 | 0.317 |
| Post | 24.4 | 1.6 | |||
| SBP (mmHg) | Pre | 120.2 | 6.8 | 7.11 | 0.00 |
| Post | 131.3 | 5.2 | |||
| DBP (mmHg | Pre | 74 | 5.0 | 7.649 | 0.00 |
| Post | 82.3 | 3.3 | |||
No significant difference between pre and postmenopausal study subjects compared to premenopausal diabetics,postmenopausal diabetics had lower estrogen level,lower HF,Higher LFand high LF/HF ratio.
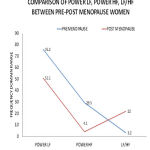 |
Chart: Comparison Of Heart Rate Variability Parameters Between Premenopausal and Postmenopausal Women |
Table 2: Frequency Domain Analysis oh heart rate variability
| Mean | SD | t value | p value | ||
| Pm2LF | Pre | 1083.9 | 153.8 | 3.417 | 0.002 |
| Post | 3245.5 | 555.2 | |||
| Pm2HF | Pre | 474.2 | 211.5 | 11.884 | 0.00 |
| Post | 189.5 | 179.7 | |||
| LF/HF | Pre | 3.2 | 1.1 | 19.307 | 0.00 |
| Post | 22.0 | 5.2 | |||
CONCLUSION
The postmenopausal women had a significantly reduced overall fluctuation in autonomic input demonstrated by lower HF, increased LF ,HF ratio in postmenopausal diabetic suggests that more sympathetic dominance.Therfore my study suggests that decline in levels of estrogen from pre to postmenopausal makes shift of autonomic balance towards the sympathetic dominence. Type II postmenopasual diabetic females have increased level of autonomic dysfunction .Hence they require hormonal replacement therapy, regular periodic evaluation of cardiac autonomic status in order to prevent future cardiovascular morbidity and mortality.
REFERENCES
- Harrison’s Principles Of Internal Medicine-18th Edition (page2868-3003).
- Vinik AI, Erbas T. Recognizing and treating diabetic autonomic neuropathy. Cleve Clin J Med.2001; 68: 928- 944.
- American Diabetes Association and American Academy of Neurology. Report and recommendations of San Antonio Conference on diabetic neuropathy (Consensus Statement). D iabetes . 1988; 37: 1000- 1004.
- Maser R, Lenhard M, De Cherney G. Cardiovascular autonomic neuropathy: the clinical significance of its determination. Endocrinologist. 2000; 10: 27-33.
- Rodica Pop-Busui, MD, PHD,1 Gregory W. Evans, MA,2 Hertzel C. Gerstein, MD, MSC,3 Vivian Fonseca, MD,4 Jerome L. Fleg, MD,5 Byron J. Hoogwerf, MD,6 Saul Genuth, MD,7 Richard H. Grimm, MD, PHD,8 Marshall A. Corson, MD,9 Ronald Prineas, MD,2,* and the ACCORD Study Group Diabetes Care. 2010 July; 33(7): 1578–1584. 6. Sayers BM. Analysis of heart rate variability. Ergonomics. 1973;16:17-32
- Hirsh JA, Bishop B. Respiratory sinus arrhythmia in humans: how breathing pattern modulates heart rate. Am J Physiol. 1981;241:H620-H629. Akselrod S, Gordon D, Ubel FA, Shannon DC, Barger AC, Cohen RJ.
- 8..Power spectrum analysis of heart rate fluctuation: a quantitative probe of beat to beat cardiovascular control. Science. 1981;213:220-222.
- Pagani M, Lombardi F, Guzzetti S, Rimoldi O, Furlan R, Pizzinelli P, Sandrone G, Malfatto G, Dell’Orto S, Piccaluga E, Turiel M, Baselli G, Cerutti S, Malliani A. Power spectral analysis of heart rate and arterial pressure variabilities as a marker of sympathovagal interaction in man and conscious dog. Circ Res. 1986;59:178-193.
- Malliani A, Pagani M, Lombardi F, Cerutti S. Cardiovascular neural regulation explored in the frequency domain. Circulation. 1991;84:1482. predictor of mortality after an acute myocardial infarction.
- Pomeranz M, Macaulay RJB, Caudill MA, Kutz I, Adam D, Gordon D, Kilborn KM, Barger AC, Shannon DC, Cohen RJ, Benson M. Assessment of autonomic function in humans by heart rate spectral analysis. Am J Physiol. 1985;248:H151-H153.
- Pagani M, Lombardi F, Guzzetti S, Rimoldi O, Furlan R, Pizzinelli P, Sandrone G, Malfatto G, Dell’Orto S, Piccaluga E, Turiel M, Baselli G, Cerutti S, Malliani A. Power spectral analysis of heart rate and arterial pressure variabilities as a marker of sympathovagal interaction in man and conscious dog. Circ Res. 1986;59:178-193.
- Ziegler D, Zentai CP, Perz S, Rathmann W, Haastert B, Doring A, Meisinger C.: Prediction of mortality using measures of cardiac autonomic dysfunction in the diabetic and nondiabetic population: the MONICA/KORA Augsburg Cohort Study. Diabetes Care 2008; 31: 556–561.
- Ferrani AU, Radaelli, Centola M. Ageing and the cardiovascular system. J Appl Physiol 2003;95: 2591–2597.
- Bannister R. Autonomic failure. A textbook ofclinical disorder of autonomic neuropathy. OxfordUniversity







